Complementary and integrative health (CIH) is an important aspect of Whole Health. CIH approaches are fundamental elements of “Well-Being Programs,” which are, in turn, a key part of a Whole Health System (Figure 1). Patients, including Veterans, pay a lot of money out of pocket for these approaches. Based on supportive research findings and expert consensus, the VA has mandated that all sites will now cover a number of these approaches in some form as part of Veterans’ benefit packages (for more information refer to “Complementary and Integrative Health Approaches in the VA: A Glossary and Where You Can Learn More” tool).
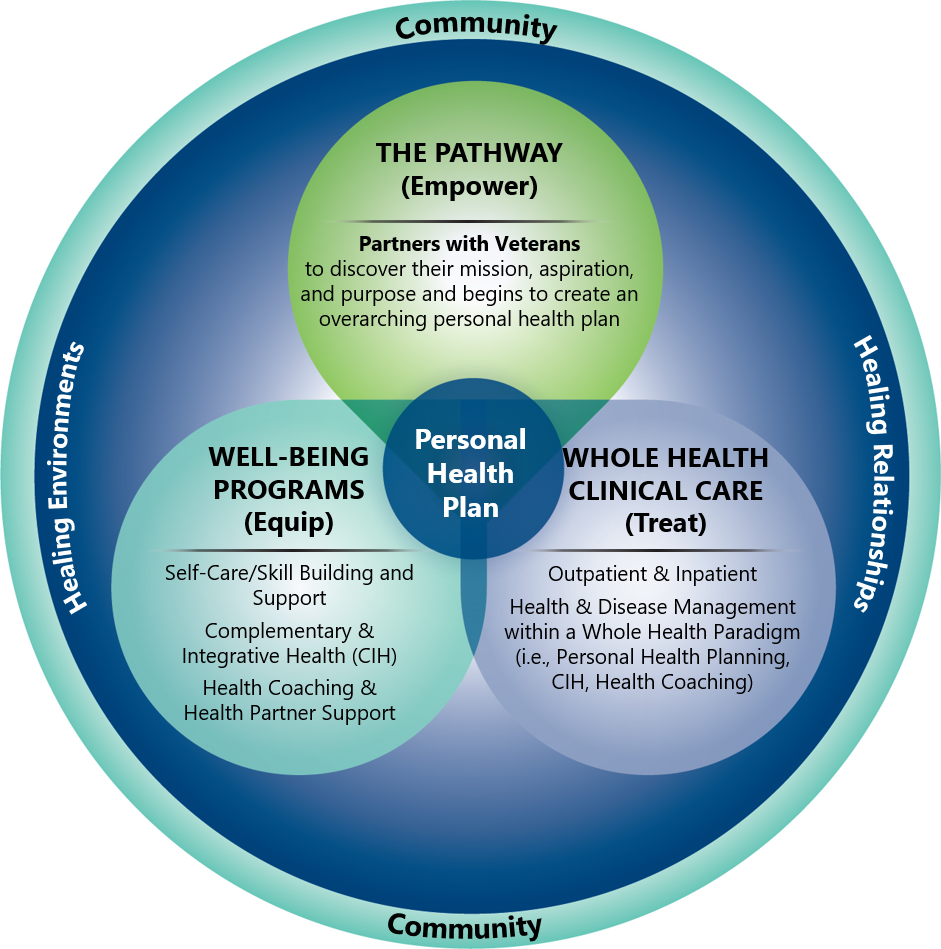
Figure 1. Key Elements of the Whole Health System
Key Points
- CIH can come up in a number of ways during Whole Health visits. As a care team member (e.g., a clinician or a Whole Health Coach), you may wish to suggest certain approaches, and at other times you may be advising against them. The key, regardless of your opinion on a given approach, is that you can have a helpful conversation about these modalities with your patients.
- Keep the ECHO criteria (Efficacy, Costs, Harms, Opinions) in mind as you discuss CIH with patients.
- Always remember to ask people where they are getting their information about CIH. Become more familiar with those sources of information yourself. Ask your colleagues where they are getting their information about CIH, particularly if they have particularly strong feelings and you are curious as to why.
- Know who offers CIH at your VA site and in your community, and learn more about their qualifications and skill sets. Firsthand experience is always best, so it may be worth arranging to visit them yourself.
- There are reputable online resources for many CIH resources, such as mindfulness and tai chi. The VA Integrative Health Coordinating Center (IHCC) and your Field Implementation Team (FIT) Consultant can help you find more information.
Introduction
Even though CIH is receiving more attention and gaining in popularity, most clinicians have limited training about how to incorporate them into practice. This overview is designed to provide some guidance with that. It features three Veteran narratives, each designed around common scenarios you may encounter when exploring how CIH might fit into a Veteran’s Personal Health Plan (PHP). These three patients include:
- Lee, a healthy 34-year-old body builder who wants to optimize his self-care practices and prevent future health issues.
- Frederick, a 56-year-old gardener with a number of chronic problems. He is a big fan of supplements and wants advice about them.
- Annie, a 70-year-old nurse who tries to manage her care almost exclusively with CIH approaches.
These narratives become progressively more complex. You may find it helpful to review just one of them and then return to the others at a different time.
The Veteran narratives go over some important aspects of how to advise patients regarding use of several widely-used dietary supplements, including multivitamins, ergogenic aids (supplements taken to enhance athletic performance), anti-inflammatories, and adaptogens (supplements to improve immunity and resilience to stressors). Several useful CIH resources are featured, including the Integrative Medicine textbook, the Natural Medicines website, the National Library of Medicine site, and various materials available on the Whole Health website. The textbook and Natural Medicines site are available to all VA clinicians through the VHA National Desktop Library Whole Health Subject Guide. The others can be accessed online from anywhere.
The narratives also focus on a variety of other CIH therapies, in addition to dietary supplements. VHA’s Provision of Complementary and Integrative Health (Directive 1137). features two lists of CIH services.[1,2] List 1 includes approaches that have evidence of promising or potential benefit and are required to be offered by all VA facilities or their community partners, if those approaches are part of a Veteran’s treatment plan. List 2 includes approaches that VA facilities have the option of offering. They are generally considered safe, even if evidence for their use is less clearly supportive than for the approaches on List 1. Many of the approaches on List 1 and List 2 are featured in the three Veteran narratives. For more information about Lists 1 and 2, refer to Integrative Health Coordinating Center Approved List of CIH. The approaches on each List 1 and 2 are highlighted in the next section of this overview.
CIH Fundamentals
The philosophies of one age have become the absurdities of the next, and the foolishness of yesterday has become the wisdom of tomorrow.
–William Osler, MD
Before reading this overview, you are encouraged to review Chapter 14 of the Passport to Whole Health, entitled “Introduction to Complementary and Integrative Health Approaches.” That chapter defines CIH and provides a background on use of CIH in the VA. It describes the work of VA’s Integrative Health Coordinating Center (IHCC) and introduces the “Spectrum of CIH” and the ECHO criteria as well. Those tools are used to create PHPs for the Veteran narratives featured below.
The Passport to Whole Health also introduces the 5 general categories of complementary approaches. Various sections of the Passport to Whole Health discuss the various CIH approaches in each category in more depth. If you are curious about a given category, note the following:
- Chapter 4, “Mindful Awareness” covers a number of mindful awareness exercises, and Chapter 12, “Power of the Mind,” explores 10 different mind-body approaches.
- Chapter 5, “Moving the Body,” discusses yoga, tai chi, and qi gong.
- Chapter 15, “Biologically-Based Approaches: Dietary Supplements,” provides key information on dietary supplements, including how to read supplement labels and issues related to supplement safety.
- Chapter 16, “Manipulative and Body-Based Practices,” has information on massage, osteopathy and chiropractic care.
- Chapter 17, “Energy Medicine: Biofield Therapies” introduces approaches like Healing Touch, Reiki, and Therapeutic Touch, among others.
- Finally, Chapter 18, “Whole Systems of Medicine” introduces Chinese medicine (with a special emphasis on acupuncture) and naturopathy. It also provides some details about homeopathy and Ayurveda.
- Note too that each of the “Professional Care” overviews on the Whole Health website also feature CIH research that is relevant for specific conditions.
Here are some highlights to remember as you make your way through the Veteran narratives in this overview.
- While these vignettes are couched in the conventional model of having one clinician gathering data and making recommendations, the truth is that Whole Health requires a full team, and everyone who a Veteran encounters in his/her care is ideally a team member. How can responsibilities be divided, so that no one clinician feels overwhelmed?
- Many Veterans use, or are interested in, CIH.
- It is important that you have a sense of your personal beliefs about these approaches and that you can provide informed advice to people about their use.
- Be especially familiar with the approaches on List 1, described above. These include acupuncture, therapeutic massage, tai chi, qi gong, yoga, meditation, guided imagery, biofeedback, and clinical hypnosis.
- It is also useful to know what approaches are on List 2. These include acupressure, Alexander Technique, animal-assisted therapy, aromatherapy, biofield therapies, Emotional Freedom Technique, Healing Touch, reflexology, Reiki, Rolfing, Somatic Experiencing, Therapeutic Touch, and Zero Balancing. (If any of these are unfamiliar, see the Whole Health Tool, “Complementary Approaches in the VA: A Glossary of Therapies and Whole Health Resources for Learning” There is a process for VA employees to petition to have additional approaches added to List 2. To make a request for an approach to be added, email the OPCC&CT Integrative Health Coordinating Center: vhaopcctintegrativehealth@va.gov
- ECHO (Efficacy, Costs, Harms, Opinions) can be a useful tool when you are deciding whether or not to use a given CIH approach.
Part of working with CIH is dealing with the differences of opinion that inevitably come up when complementary approaches are discussed. For that, it might be helpful to read the Whole Health tool, “How Do You Know That? Epistemology and Health.”
Meet the Veteran: Lee
Lee is a 34-year-old Operation Enduring Freedom Veteran and former Marine. He recently enrolled in the VA, after hearing that the VA is beginning to cover CIH approaches. Lee prides himself on being healthy. A dedicated body builder, he is a semiprofessional kickboxer who also works as a personal trainer at a local health club. Overall, he is quite healthy, aside from occasional shoulder and wrist pain that flares up after he lifts weights. His father died of a myocardial infarction (MI) at the age of 52, and he wants to do all he can to avoid having the same thing happen to him.
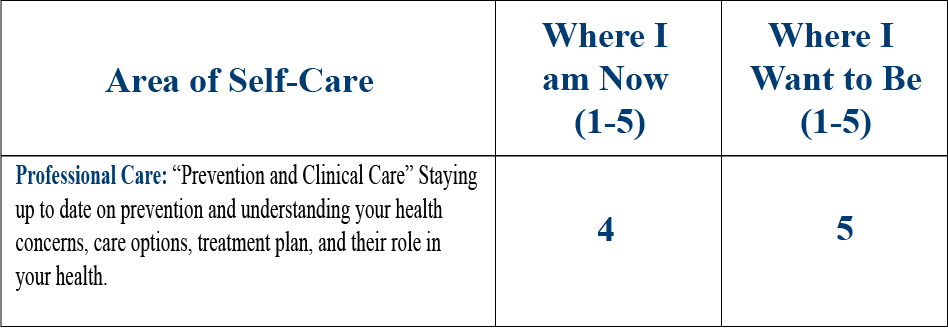
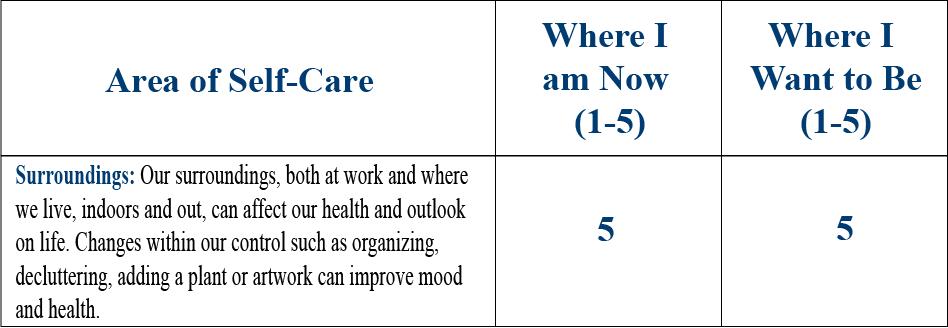
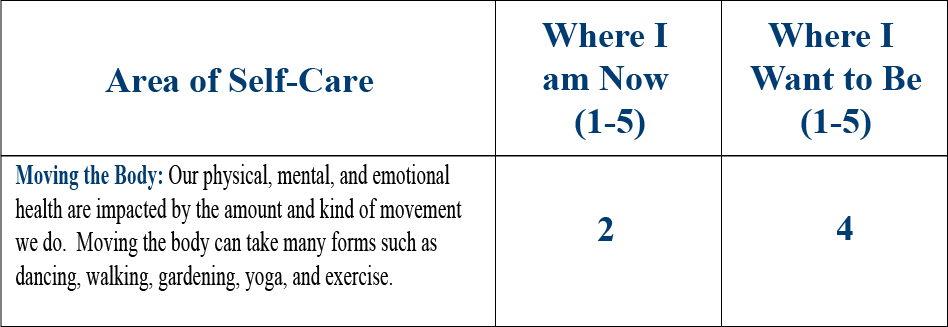
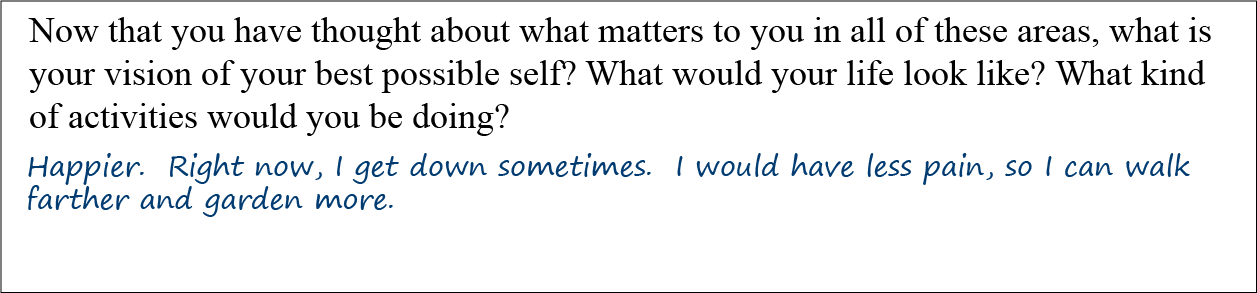
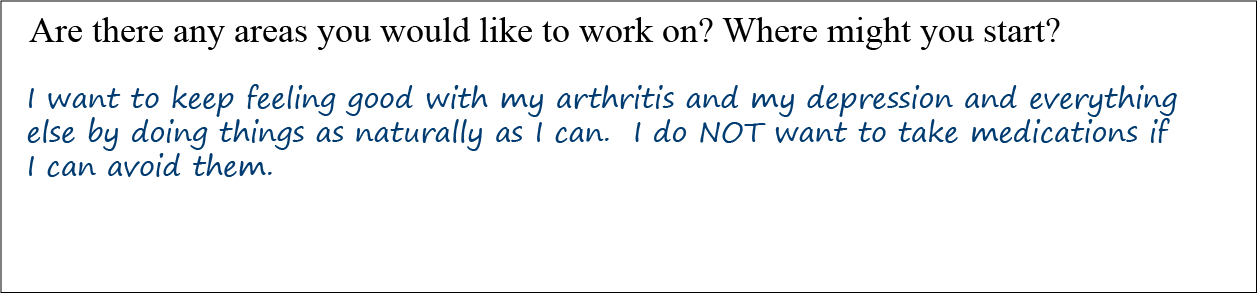
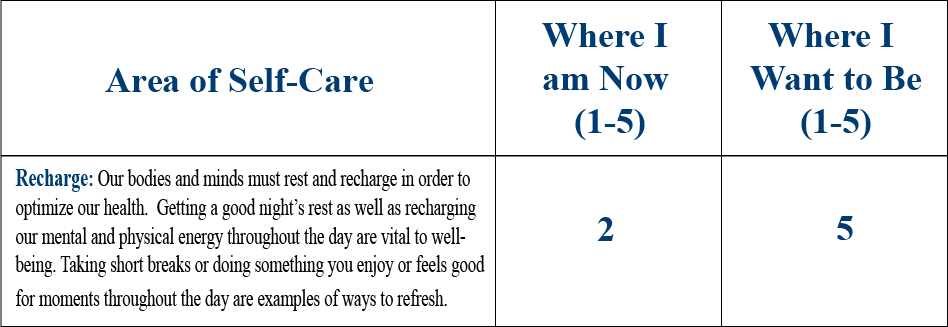
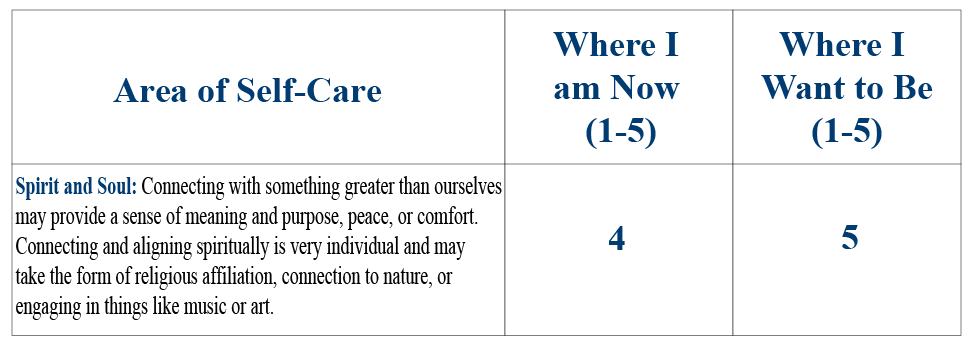
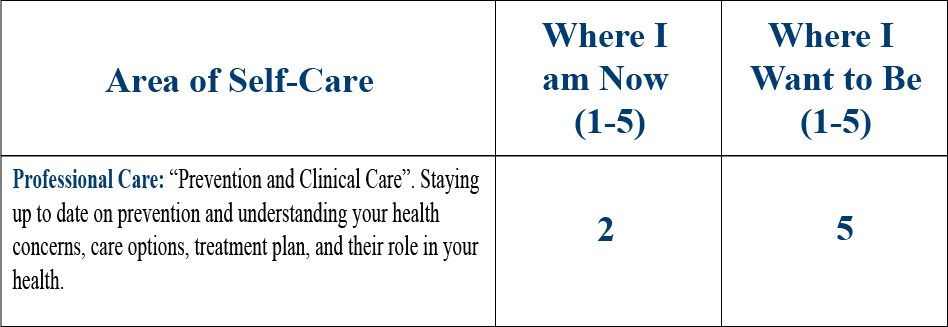
Lee completes his Personal Health Inventory (PHI), and it is striking how well he is doing overall with his self-care. None of his clinicians feel he is rating himself more highly than he should; he is incredibly fit, seems quite happy, and has an almost contagious excitement when he talks about being healthy. Some highlights are:
Lee gives himself 5/5 on all the Vitality Signs (physical health, mental health, and how it is to live his life).
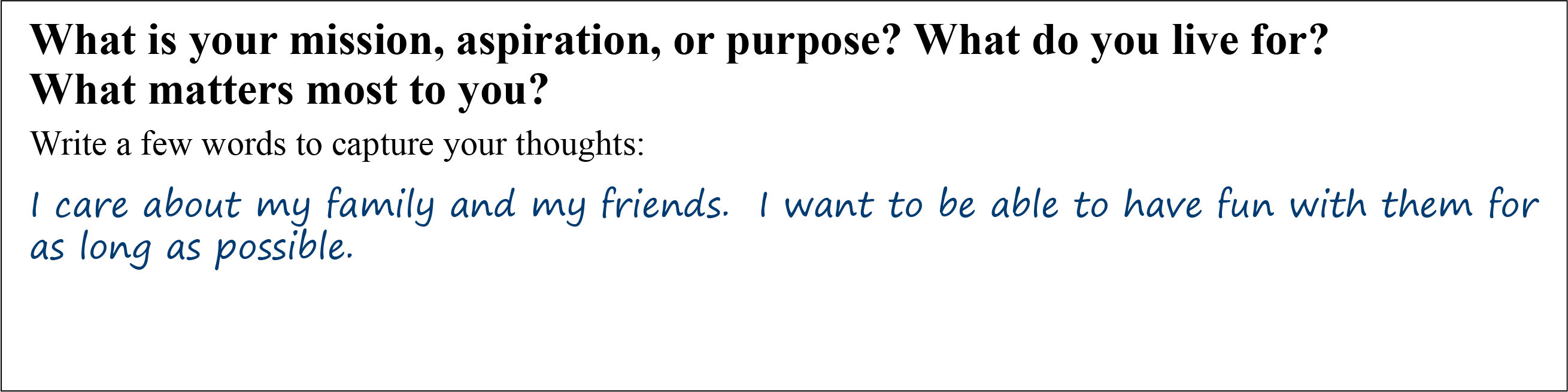
When asked, “What do you live for? What matters to you? Why do you want to be healthy?” Lee answers:
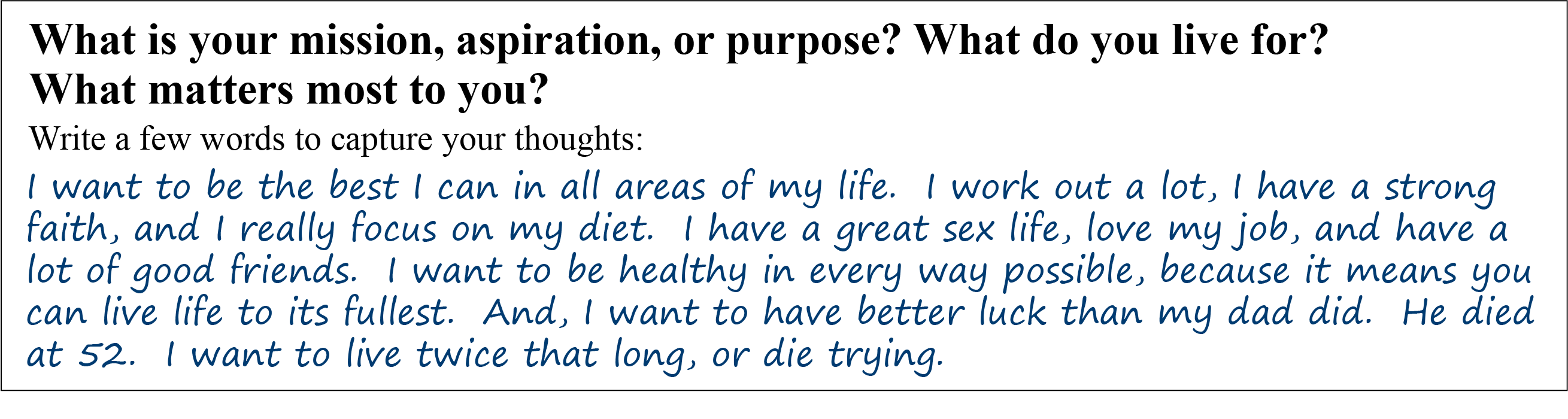
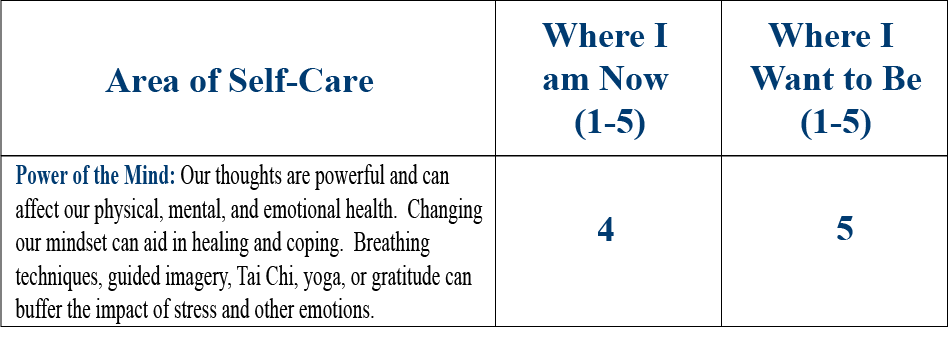
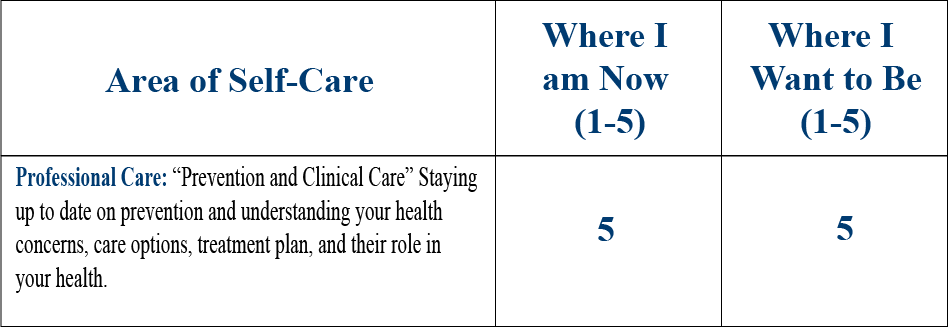
He gives himself a 5 out of 5 on all the self-care and professional ratings on the second page of the PHI, except for Power of the Mind, where he rates himself a 4 out of 5. He is up to date with all his Professional Care, and he reports no high-risk behaviors.
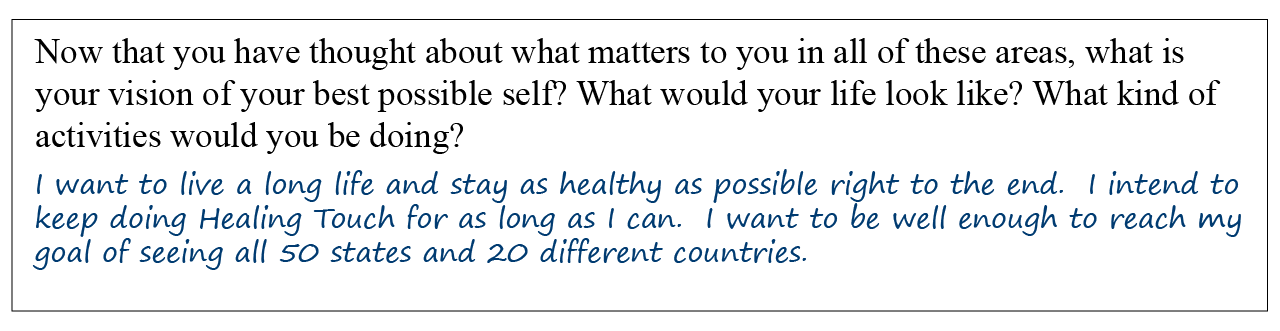
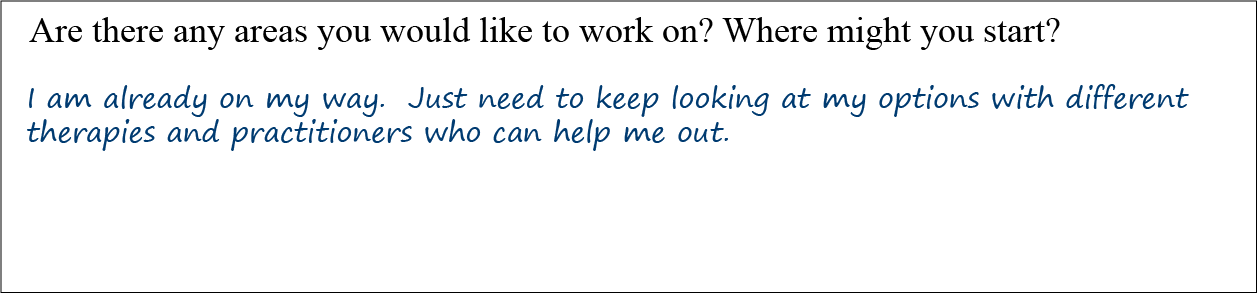
Lee’s answers to the reflections questions offer a strong sense that he is interested in CIH:
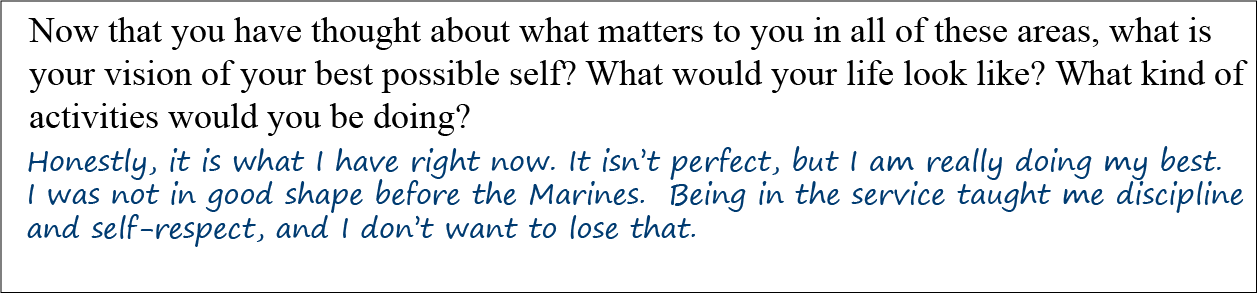
During the first part of his clinical visit, Lee elaborates some more.
- He exercises at least 2 hours daily, 6 days a week.
- He has a girlfriend, also a kickboxer. He plans to propose to her sometime in the coming year.
- He is taking fish oil supplements, whey protein, creatine, and a multivitamin. He adds wheat grass to his smoothies and also eats a few protein bars a day.
- His diet is nutrient dense, with lean meats, plenty of fruits and veggies, reasonable amounts of fiber, and limited junk food.
Lee seems friendly, earnest, and a bit intense. He is clearly very open-minded about CIH (which is particularly common for many OEF/OIF Veterans[3] and for Veterans in general[4]). It is clear he is worried about having a heart attack at a young age like his father.
Mindful Awareness Moment
Mindful Awareness Moment
Now that you have read about Lee, what do you notice in terms of your own feelings and judgments? Do you like Lee? Do you think you can help him? Are there any aspects of his care where you feel particularly confident? Where you feel uncertain?
Lee’s primary concern is well-being. He has a few health concerns, but his main goals are to optimize his health and prevent future problems. Do his goals strike you as unusual, compared to your typical clinic visits? Which CIH approaches might be useful for Lee? What other suggestions would you make to him, based your initial impressions?
Lee: CIH Options
In considering how to discuss CIH with Lee, it can help to consider each of the 5 different CIH categories, one at a time. Each one can be assessed using the ECHO criteria. Lee’s clinician decides to do this with an eye to the latest research findings available on PubMed, which is part of the National Library of Medicine website administered by the National Institutes of Health (NIH).
1. Biologically-Based Approaches for Lee
Lee is taking whey protein and creatine, which are ergogenic supplements. That is, they are designed to support body-building and athletic performance. He is also taking fish oil, 2 gm daily, and adding wheat grass to his diet. He pays $60 per month for his multivitamin but wonders if he needs it.
Whey Protein. Lee’s clinician does a quick PubMed search using the search term “whey protein,” as illustrated in Figure 2. Her search yields thousands of results. By sorting findings according to “Best Match” she finds an article entitled, “Supplemental Protein in Support of Muscle Mass and Health: Advantage Whey.”[5] The abstract notes that “…whey protein has been found to stimulate muscle protein synthesis to a greater degree than other proteins such as casein and soy.” It also notes that higher-protein diets do indeed promote gains in muscle mass with resistance training.
To read in more depth, Lee’s clinician narrows the search. She uses “whey protein supplementation” as a search term and selects additional criteria in the column on the left side of the page. (Refer to the screen capture, Figure 3, below.) Under “Article types,” she selects “Review” and “Systematic Review.” She chooses “5 years” to narrow down the search in terms of “Publication dates,” and she selects “Humans” under “Species” to exclude animal studies.” 25 articles were found. If a more detailed search were needed, she could also have selected “Show additional filters” and chosen “Languages” (to review only articles in English) or other “Search Fields.”
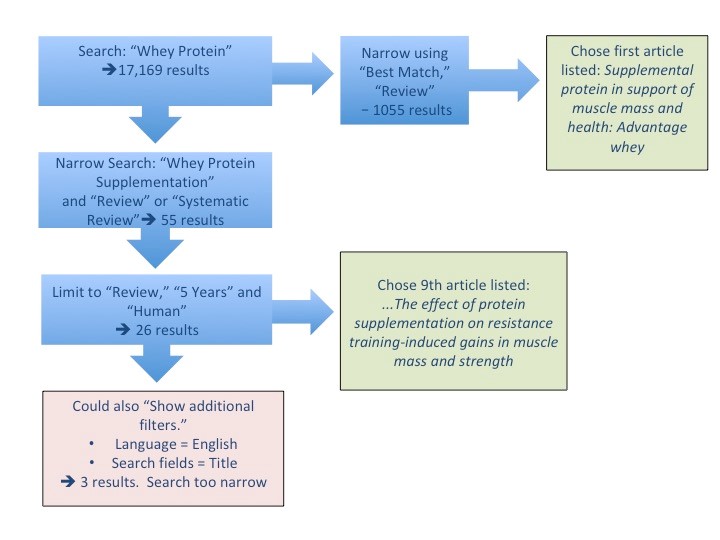
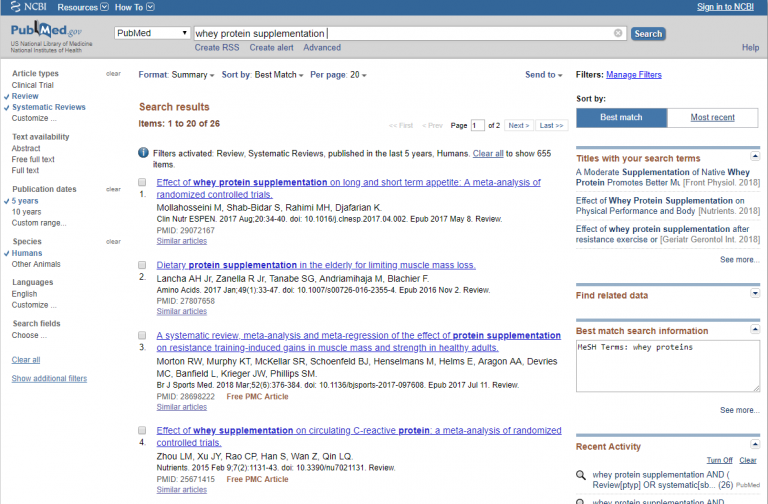
One of the articles with the most potential is a 2018 article entitled “A systematic review, meta-analysis, and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults.” It reports that protein intakes at amounts greater than 1.6 gm/kg per day do not lead to any additional muscle mass gains with resistance training, which is useful information to guide Lee in terms of his questions about protein “dose.”[6]
When “Whey Protein Safety” is searched, no concerning articles come up, and one article even notes that the “Whey2Go” randomized controlled trial found whey protein lowers blood pressure and improves lipids and endothelial function in people with mild hypertension.[7] In other words, whey protein may offer Lee the additional benefit of lowering his cardiovascular risk. Of course, it is important to remind Lee that simply eating high-protein foods in general could suffice. He can get protein not only through meat, but through a number of plant sources as well.
Creatine. Creatine (as opposed to “creatinine”) is naturally found in muscle cells and helps them produce energy during exercise via ATP production. There are many theories regarding its mechanism of action, but how it works is not completely clear.[8] A 2018 review that came up after a search of “Creatine Supplementation” concluded that it is safe and “effective for particular settings” such as short-duration, high-intensity resistance training.[9] Most creatine studies have only been done short term, however. It is not clear that creatine helps people do better in sports. Overall, it seems to be safe for short-term use, though it should not be used in high doses in people with renal conditions.[10]
Fish oil. Lee read that fish oil could prevent heart attacks, and since his father had one at such an early age, he figures it is worth it for him to take. He chose to take fish oil supplements instead of eating fish, because the fish oil in capsules is micro-distilled, which means it has less heavy metal content than the fish themselves.
In a PubMed search, Lee’s clinician found one 2017 review that concludes there are cardiovascular disease (CVD) benefits of fish oil, and specifically the benefits of the omega-3 fatty acid docosahexaenoic acid (DHA), are heavily dependent on dose.[11] However, a 2018 meta-analysis that included nearly 78,000 people for an average of 4.4 years did not find benefits of taking approximately 1 gm daily of omega-3s for any subgroups. Lee is currently not taking the 500 mg of total DHA that previous studies recommend, so even if the 2018 study is not taken into account, he is probably not taking enough fish oil to get much benefit.
In terms of fish oil safety, while there is some concern about doses of 2-15 gm of combined omega 3s causing increase bleeding risk, the European Food Safety Authority has not found that doses of fish oil under 5 gm have ever caused bleeding problems. In general, side effects of omega-3 supplements are mild and mostly tie into dyspepsia and related symptoms.[12]
After discussing where the research stands, Lee decided to keep taking his fish oil, recognizing that while it was not clear how much it would help him prevent heart disease, he also wanted to take it for its other potential benefits, such as effects on inflammation in general and on mood, especially since he has not experienced any adverse effects while taking it.
Wheatgrass. Searches on PubMed for “Wheat grass,” “Wheat grass supplementation,” or even the Latin name, “Triticum aestivum,” are not revealing in terms of using wheatgrass as a dietary supplement. However, the term “wheatgrass” as a single word provided a few useful studies. One 2017 trial found that wheatgrass supplementation at 3.5 gm daily for 10 weeks resulted in improved lipid panels in a group of 59 women with hyperlipidemia.[13] A 2015 review noted a gap between basic science (in vitro) findings, which show that wheatgrass may be helpful for cancer prevention and as an antioxidant, versus human studies which to date do not show evidence of clinically significant benefits, largely because the research simply has not been done today.[14] Fortunately, wheatgrass seems to be quite safe.
Multivitamins. Many people take multivitamins, but it is not clear that they are beneficial. The Physicians’ Health Study II trial did not find that daily multivitamins reduced cardiovascular events, heart attacks, stroke, or cardiovascular mortality over 10 years.[15] It is not clear that a multivitamin would benefit someone like Lee, who has a healthy diet rich in fruits and vegetables (not to mention vitamin-fortified protein bars which he eats daily). Fortunately they tend not to be associated with adverse events,[10]
For many patients, it can be helpful to check for drug-supplement or supplement-supplement interactions. While Lee is not taking medications, this still worth considering. Refer to the resources in Chapter 15 of the Passport to Whole Health for more information.
2. Manipulative and Body-Based Practices for Lee
Lee notes that he has pain in his right shoulder, left wrist, and sometimes his lower back after a day where he does heavy lifting. He also has significant muscle soreness after a kickboxing tournament. Lee might benefit from therapeutic massage, which may be available as part of his VA benefits package, or from manual therapy, such as chiropractic. He may also benefit from yoga, which can serve as a great complement to his intense fitness routine and has shown promise for health issues such as low back pain. Refer to the Whole health tool, “Yoga: Looking Beyond the ‘Mat’,” as well as Chapter 16 of the Passport to Whole Health for more information on the benefits of massage and manual therapy.
3. Energy Medicine.
Research is limited, but many energy medicine studies report decreased stress levels and increased energy in people who receive treatments, regardless of their underlying diagnoses. (Refer to Chapter 17 in the Passport to Whole Health for more information and for a research summary.) This is an option that could be considered, but Lee does not have a strong interest in it at this time.
4. Whole Systems of Medicine
Chinese medicine, Ayurveda, and other healing systems emphasize prevention of disease versus merely treating it after it arises. However, in the U.S., it is more common for these sorts of CIH approaches to be used for treatment, rather than prevention. It would be worth discussing these with Lee to gauge his interest. Acupuncture, which is one of several interventions used in Chinese medicine, might help with his muscle pain. There is increasingly strong evidence favoring its use for low back pain and other pain problems (refer to Chapter 18 in the Passport to Whole Health, as well as the Whole Health website for materials on pain), but it may be that Lee would prefer to start with massage, for which there is less research but also a suggestion of potential benefits, as outlined in Chapter 16 of the Passport to Whole Health.
5. Mind-Body Approaches
It is striking that the only self-care circle in the PHI that Lee gave himself less than a 5 out or 5 on was Power of the Mind. When asked to elaborate, Lee explains that he would like to be “more focused,” and that he needs to “slow down and catch a breath” more often. He feels like his workouts are a good chance to focus his mind, which is why he spends a lot of time exercising. He is not sure he could do a seated meditation, “the more my body slows down, the more my mind speeds up.”
Lee’s Personal Health Plan: Prevention and Focus
As he reviews the different areas of the Circle of Health with his clinician, Lee notes he wants to focus first on Professional Care. Who can help him optimize his health and help him keep his heart healthy? A few discussion topics and suggestions come up during his visit:
- Lee’s clinician acknowledges his strengths, including his commitment to wellness, his level of physical fitness, and his willingness to keep exploring options.
- Lee is asked to focus more on why he wants to be “at his best.” What does it allow him to do? How does it shape his future? He tells his clinician that his dream is to be an athletic trainer for a college sports team, and to eventually marry and have children. He does not want to be like his dad, who “always watched us play as kids, but never joined in.” He wants to be a triathlete, but says he has to get better at swimming before he can do so.
- He is pushing his body hard with his workouts and kickboxing. He is asked to consider whether or not he might be over-training. Can he cross-train in a way that would be less likely to cause the chronic muscle soreness? Lee is not willing to work out less. He believes a lot of the pain actually comes from the kickboxing, and he does not consider it to be a problem, so much as a natural consequence of doing what he enjoys.
- Massage therapy is certainly reasonable to help with his sore shoulder, low back, and other areas. He is given information about options. It is not clear that the VA will cover this on an ongoing basis.
- He could benefit from bringing in mind-body approaches.
- This includes doing a body scan exercise once a day. This might be one way to help him be more focused. He is interested in learning more, and he is willing to meet with someone who can teach him how to do a body scan and other meditation exercises. Lee is given a copy of the “Body Scan” tool from Chapter 4 of the Passport to Whole Health, as well as links to some of the online guided meditation resources listed at the end of the chapter.
- If Lee finds the body scan helpful, his clinician will discuss the possibility of taking a meditation class with him at a future visit. Lee is given the Whole Health Veteran Handouts, “An Introduction to Mindful Awareness” and “Seated Meditation.”
- His clinician gently reminds him that often the people who benefit most from such practices are those who say their mind just “doesn’t slow down that way,” as Lee put it. It is similar to working out— you do not expect to be as strong as you want when you are first beginning. Practice is required.
- As Lee’s provider gets to know him more, the intent will be to talk more about his stress levels. Lee claims he manages stress, but this is not conveyed in his body language. His blood pressure is slightly elevated, and various options for managing this (medications, stress reduction, and dietary changes, for example) will be broached when he sees his primary care provider next time. It will be important to talk more with him about his experiences in the military as well; for instance, are his stress and overactive mind tied to trauma he suffered during service? Often Veterans do not see this correlation. (For more information on options, refer to “Hypertension” on the Whole Health website.)
- In terms of dietary supplements, Lee seems to be doing relatively well. All of his supplements are reasonable to take, but some of the following changes could be beneficial:
- He understands that his fish oil may not be as helpful as he hoped, and he could consider stopping it in the future. His clinical team reminds him that he is doing a great job as far as overall risk factors and lowering his risk with many of his lifestyle choices.
- He will continue the whey protein, recognizing that protein from food in general might be another good option
- He is interested to hear about research findings indicating creatine mainly helps resistance training in the short term. He will try going off creatine for a couple of weeks to see if he notices a difference.
- He likes and plans to continue the wheatgrass, recognizing it is likely safe even though little is known about efficacy.
- On reflection, he feels he is getting enough nutrients through his diet and his protein bars. He will stop his expensive multivitamin.
- Lee is happy to have his lipids checked, along with a few other He is reassured that he is already doing many positive behaviors that his father did not do (e.g., his father struggled with obesity and smoked 2 packs a day) and this reduces Lee’s chances of having an MI at a young age. His clinician offers him the chance to talk with a mental health provider more about his fears of dying young like his father did. He says he will consider it.
- Lee will follow up in 4-6 weeks with one of the nurses on the team with an update on how he is doing. He will come in for a blood pressure check in 3 months; it is clear that the slight elevation caught his attention.
Lee’s choices around his CIH care are summarized in Table 1.
Table 1. A Summary CIH-Related Elements of Lee’s Personal Health Plan (PHP)
| Element of PHP | Research Support (+, +/-, or -) | Comments |
|---|---|---|
| Whey Protein | + | Consider protein via food too. |
| Creatine | +/- | Will do a trial without |
| Fish oil | - | Wants to continue despite data |
| Wheatgrass | +/- | Safe, he prefers to take |
| Multivitamin | - | Will stop |
| Therapeutic Massage | + | Will give it a try |
| Yoga | + | Less enthused, but will consider |
| Acupuncture | + | Will try if massage not helpful |
| Stress management | + | Important to clinician, who wants to explore his mental health further |