Background
Note: The terms atopic dermatitis and eczema are used interchangeably in this document and refer to chronically itchy and inflamed skin, which may be accompanied by hay fever and/or asthma.
Atopic dermatitis is a chronic and relapsing dermatitis that typically shows up during infancy or early childhood. It affects 5%-20% of the childhood population around the world. Atopic dermatitis appears increasingly common and is more prevalent in developed countries and in urban locations. Eczema is grouped into three age categories: infantile, childhood, and adult. In infants, the face and extensors are typically involved. Childhood and adult eczema tends to affect the flexural areas and is characterized by more chronic inflammation with dry, scaly, thickened skin. People with eczema typically have a lower tolerance for skin irritants. Heat and perspiration are the most common offenders with wool and emotional stress close behind.
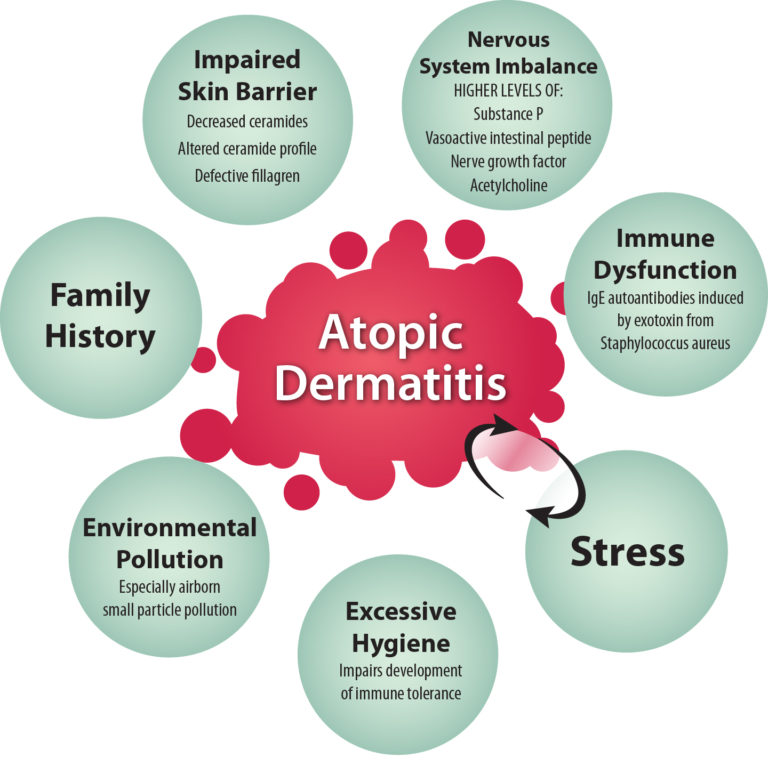
There are many factors at play in the development of eczema. Family history (especially maternal history) is a strong predictive risk factor, but there appear to be many environmental factors as well, including insufficient exposure to microorganisms in early childhood and excessive exposure to airborne pollution.[1][2] People with eczema have problems with their skin barrier, which puts them at risk for increased evaporation of moisture from the skin and decreased ability to maintain skin moisture. They also have an increased risk of developing skin infections due to bacteria, viruses, and fungus. The superficial cutaneous nervous system in people who have atopic dermatitis is hyper-reactive as well, and people with atopic dermatitis are more likely to experience the sensation of itch.
Along with the physical symptoms of this condition, atopic dermatitis carries a significant emotional burden. People with atopic dermatitis have been found to have a significantly decreased quality of life and self-esteem, as well as increased sleep disturbances, depression, and anxiety.[3] The fact that stress worsens symptoms of atopic dermatitis[4] can result in a downward spiral with stress from the atopic dermatitis worsening the flare, which can worsen stress.
Treatment
Skin Care
Adequate skin hydration is the most basic aspect of care for both the prevention of eczema flares and for treatment of active disease. This begins with minimizing contact with irritantsincluding hot water. Both frequency and duration of bathing should be limited, and the lowest water temperature tolerable should be used. Generous amounts of thick cream or ointment should be applied to the skin immediately after bathing while the skin is still slightly damp. A good rule is to look for an emollient that is scooped from a tub or squeezed from a tube (a cream or ointment). Creams that contain ceramides (which are deficient in eczematous skin) can be especially helpful. Specific products that can be purchased over the counter include Aveeno Eczema Therapy, Cetaphil, Curel, and CeraVe. Soaps should be pH neutral. Specific brands include Dove, Earth Friendly, Pears natural glycerin soap, Clearly Natural glycerin soap, and South of France glycerin soap. Caution should be taken with personal care products that contain fragrances because these can be irritating.
Food & Drink
While it seems to make sense that following an anti-inflammatory diet would help minimize the effects of an inflammatory condition of the skin, there have been few studies looking specifically at this issue. Indeed, there is strong evidence that this dietary approach can positively affect other systemic inflammatory conditions, but research looking at anti-inflammatory diets in people with eczema is limited. One study looking at maternal adherence to a Mediterranean diet and infant wheeze and atopic dermatitis in the first year of life did not find any correlation.[5] Researchers from the International Study of Allergies and Asthma in Childhood (ISAAC)a large multicounty, multiphase cross-sectional studyfound a positive correlation between severe eczema and fast food consumption three or more times per week in children (6-7 years) and adolescents (13-14 years). They also found a protective effect with high fruit consumption.[6]
A group of researchers in India looked at 148 adult patients with atopic dermatitis who followed a hypoallergenic diet for three weeks and found significant improvement in parameters of atopic dermatitis.[7] This diet was very restrictive and included only gluten-free foods, potatoes, rice, chicken, beef, pork, thermally modified fruits, and vegetables (excluding parsley and celery). Participants were only allowed to drink plain water, mineral water, or black tea, and all seasonings were avoided.[7] The research group recommended short term use of the hypoallergenic diet to identify whether or not food allergies play a role in specific patients atopic dermatitis before focusing on a more typical elimination diet. This study suggests that food sensitivities may play a role in adult eczema as well.
Although information about diet for atopic dermatitis is limited, its overall safety and benefits in other inflammatory conditions is reassuring. It is reasonable to offer information about an anti-inflammatory dietary approach to patients with eczema. A three-week trial of a hypoallergenic diet or trying an elimination diet may also help some people with eczema. To learn more, refer to The Anti-Inflammatory Diet Tool. Chapter 8 of the Passport to Whole Health.
Tea
One study looked at 118 people with recalcitrant atopic dermatitis who drank Oolong tea daily for six months. Ten gm of dried tea leaves were steeped for 5 minutes in 1,000 gm boiling water and divided into 3 cups and consumed after each meal. After one month, a marked (>50%) or moderate (25-50%) improvement of the dermatitis was seen in 64% of participants. This was based on comparison between photographs and pruritus intensity.[8] This effect was postulated to be due to the polyphenol content of the tea. While this is promising, more studies will be necessary to clarify the role of tea consumption in atopic dermatitis. Nonetheless, this is a very safe and worthwhile recommendation.
Food Allergies
The issue of food allergies as triggers for flares of eczema can be confusing, since food allergies can induce a variety of allergic reactions.[9] The connection between food sensitivities and eczema has primarily been examined in children and infants. Several studies have found that about 10%-30% of children with eczema have food-related exacerbations of symptoms.[9][10][11] The most common foods implicated are milk, eggs, and peanuts. Others to consider include soy, wheat, fish, and tree nuts. Testing for these allergies can be done either by atopy patch testing or by measuring food specific IgE antibodies. Both tests have limitations, and elimination diets should be used to confirm the sensitivity.[12][13] For more information, refer to the Elimination Diets” Whole Health tool.
Once a food sensitivity has been identified and confirmed by elimination, avoidance of the food can minimize flares of eczema. However, care must be taken to make sure that adequate nutrient intake is maintained. When multiple foods are implicated, the risk of nutritional deficiencies increases. It is important to educate patients and their families about maintaining a healthy diet with adequate nutrient intake.[14]
Supplements
Note: Please refer to the Passport to Whole Health, Chapter 15 on Dietary Supplements for more information about how to determine whether or not a specific supplement is appropriate for a given individual. Supplements are not regulated with the same degree of oversight as medications, and it is important that clinicians keep this in mind. Products vary greatly in terms of accuracy of labeling, presence of adulterants, and the legitimacy of claims made by the manufacturer.
Gamma Linolenic Acid
Essential fatty acid deficiency can cause eczema-like skin changes including dry, scaly, itchy skin with impaired barrier function. Replenishing these essential nutrients reverses the skin problems seen in deficiency states. This has led people to consider potential abnormalities in essential fatty acid metabolism in people with atopic dermatitis. At least some patients with eczema may have decreased levels or defects in delta-6-desaturasean enzyme involved in converting linoleic acid (found in seed and corn oils) to gamma-linolenic acid (GLA). GLA is an omega-6-polyunsaturated fatty acid that is converted to dihomo-GLA which is important in the formation of anti-inflammatory prostaglandins in the skin.[15][16]
Given these findings, it would make sense that supplementation with GLA (found in borage oil, evening primrose oil, hemp oil, and black current oil) should help with the management of eczema. However, studies looking at useparticularly of borage oil and evening primrose oilhave been conflicting. A recent Cochrane review looking specifically at studies evaluating borage and evening primrose use in eczema found no benefit.[17] Many of the studies included were small and flawed. Overall, these products are generally safe, with GI side effects being the most commonly reported. However, there may be increased risk of bleeding when taken concomitantly with other anticoagulants.
- Dose: 920 mg GLA daily for people ages 18 and up, 360-460 mg daily for children younger than 18 [18][19]
Omega-3 Fatty Acids
Omega-3 fatty acids are known to promote an anti-inflammatory profile of leukotrienes and prostaglandins. DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid) are found in fish oil and do not require modification by the enzyme delta-6-desaturase to be activated. Other sources including flax seeds, hemp seed, nuts, leafy green vegetables, soybeans, and algae do require delta-6-desaturase activity. This enzyme is also used by the omega-6 fatty acids, which promote pro-inflammatory leukotrienes and prostaglandins. If the ratio of omega-6 to omega-3 fatty acids is too high, the benefit of additional omega-3 fatty acids is negated from an inflammatory standpoint.[20]
Evidence for use of omega-3 supplementation in atopic dermatitis is limited but promising. [21] Thirty-one patients with moderate to severe atopic dermatitis experienced decreases in itching, scaling, and subjective severity after receiving 10 gm of fish oil/day (containing EPA) for 12 weeks.[22] An epidemiologic study looking at Korean children found that those who had atopic dermatitis had lower omega-3 to omega-6 ratios.[23] Additionally, it appears from many studies that fish and fish oil consumption during pregnancy and lactation decreases the risk of developing eczema in infants, but evidence is not as strong for supplementation of infants.[24]
- Dose: Fish oil supplementation recommendation is 2-4 gm daily for treatment of active inflammatory conditions, and 1 gm daily for prevention.[20]
Probiotics and Prebiotics
Many studies support probiotic supplementation (Lactobacillus rhamnosus GG in particular) in pregnant or breastfeeding mothers and infants; it has been found to prevent the development ofand reduce the severity ofatopic dermatitis.[25][26][27] While there is still much to be learned, evidence is building that use of pre- and probiotics in the prenatal and perinatal periods, as well as early childhood, is protective against the development of atopic dermatitis.[28]
The use of probiotics for treatment of established atopic dermatitis is not well studied, and available research is generally not promising. There is one good study looking at the use of a specific strain of Lactobacillus salivarius (LS01) in 38 adult patients with atopic dermatitis over 16 weeks. These researchers found significant clinical improvement in the treated group versus the control group, as well as differences in the cytokine profiles of the two groups favoring the treated group.[29]
There are many strains of probiotics, and comparing studies is difficult since most use different strains. Hopefully, research will continue to offer more information about the specific doses and microorganism strains that are likely to be most helpful in specific skin conditions like atopic dermatitis. For more information, refer to Promoting a Healthy Microbiome with Food and Probiotics Whole Health tool.
Vitamin D
There have been a few studies looking at vitamin D levels in people with atopic dermatitis. A recent review and meta-analysis found that people with atopic dermatitis especially kids are more likely to have low levels of vitamin D. One review identified three intervention studies and found that a dose of 1,600IU a day for three months or more is likely to result in improvement of the atopic dermatitis severity.[30][31]
- Dose: 1,600IU Vitamin D3 daily for 3 months or more
For more information, refer to Promoting a Healthy Microbiome with Food and Probiotics Whole Health tool.
Topical Botanicals
Glycyrrhetinic acid
Glycyrrhetinic acid is a component from licorice root that has inhibitory activity on the enzyme 11-beta-hydroxysteroid dehydrogenase which is responsible for inactivating cortisol. It has been shown to potentiate the action of hydrocortisone in the skin. [32] Glycyrrhetinic acid has also been shown to have anti-inflammatory properties as well as ability to decrease IgE-related skin diseases in mice [33] and inhibit histamine synthesis in mast cells in vitro.[34]
Atopiclair is a topical over-the-counter cream that contains 2% glycyrrhetinic acid as well as vitis vinefra (a grapevine extract which is high in antioxidants and enzymes that prevent degradation of proteins in the skin) and telmestine (which contains several classes of enzymes that inhibit the degradation of compounds important to the structure of the skin). Purified shea butter and hyaluronic acid are also present in this preparation and are high quality emollients. Several studies looking at use three times a day have found it to be beneficial in patients with mild to moderate atopic dermatitis.[35][36][37][38] Stinging and burning occurred in some people using this preparation.
- Dose[35]: 2% cream or ointment
Chamomile
Chamomile is a member of the Asteraceae family which includes plants such as rhubarb, chrysanthemum, aster, daisy, sunflower, zinnia, dandelion, echinacea, and many others. In Germany, chamomile has been called alles Zustraut which means capable of anything. It has long been used to treat skin inflammation and it appears to have similar efficacy to 0.25% hydrocortisone. While good clinical studies are lacking, it seems to have anti-inflammatory, antimicrobial, and antioxidant properties. Additionally, flavonoids present in chamomile have been shown to prevent histamine release from basophils.[39]
Chamomile can be found in cream or ointment formulations and should contain 20 gm of essential oil per 100 gm of the base. Chamomile can also be used in the bath by adding 5 gm powder or 0.8 gm alcoholic extract per liter of water. Poultices can be prepared by steeping 6 gm dried powdered flower heads in 150 mg boiled water. This should be cooled and applied as a poultice for one hour twice a day.
There have been many reports of allergic contact dermatitis and irritation from chamomile. Although anyone can develop a contact dermatitis to chamomile, people who are known to be allergic to other members of the Asteraceae family are at a higher risk, and they should probably avoid products containing calendulaespecially in areas of skin breakdown.
- Dose [40]
- Creams or ointments: Should contain 20 gm of essential oil per 100 gm of the vehicle
- Bath: Add 5 gm powder or 0.8 gm alcoholic extract per L of water
- Poultice: 6 gm dried powdered flower heads in 150 mL boiled water; apply rags soaked in this preparation for 1 hour twice a day
Indigo Naturalis Extract
Indigo naturalis extract has been shown to increase fillagrenan important protein in the epidermal skin barrier that is often deficient or defective in people with atopic dermatitis.[41] A small clinical trial showed significant improvement in people with moderate to severe atopic dermatitis who used Indigo naturalis ointment twice a day for 6 weeks.[42] While contact dermatitis is possible, it has not been reported in the studies of indigo for atopic dermatitis or psoriasis.
- Dose: 3%-7% cream, ointment or oil twice a day
Calendula.
Calendula officinalis is commonly known as marigold and has been used historically to soothe irritated skin. Studies looking specifically at the usefulness of calendula in atopic dermatitis are lacking. Calendula appears to have antibiotic, antiviral, anti-inflammatory, and antioxidant properties.
Although anyone can develop a contact dermatitis to calendula, people who are known to be allergic to other members of the Composite family are at a higher risk. They should avoid products containing calendulaespecially in areas of skin breakdown.
- Dose:[43]
- 2%-5% ointment/cream
- 1:1 tincture in 40% alcohol or 1:5 tincture in 90% alcohol*
- *Dilute with boiled water to a 1:3 ratio in order to be applied on the skin.
Food grade oils
Oils intended for consumption can work really well as occlusive moisturizers. Almond oil, avocado oil, apricot kernel oil, grapeseed oil, sunflower oil, jojoba oil, coconut oil, and shea butter tend to be well tolerated. Some shea butter preparations can contain trace amounts of latex and should be avoided by people who have a latex allergy. There is a potential risk of contact dermatitis, and any food allergies (such as to tree nuts) should be taken into consideration when choosing an oil for topical application.
Other Therapies to Consider
Lifestyle Choices
Regular exercise and good sleep are important for all aspects of overall health. Many people with atopic dermatitis suffer from sleep disturbances. Sleep is extremely important, not only for physical health, but for emotional health as well. Sleep deprivation has been shown to result in increased systemic inflammatory markers.[44] Additionally, people who do not get adequate sleep are more likely to be diagnosed with depression and anxiety,[45][46] and maintaining adequate sleep schedules can be a part of treatment for depression.[45] The Recharge Whole Health overview has general information on sleep and health.
People who suffer from eczema commonly complain of poor sleep quality. Indeed, sleep disturbances have been reported in as many as 60% of patients with atopic dermatitis.[47] Children with eczema have been found to have increased nocturnal wakefulness, a higher number of shifts between sleep stages, and longer latency to REM onset.[48] One study looked at sleep disturbance in 72 people with atopic dermatitis compared to 32 healthy controls based on data from actigraphy and polysomnography as well as samples looking at melatonin metabolites, cytokines and IgE levels. The objective measures for sleep disturbance positively correlated with severity of atopic dermatitis, and degree of sleep disturbance was significantly associated with lower nocturnal melatonin.[49]
A subsequent randomized, double blind, placebo controlled crossover study looked at melatonin supplementation (3mg/day) for 4 weeks vs. placebo in patients between the ages of 1 and 18 with atopic dermatitis who had a body surface area involvement of 5% or more. The 38 people who completed the crossover had significant decreases in objective measures of atopic dermatitis as well as decreased sleep onset while taking melatonin when compared to placebo.[50] Many people with atopic dermatitis also have symptoms of anxiety and depression, which can also contribute to poor sleep. It is unclear if associated mood disturbances are due to inadequate and/or poor quality sleep, or if the sleep disturbances are responsible for mood issues some of these patients have. Likely the situation is a vicious cycle, with each aspect feeding the other.
Identifying those patients with sleep disturbances and offering counseling and/or information about good sleep hygiene, including a recommendation for melatonin supplementation along with the physical management of eczema, may offer additional benefit in improving both the disease and the quality of life. For more information, go to Passport to Whole Health Chapter 9, Eleven Tips for Improving Sleep Whole Health Tool.
Mind-Body
There are numerous mind-body approaches to health. Three of the more common modalities include clinical hypnosis, biofeedback, and Cognitive Behavioral Therapy (CBT). Medical hypnotherapists help guide people into a deeply relaxed trance state and make suggestions with specific intentions regarding the alleviation of suffering and promotion of healing. Biofeedback uses technology to help patients learn to relax by teaching them to control their autonomic nervous system. CBT helps bring inaccurate or negative thinking into awareness so challenges can be seen more clearly and responded to in a more effective manner.[51] For more information about mind-body tools, refer to the Power of Mind Whole Health overview.
All of these modalities can be especially beneficial in skin conditions that are triggered or worsened by stress, including atopic dermatitis. The relationship between practitioner and patient is extremely important, and it is crucial to find a practitioner that one can work with comfortably.
Traditional Chinese Medicine (TCM)
TCM is a health system that has been around for over 2,500 years. It is based on the premise that qi is a vital energy that maintains health and balance in the body. Two opposing but complementary forcesyin and yangsupport health when they are in harmony and are responsible for disease when they are out of balance. There are several techniques used in the scope of TCM, with acupuncture and herbal medicine being the most common in the United States. As a system, the techniques are best used in combination by skilled practitioners. Acupuncture and TCM herbs have been shown effective for people with atopic dermatitis in a number of studies.[52][53][54]
When looking for a TCM practitioner, one should inquire about certification and education. Any practitioner should have state licensure at the very minimum. The National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) has strict certification requirements, and members are required to recertify every 4 years. For NCCAOM-certified practitioners visit the organizations website. For more information, refer to Passport to Whole Heath Chapter 18, Whole Systems of Medicine.
Energy Medicine
The field of energy medicine is broad and encompasses therapies that manipulate subtle energy fields imperceptible to most people. It is based on the premise that healing energy can be channeled into another person via hands-on, hands-off, and/or distant techniques. Healing Touch (or therapeutic touch), reiki, and spiritual or faith healing are the most well known in the United States. Energy medicine is a very subtle approach to facilitating healing and difficult to study. The evidence supporting this area of healing is shaky, but the risks are minimal and many people do find energetic approaches to healing beneficialespecially in decreasing anxiety, worry, and fatigue, which are common in people who have atopic dermatitis. Healing Touch is available in many VAs and would be a good place to start for people interested in this modality. Refer to Energy Medicine: Biofield Therapies, Chapter 17 of the Passport to Whole Health, to learn more.
Homeopathy
Homeopathy is a medical system that treats disease with highly diluted substances with the goal of triggering the bodys innate ability to heal. Remedy selection takes into consideration the patients symptoms, personality traits, physical and psychological states, and life history. Although research is limited, homeopathy can be helpful for some patients with atopic dermatitis.[55][56] Because worsening of a condition is a possible adverse reaction, especially early in treatment, it is important to work with a well-trained and qualified homeopathic practitioner. One should look for a practitioner who is certified by at least one of the following organizations: Council for Homeopathic Certification (CHC), North American Society of Homeopaths (NASH), American Board of Homeotherapeutics (ABHt), or Homeopathic Academy of Naturopathic Physicians (HANP). For more information, refer to Biologically-Based Approaches: Dietary Supplements, Chapter 15 of the Passport to Whole Health.
Prevention Overview: Atopic Dermatitis
- Take gentle care of your skin.
- Bathe in lukewarm water with gentle soaps.
- Apply thick creams or ointments while skin is still slightly damp.
- Ensure adequate good-quality sleep and consider melatonin supplementation.
- Take an anti-inflammatory dietary approach, and reduce intake of refined carbohydrates.
- Consider taking an omega-3 supplement.
- Consider taking supplemental vitamin D3.
- Consider taking a good-quality multivitamin that contains appropriate doses of zinc, vitamin A, and vitamin E.
- Consider topical glycyrrhetinic acid, indigo, calendula, and/or chamomile.
- Learn about different approaches to stress management.
Author(s)
Atopic Dermatitis was written by Apple Bodemer, MD (2014, updated 2020).



















