What is Heart Rate Variability?
Heart rhythm, the pattern of heart contraction and relaxation, is the response of the heart muscle fibers to electrical activation. The electrical signal comes from specialized cells and fibers within the upper and lower chambers of the heart, the atria and ventricles. Heart rate should be 60-99 beats per minute at rest.
Under normal conditions, a healthy heart displays slight beat-to-beat variability; that is, it is healthy to have variation in the time between your heartbeats. For example, in sinus arrhythmia, a healthy heart rhythm pattern, the interval between beats shortens during inspiration and lengthens during exhalation. A healthy heart rhythm is not strictly regular, but varies slightly, a result of numerous factors, especially vagus nerve activity. This is true for fetal heart monitoring in women in labor, and it is true throughout our lives, though HRV tends to decrease with age.[1]
In an electrocardiogram (ECG), this is reflected in the R-R interval. R-R interval variability reflects a confluence of the complex interplay between many factors. Especially important is the balance between the sympathetic and parasympathetic arms of the autonomic nervous system, which is itself influenced by physical, emotional, pharmacologic, and pathophysiologic factors. Heart rate variability (HRV) may be taken as an indicator of baroreflex (blood pressure sensing) activity and psychophysiological resilience (the bodys response to the minds experience). High HRV signifies healthy systemic adaptability, and low HRV points to susceptibility to the negative consequences of stress and disease.[2]
Measuring HRV may provide useful clinical information about autonomic tone and heart function. In addition, reductions in HRV have been associated with a wide range of disorders.
There has been growing interest in the potential role of the heart as a sensory organ, specifically as relates to emotions and the interplay between brain and heart as collaborative interpreters of our environment. Some experts believe that people are most healthy when cardiac, respiratory, and central nervous system activities align and function in synchrony. This reflects as balanced autonomic nervous system tone and, in part, high HRV.
Clinical Importance of Heart Rate Variability
As an independent variable, HRV is believed to have significant prognostic importance. Low HRV is correlated with increased all-cause mortality and a range of noncardiac disorders including diabetes mellitus (where autonomic nervous system dysfunction is common), fibromyalgia, and neurologic and psychiatric disorders such as epilepsy, Parkinsons disease, anxiety, depression, and posttraumatic stress disorder (PTSD). Acute, intense stress, of the kind frequently experienced by military personnel, is related to parasympathetic withdrawal and high cortisol levels. High cortisol levels are associated with reduced memory, impaired cognitive performance, and an increase in mental errors. HRV varies inversely with cortisol secretion during stressful tasks. People with high resting HRV recover quickly and function at a higher level.[3]
Reduced HRV has been tied to an increased risk of dysrhythmias and sudden cardiac death in the recent post-heart attack period, as well as worsened prognosis in the setting of heart failure. It has been noted to occur in people at risk for suicide, though additional research is needed to gauge how well it can help gauge a persons risk of dying by suicide.[4]
Abnormalities of heart rhythm may occur as a result of underlying coronary artery disease, reentry phenomena (misguided flow of electricity), cardiotoxin exposure, ectopic foci (areas of the heart that send out inappropriate electrical signals), medication side effects, and other influences. Apart from lowered HRV, factors that may promote cardiac arrhythmias include stimulant or alcohol use, cigarette smoke,[5] sympathetic nervous system overdrive as a result of psychosocial stress, and the use of certain medications.[6]
Prevention of heart rhythm problems should be a first priority. Not only does this reduce risks to morbidity and mortality, but also because conventional medical treatment of a cardiac arrhythmia has to deal with potential treatment side effects. Dietary and lifestyle factors may help lower the risk for arrhythmias, as may a variety of complementary and integrative health (CIH) approaches, like acupuncture, spinal manipulation, and dietary supplements.
Most of the research on problematic heart rhythms has focused on atrial fibrillation (AF), one of the most common arrhythmias people experience.
Me at the Center
As you explore the Circle of Health with someone, it may be informative to frame questions of Mission, Aspiration, and Purpose (MAP) around expressions related to the heart. Some examples include:
- What is your hearts desire?
- When is your heart most open?
- What makes your heart sing?
- Who is in your heart?
More specifically, you can explore peoples history with irregular rhythms or palpitations. You can also get a sense of how stress affects their lives and how they do (or do not) manage it. Of course, all this exploration is done within the broader context of each individuals life.
Mindful Awareness
Mindful awareness ties in closely with HRV. For example, activities that encourage a person to focus on breath can have a profound positive influence on HRV. We can learn to settle our breathing rate so that it moves into a sweet spot where our HRV is optimized. For most people, that is somewhere in the neighborhood of 5-6 breaths per minute.
More information is available in the Breathing and Power of Breath: Diaphragmatic Breathing Whole Health tools.
Self-Care
Healthy lifestyles lower risks of unhealthy heart rhythms, like atrial fibrillation (AF). AF increases with excess weight, metabolic syndrome, and stress, all of which can be managed through enhancing self-care.[7] All the areas of self-care are important to heart health, as noted in the Whole Health Heart Health overview, and for some, there are studies of their effects specific to heart rhythm.
Food and Drink
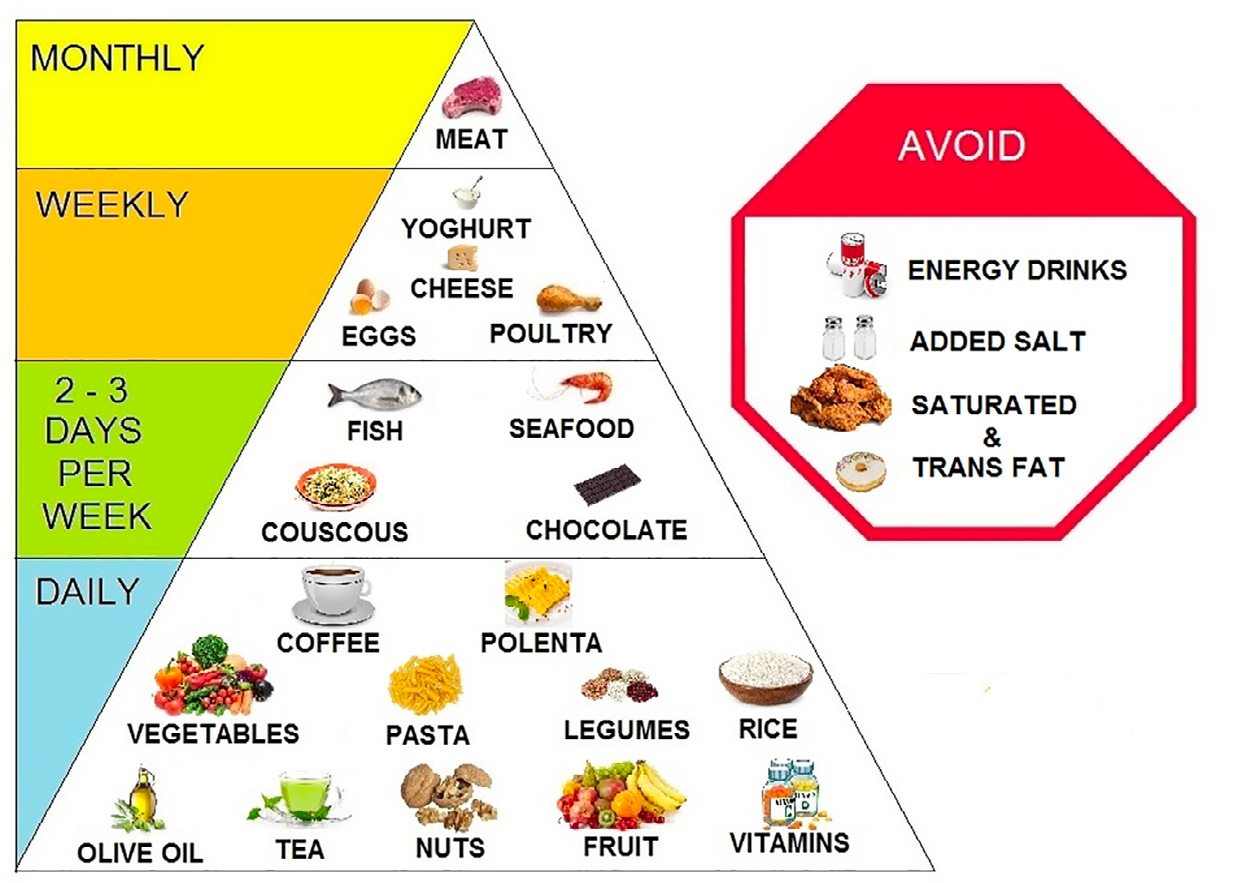
Food and drink choices can influence heart rhythm through a variety of means. Coffee, tea, nuts, antioxidant vitamins, and chocolate may have some benefits, while energy drinks, added salt, and saturated fat may be harmful.[8] This is summarized in Figure 1.
Weight loss. Weight loss has a positive effect on heart rhythm. In one observational study, people who achieved >10% weight loss had six times the reduction of AF recurrences compared to people who lost <3% of their body weight.[9]
Diet patterns. Following a Mediterranean pattern of eating, or the DASH Diet, provides safe and adequate amounts of magnesium, potassium, and other nutrients that help support normal sinus rhythm. One study found that the closer one comes to eating a Mediterranean diet, the better their HRV. Those with the highest adherence to the Mediterranean diet in one large case control study had the highest rate of conversion from AF to sinus rhythm (odds ratio of 1.9.)
Omega-3 fatty acids can be obtained by eating cold-water, fatty fish or perhaps through supplementation with high-quality fish oil. Omega-3s may help protect against life-threatening arrhythmias following acute coronary events. However, there is little evidence supporting an overall antiarrhythmic effect of omega-3s, especially against ventricular ectopy.[10] They may increase heart HRV.[11]
Alcohol. Alcohol has a role in the Mediterranean diet, but moderation is important for many reasons, not the least of which is the association of binge drinking and subsequent development of arrhythmias, including atrial fibrillation. A 2019 review of 33 articles explored the effects of alcohol on HRV.[12] Acute alcohol use reduces resting HRV. HRV also decreases in people with alcohol use disorders and it has been found that it takes the heart at least four months to return to baseline once a person became abstinent from long-term alcohol abuse.
Caffeine. A 2018 review summed up the effect of caffeine on heart rhythm as follows[13]:
- Caffeine has a range of effects on the sympathetic nervous system, calcium trafficking in the cells, and adenosine receptor function. It is also an antioxidant.
- Caffeine at high doses may induce arrhythmias in part by increasing calcium levels in cells.
- Caffeine may actually be anti-arrhythmic at normal doses, because of how it affects adenosine receptors.
- A review of 11 studies found only one small study that indicated coffee had a negative effect on atrial arrhythmias. Three studies found consistent benefits, and the rest showed no effects.
- Only two lower-quality studies found a link between coffee and ventricular arrhythmias, and these were for intake at >9-10 cups daily. Other studies showed no association.
- In rat models, tea actually decreases ventricular arrhythmias. In humans, this also seems to be the case in people who drink up to 14 cups a week. In fact, 3 cups of tea per day significantly reduces a persons risk of cardiac death (relative risk 0.74)[14].
- Energy drinks, which have higher amounts of caffeine relative to coffee or tea, have been found to lower HRV and increase QTc. Regular consumers report frequent palpitations, and there are many case reports of arrhythmias secondary to their use.[15] Even consuming one energy drink a day may be harmful.[16]
Tobacco. Cigarette smoking can induce cardiac arrhythmias along with all the other contributions it makes to health problems.[5] Stopping smoking is always a worthy goal.
Minerals. Magnesium is important to healthy heart rhythms, so consuming foods that contain it is worth recommending. Examples include grains, nuts, dark chocolate, green vegetables, and avocados. People with low levels had a 50% higher risk of having an initial episode of AF[17], but studies have not conclusively shown that dietary magnesium supplementation is beneficial for preventing or treating AF.[8]
Moving the Body
Regular physical activity enhances vagal tone, reduces release and sensitivity to catecholamines, and improves heart rate variability, all of which protect against cardiac rhythm disturbances. Exercise can occasionally induce arrhythmias, but for most patients the health benefits of maintaining and improving aerobic capacity outweigh potential risks.
Yoga and exercise programs reduce AF and its overall health burden.[18][19][20] Exercise programs, in general, not only improve quality of life but also reduce AF symptoms and frequency, according to a 2018 review.[7]
According to a 2016 review of tai chi and HRV, tai chi can enhance vagal modulation and reduce sympathetic modulation, increasing HRV.[21] More studies are needed to assess how much this can have a meaningful clinical effect.
Recharge
Sleep quality is linked to heart rhythm. People who sleep less have a higher risk of AF.[22] A small 2012 study found that HRV and endothelial function are impaired in people who do shift work, probably because of higher sympathetic and/or lower parasympathetic activity.[23] Obstructive sleep apnea is linked to arrhythmia risk and should be kept in mind.[24]
Surroundings
Various aspects of our surroundings can have an important impact on heart rhythm, just as they do on many other aspects of our health. For example, a 2017 study concluded that long working hours (versus standard hours) increases a persons risk of developing AF over a 10-year period (hazard ratio 1.4)[25]. Higher overall stress at work is associated with decreased HRV.[26][27]
Power of the Mind
Chronic stress can negatively affect the balance between the parasympathetic and sympathetic nervous systems through a variety of means, reducing HRV and increasing arrhythmia risk.[28][29] Negative emotions like anger can trigger arrhythmias.[30] Long-term negative emotions can increase risk of arrhythmias in people with implanted defibrillators.[31]
Regular practice of mind-body therapies can be helpful. HRV biofeedback has been shown to lead to a large reduction in self-reported stress and anxiety.[32] A 2020 review and meta-analysis concluded it improves emotional and physical health and performance in a variety of ways.[33] The most significant effect sizes were found for using it in anxiety, depression, anger, and athletic/artistic performance.
Meditation of various types has a favorable impact.[34] A 2015 study comparing meditation, HRV biofeedback, and exercise found that all three had equivalent beneficial effects on stress, anxiety, depression, sleep quality, an overall well-being.[35]
Clinical hypnosis also seems to be associated with improved HRV, according to a small 2017 trial, both while someone is hypnotized and after.[36] This is also the case in small trials using Guided Imagery.[37] Equine Therapy also seems to have beneficial effects.[38]
When all is said and done, the bottom line is that heart rhythm, and many other aspects of health, benefit from healthy management of stress.
Complementary and Integrative Health Approaches
Acupuncture
Acupuncture has a long history of use for heart rhythm disturbances. A 2011 study found that, over 12 months, people with persistent AF who had recently had an ablation had a recurrence rate of 35% if in the acupuncture group, compared to 69% of those who received sham acupuncture, 54% of controls, and 27% of the people in the group that took the drug amiodarone.[39] The acupuncture group received 10 weekly sessions of acupuncture starting within 48 hours of cardioversion. A later study by the same authors also found benefit for acupuncture for paroxysmal AF.[40] Studies had relatively small sample sizes and found no indications of adverse effects.
Dietary Supplements
Note: Please refer to the Passport to Whole Health, Chapter 15 on Dietary Supplements for more information about how to determine whether or not a specific supplement is appropriate for a given individual. Supplements are not regulated with the same degree of oversight as medications, and it is important that clinicians keep this in mind. Products vary greatly in terms of accuracy of labeling, presence of adulterants, and the legitimacy of claims made by the manufacturer.
Caution is recommended with stimulant herbs. Substances, such as guarana, ginseng, yohimbine, and ephedra (including its derivative ma huang), may augment pro-arrhythmic effects of caffeine.[41]
Of note, botanicals such as khella (Ammi visnaga, from which amiodarone and nifedipine were developed), rhodiola (Rhodiola rosea, extracts of which show some anti-arrhythmic activity), motherwort (Leonurus cardiaca, associated with negative chronotropic effects), and hawthorn (Crataegus sp., a traditional cardiac tonic with suggestion of anti-arrhythmic activity), have shown promise.[42][43] Concerns about overlapping mechanisms of action with conventional anti-arrhythmic agents, and thus increased potential for toxicity, as well as limited data on safety and effectiveness, serve to relegate herbal therapy against arrhythmias as no more than investigational. Coenzyme Q10 (CoQ10) does seem to offer protection against rhythm disturbances in people with AF.[44]
Body-Based Therapies
Chiropractic care leads to significant favorable changes in HRV.[45] A 2018 systematic review of 9 studies chosen from a pool of 505 concluded that osteopathic manual therapy (OMT) exerts an influence on sympathetic and parasympathetic tone (and thereby, HRV) that varied depending where in the body manipulation was done.[46]
In Summary
Keep an array of options in mind as you are working with someone on their Personal Health Plan (PHP) to improve HRV or prevent/treat arrhythmias. Some of the most supportive research has suggested benefit from the following options, many of which seem to balance sympathetic and parasympathetic tone:
- Acupuncture
- Aerobic exercise
- Biofeedback (namely, HRV biofeedback)
- Breathing exercises
- Good sleep
- Healthy work environment
- Meditation
- Mediterranean diet
- Omega-3 fatty acids (increased intake)
- Smoking cessation
- Spinal manipulation
- Tai Chi
- Yoga
Author(s)
Heart Rate Variability and Arrhythmias was written by Russell H. Greenfield, MD and updated by J. Adam Rindfleisch, MPhil, MD (2014, updated 2020).



















