Community Care Network–Information for Providers
The VA Community Care Network (CCN) is VA’s direct link with community providers to ensure Veterans receive timely, high-quality care. CCN uses industry-standard approaches and guidelines to administer services, pay for services promptly, and manage the network to its full potential.
CCN is the preferred national network VA uses to purchase care for Veterans in their community.
On this page
Regional Networks
CCN is comprised of five regional networks that serve as the contract vehicle for VA to purchase care for Veterans from community providers.
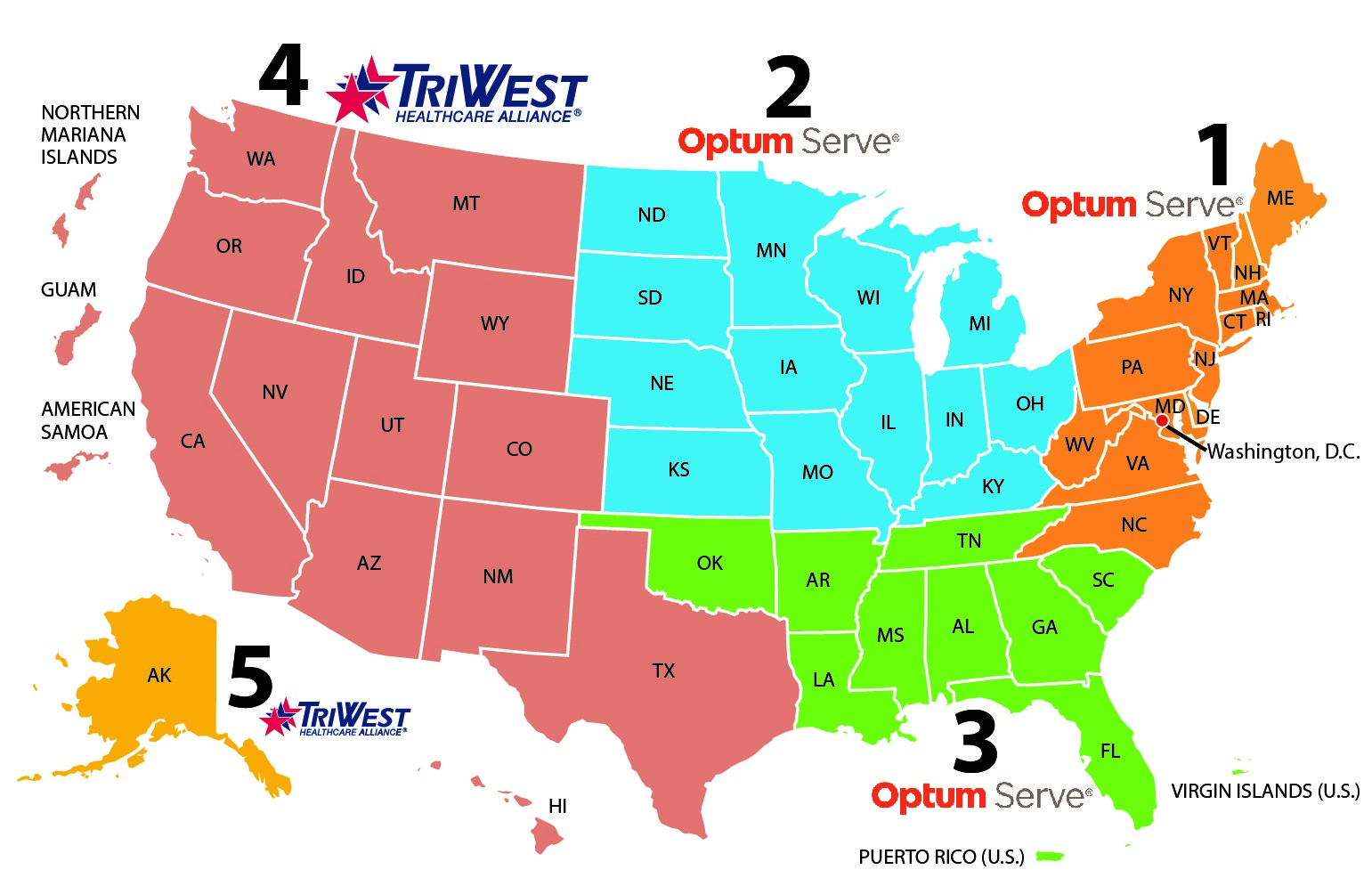
| Region 1 | Region 1 map | Connecticut, Delaware, District of Columbia, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, New York, North Carolina, Pennsylvania, Rhode Island, Vermont, Virginia, West Virginia |
|---|---|---|
| Region 2 | Region 2 map | Illinois, Indiana, Iowa, Kansas, Kentucky, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin |
| Region 3 | Region 3 map | Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Oklahoma, Puerto Rico, South Carolina, Tennessee, Virgin Islands (U.S.) |
| Region 4 | Region 4 map | American Samoa, Arizona, California, Colorado, Guam, Hawaii, Idaho, Montana, New Mexico, Nevada, Northern Mariana, Islands, Oregon, Texas, Utah, Washington, Wyoming |
| Region 5 | Region 5 map | Alaska |
NOTE: Optum Public Sector Solutions, Inc. (Optum), part of UnitedHealth Group, Inc., serves as the third party administrator (TPA) for CCN regions 1, 2, and 3. TriWest Health Care Alliance (TriWest) serves as the TPA for regions 4 and 5.
Join CCN
If you are a community provider located in Regions 1-5 and are ready to partner with VA to care for Veterans, sign up to join CCN today! Contact Optum or TriWest below:
Regions 1, 2 and 3–Contact Optum:
Region 1: 888-901-7407
Region 2: 844-839-6108
Region 3: 888-901-6613
Regions 4 and 5–Contact TriWest:
Provider Contract Request website (preferred)
877-CCN-TRIW (877-226-8749)
CCN Frequently Asked Questions
What is the Community Care Network (CCN)?
CCN is the preferred national network VA uses to purchase care for Veterans in their community.
Why did VA hire third party administrators?
CCN is part of the VA modernization efforts to increase transparency, accountability, quality, and communications between VA, providers, and Veterans to improve Veterans' access to care. The selected TPAs for each region administer CCN with transparency, accountability, quality, and in accordance with the enhanced requirements of the contract.
What happens if a Veteran needs a referral for additional health care services?
Community providers submit a referral request directly to VA when a Veteran requires care beyond what is included on the original referral.
Who is responsible for handling customer service for Veterans?
VA directly manages Veteran community care customer service touchpoints while the TPAs (i.e. Optum or TriWest) support inquiries from community providers and VA.
What are Veterans Care Agreements (VCAs)?
VCAs are agreements between a community provider and a VA medical facility that are used in limited situations where contracted services through CCN are either not provided or not sufficient to ensure Veterans can receive the care they need. The term of the VCA is three years, beginning on the effective date. Community providers and agencies participating through a VCA must be credentialed through VA's Credentials Verification Organization (CVO) contractor. Learn more about VCAs below.
Veterans Care Agreements
For questions and support, contact your local VA medical facility’s community care office.
Where do I get information on claims and payments?
Community providers should refer to the terms of the applicable contract or agreement governing their provision of community care to determine requirements regarding claims and payments. The applicable contract or agreement may be directly with VA or a TPA under contract with VA to administer portions of VA’s community care program.
The status of a community care claim filed directly with VA is available in the Customer Engagement Portal (CEP) (registration required). Patient and claim identifiers are needed to locate the unique claim status information. Questions about the status of claims submitted to a TPA should be directed to the TPA for your region.
Where can I get information about training and credentialing?
Providers can access required training courses through VHA TRAIN. Community providers may create an account, register for and complete any required courses. Maintaining training standards is essential for network providers to continue to receive referrals.
For credentialing, community providers participating in CCN must be credentialed through a TPA. Community providers participating through a VCA must be credentialed through VA.
How do I become a CCN dental provider?
Dental providers with practices located in Regions 1, 2, and 3 interested in serving Veterans in their community should visit the Logistics Health, Inc. (LHI) Provider Portal. Dental providers with practices in Region 4 and 5 interested in serving Veterans in their community should contact TriWest.
Following submission of necessary documentation, the TPA for the provider’s region of CCN (i.e. Optum or TriWest) will reach out to you to complete the enrollment process.
What is External Provider Scheduling?
The External Provider Scheduling (EPS) process uses the WellHive digital platform to enable VA schedulers to view and make appointments directly into in-network community provider scheduling grids. This eliminates many of the steps often taken between the VA scheduler, community provider, and Veteran; saves time in the scheduling process; and improves access to the soonest and best care. For questions or inquiries contact the EPS Provider Engagement Team.



















