Whole Health emphasizes mindful awareness and Veteran self-care along with conventional and integrative approaches to health and well-being. The Circle of Health highlights eight areas of self-care: Surroundings; Personal Development; Food & Drink, Recharge; Family Friends, & Co-Workers; Spirit & Soul; Power of the Mind; and Moving the Body. The narrative below shows what a Whole Health clinical visit could look like and how to apply the latest research on complementary and integrative health to neck pain.
A Whole Health approach to neck pain incorporates proactive self-care. This may include an anti-inflammatory diet, manual therapies, and various ways to move the body such as yoga, qi gong, and tai chi. Dietary supplements, injection therapies, and other conventional and complementary approaches also can be considered.
Meet the Veteran
Michael is a 35-year-old Navy Veteran who is complaining of midline and left-side neck pain that he developed about three years ago following a whiplash injury during military service. The symptoms have been slowly getting worse. He currently works in a customer service position that is mostly sedentary. The neck pain is generally mild in the morning, but gets worse as the day progresses. He does not have any associated neurological signs, such as pain down the arm, extremity weakness, or bowel or bladder dysfunction. The neck pain is occasionally accompanied by mild posterior headaches.
He has a normal neurological exam, some point tenderness in the mid-cervical region and left cervical paraspinal muscles.
Imaging showed nonspecific mild degenerative disk and facet changes of the lower cervical spine.
Michael has tried a variety of treatments, including several courses of Physical Therapy, chiropractic care, and acupuncture without significant sustained improvement. Ibuprofen and Tylenol “take the edge off” but do not provide any lasting relief. He takes Nortriptyline at bedtime and finds that it helps reduce daytime pain the next day.
He is frustrated about the lack of improvement in his symptoms despite treatments and the impact that neck pain has on his day-to-day quality of life. He is wondering if he will have “to live with this pain” for the rest of his life and feels anxious about it.
Refer to Michael’s PHI.
Background
Neck pain is a common presenting complaint both in primary care and rehabilitation setting.[1] Yearly prevalence of neck pain is estimated at 30%-50%, and lifetime prevalence is estimated at two-thirds.[2][3]
The neck contains many vital structures, including the spinal cord, various nerves (including spinal nerves and vagus nerve), major blood vessels, swallowing and breathing tracts, vocal cords, and thyroid and parathyroid glands.[4] The neck has capacity to both be flexible and rigid, thanks to the presence of 37 separate joints and multiple muscle and connective tissue structures. It is also the area of the body that can be vulnerable both physically and metaphorically. On a subtler level, the neck is a center of self-expression and communication.
All potential causes of neck pain must be considered, keeping in mind that most common etiology of neck pain is musculoskeletal.[1][3][4][5] Exact structures responsible for pain can be very difficult to identify with precision. In the majority of cases, pain localizes to the posterior or lateral neck regions in a variable distribution and can also spread to the suboccipital region or upper shoulder and thoracic areas.[4] For the purposes of this clinical overview, the focus will be on musculoskeletal neck pain that does not require emergent treatment. Anterior neck pain will not be covered.
Musculoskeletal neck pain can be further subdivided into traumatic and nontraumatic.[4] Traumatic neck pain often results from a hyperextension injury such as whiplash and can often develop into a chronic complaint.[4][6] However, it is important to keep in mind that in less litigious countries, long-term negative effects of whiplash are almost nonexistent. This may cause one to question both the mind-body and secondary gain effects on long-term outcomes of posttraumatic neck pain.[4][7]
Nontraumatic neck pain is most commonly related to myofascial disorders, but can certainly be related to structural or degenerative issues. Sedentary lifestyle, poor posture, repetitive overuse including work and sports-related injuries are the common factors implicated in soft tissue neck pain.[4] Mental health also plays an important role. There is a definite correlation between incidence of neck pain and presence of anxiety or depression.[4][8]
Definitions
The International Association for Study of Pain (IASP) defines acute neck pain as lasting less than 7 days, subacute neck pain lasting between 7 days and 3 months, and chronic neck pain lasting 3 months and longer.[9][10]
Pathophysiology
Neck pain pathophysiology is a complex combination of mechanical and chemical processes, which are yet to be fully understood. Pain cascade is initiated with tissue irritation which may be caused by a variety of factors such as trauma, infection, degenerative processes, over- or underuse, psychological factors, or a combination of the above. Nociception follows tissue irritation and often leads to more neck pain due to the compensatory postural strategies or activity avoidance. If not addressed, the process may become chronic.[4]
Evidence for Mainstream Medicine
The mainstream approach to nonemergent neck pain includes symptomatic management aimed at reducing nociception and inflammation with over the counter medications such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). A conclusion of 2007 Cochrane review was that “muscle relaxants, analgesics, and NSAIDs had limited evidence and unclear benefits” for treatment of mechanical neck issues.[4][11] Second-line agents such as selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, tricyclic antidepressants, anti-epileptics, and topical medications may be considered both in primary care and specialty care settings, but the current evidence for use of these medications for neck pain treatment is limited.[4]
Clinical experience with many patients has indicated that topical preparations may be an effective and safer alternative or adjunct to oral pain medications, as the topicals have much lower systemic absorptions rates (and thus fewer potential side effects) and are applied directly to the painful body area. It is reasonable to start with a single agent such as 5% topical lidocaine or 1% topical diclofenac and monitor the response. If the response is minimal or incomplete, it is reasonable to try a preparation containing a combination of several medications including any of the following: anti-inflammatory (diclofenac), anesthetic (lidocaine or bupivacaine), muscle relaxants (cyclobenzaprine or Flexeril). Adding a low-dose narcotic medication such as 5%-10% tramadol can have additional benefit and may help avoid starting oral narcotics. Using narcotic medications topically may be less habit forming, have less potential for abuse, and help reduce the overall dose of oral pain medications. Compounding pharmacies are available country-wide and some of them specialize in topical pain preparations. In general, pharmacists can help guide the clinician in helping choose appropriate ingredients and doses for a specific patient. It is important to remember that the same contraindications apply to the topical medications as to oral medications. Keep topical medications in mind as one option for neck pain care.
In contrast, oral or transdermal (i.e., fentanyl patches) opioid therapy for musculoskeletal neck pain is strongly discouraged. In rare cases when a measurable and sustained functional benefit can be demonstrated, low dose opioid therapy may be justified. The need for ongoing opioid therapy should be re-evaluated at each follow up appointment. There is currently no evidence that opioid use improves quality of life and pain levels or helps reduce the number of disability claims despite the 108% increase of use of opioids for treating spinal disorders between 1997 and 2004.[4][12]
Patients with persistent neck pain should be referred to Physical Therapy (PT) for evaluation and treatment. Specialty PT with focus on spine care is preferable. A 2014 review by O’Riordan found the best functional and quality of life outcomes with PT programs utilizing a multimodal approach, especially when active strengthening was emphasized. Even further benefits were seen when aerobic exercise and stretching were added to the PT regimen.[13]
If there is no significant improvement in neck pain symptoms, it would be reasonable to refer the patient to a physical medicine and rehabilitation physician (physiatrist) specializing in nonoperative spine care. The physiatrist can evaluate the patient for other potential treatment options, beyond what can be provided in the primary care setting, such as injection therapy.
Spinal injection therapy is widely utilized in the mainstream medical model. There is some positive evidence in favor of epidural steroid injections for neck pain in carefully selected patient population subsets, such as for people with neck pain and arm pain stemming from a herniated cervical disk.[4][14] Manchikanti et al. performed a systematic review and concluded that there was Level II positive evidence in favor of interlaminar epidural steroid injections (ESIs) in patients with post-operative, central spinal stenosis, disk herniation, and nonfacet discogenic pain.[15] Potential benefits versus risks of the ESIs should be carefully considered.[16]
Other types of imaging-guided neck injections include cervical facet medial branch blocks and radiofrequency ablation/neurotomy procedures (Level II positive evidence) and intra-articular facet joint injections (Level III positive evidence).[17]
Again, it is important to consider how and for how long the injection therapy would improve functional and quality-of-life outcomes before deciding to proceed. Potential complications and higher cost of these relatively invasive procedures should be considered relative to some of the less-invasive interventions. See the section titled “Injections for Neck Pain” below for a discussion regarding various other injection treatments that can benefit a neck pain patient population.
Surgical treatments should be considered in patients with neck pain who have operable conditions confirmed by imaging and/or symptoms of spinal cord or spinal nerve root compromise resulting in functional impairments such as losses of strength, coordination, or bowel and bladder control.[4][18] Research is inconclusive regarding the use of surgical treatments in the absence of the above circumstances.[4][19]
Proactive Self-Care and Neck Pain
Moving the Body
Getting a Veteran into a regular exercise program that is both enjoyable and compatible with his or her lifestyle is essential for addressing neck pain. Human bodies are designed for motion. Exercise is essential for re-establishing healthy movement patterns in the neck and surrounding areas, improving circulatory exchange of nutrients and removal of waste products, and also addressing the stress component, which is often a contributing factor.
In general, it is helpful to be aware of general exercise prescription guidelines for healthy adults when advising patients. The American College of Sports Medicine released an updated position statement in 2011 recommending that “most adults engage in moderate-intensity cardiorespiratory exercise training” such as brisk walking for at least 30 minutes per day at least 5 days a week for a total of at least 150 minutes per week. In addition to cardiorespiratory exercise, the individuals should do resistance and flexibility training as well as neuromotor exercise (balance, agility, and coordination) at least twice weekly.[20] These guidelines may be adjusted based on the specific patient’s goals and state of health. Refer to the “Prescribing Movement” Whole Health tool for further guidance on tailoring exercise to individual needs. Clinicians may also consider using the frequency, intensity, time (duration), and type (FITT) principle when advising the patients regarding exercise goals.[21]
In addition to the general exercise guidelines above, a variety of exercise modalities is available to help neck pain patients. The chin tuck is a simple exercise that can be taught to the patients. See Appendix 1. A systematic review by Gross et al. found moderate evidence that when white collar workers with chronic myofascial neck pain did something as simple as 2 minutes of scapulo-thoracic endurance exercises daily for 10 weeks, there was measurable improvement in neck pain reported over the course of the previous week by every fourth participant.[22] The authors felt that these result warranted recommending this approach for the office workers. Interestingly, the same review did not find evidence that using a soft collar had any long-term benefit for neck pain patients.
Physical Therapy
As mentioned previously, Physical Therapy (PT) is an excellent starting point for patients with neck pain.
Ergonomic Interventions
A Cochrane Review by Verhagen and colleagues concluded that there was at best low-quality evidence to support ergonomic interventions for long-term but not short-term pain reduction.[23] More research is needed. It is reasonable to consider a trial of sit-to-stand work space for patients with persistent neck pain. For recommendations regarding proper body mechanics during computer work while sitting or standing, please visit United States Department of Labor Occupational Safety and Health Administration website page on good working positions.[24]
Yoga
There is evidence that yoga can be beneficial for patients with neck pain. Please refer to the “Yoga” Whole Health tool for details. The American Pain Society released a statement in 2012 that yoga is effective for treatment of neck pain.
A systematic review by Crow et al. found Iyengar/alignment-based yoga to be more beneficial when compared to control treatments for short-term relief of both low back and neck pain. Control treatments included no interventions, educational materials, standard care, a home exercise program.[25] A randomized controlled trial (RCT) examined the same population and concluded that Iyengar yoga was superior compared to a home exercise program in regard to severity of neck pain, quality of life, and neck pain related disability.[26] A subgroup of the above patients also took part in a qualitative study that found that participating in a yoga intervention resulted in improved body awareness, greater pain coping abilities, and increased sense of control over health.[27]
Alexander Technique, Feldenkrais Method, and Pilates
All three of the therapeutic modalities described here were developed by and named after the individuals who discovered and perfected these techniques through the course of their own healing journeys.
Both Feldenkrais Method and Alexander Technique teach greater body awareness through movement.
Alexander Technique utilizes postural adjustments of various body areas, including the head and spine, to help rebalance the body. Pain relief is not a specific focus of Alexander Technique, but it may result from improved body alignment.
Feldenkrais Method uses physical movement to address imbalances and dysfunctions in the nervous and musculoskeletal systems which over time may lead to increased pain and disability. This therapeutic modality focuses on improving joint range of motion without flaring up painful symptoms and re-integrating the body and the mind.[28]
The Pilates Exercise Method is very popular and is offered throughout the country in a variety of settings, including in many health clubs, hospitals, and private studios. The focus of this modality is on the core muscles of the back and the abdomen, precise positioning, and proper breathing technique. Pilates method may also utilize specific equipment to help speed up therapeutic process.[28]
There is limited research regarding the specific effects of the above three modalities on neck pain specifically, but new data is continuing to emerge. A 2015 RCT showed that when either acupuncture or Alexander Technique were combined with usual care, there was a significant improvement at 12 months in neck pain and disability scores compared to usual care alone. Authors of another 2015 RCT found no difference between disability scores, use of pain medications, or pain levels in the patients treated with Alexander Technique compared to those treated with heat application or Guided Imagery. However, significant difference was found in favor of Alexander Technique in regard to general health, physical function, and preference for Alexander Technique as a treatment modality, which may be an important factor in ongoing adherence to treatment.[29]
A 2015 quasi-RCT found that both yoga and Pilates were similarly effective and more effective in reducing neck disability index and pain scores when compared to controls. No difference in posture or range of motion was detected between treatment groups versus controls.[30]
It is important to note that Alexander Technique, Feldenkrais Method, and Pilates are becoming wider used among individuals with chronic pain, have been shown to be beneficial for various musculoskeletal conditions, and are generally safe.[4][31][32][33] There are some isolated case reports of adverse effects following Pilates classes.[34][35][36] More research is needed, but it is unlikely that the risk exceeds the potential adverse effects of other mainstream therapeutic movement modalities. Most common side effects include temporary increases in muscle soreness and pain.[29]
Tai Chi and Qi Gong
Tai chi and qi gong both have elements of mindful movement and breathing awareness. They are sometimes categorized under bioenergetic therapies as well.[4] Tai chi was an ancient Chinese martial art that evolved into a form of exercise.[37]
According to the National Qigong Association, qi gong is a synergy of “physical postures, breathing techniques, and focused intentions.”[38] Qi gong has origins in fighting arts as well, and can be further subdivided into internal and external forms. According to Chan et.al, internal qi gong is “self-directed” and uses “movements, meditation, and control of breathing pattern…to achieve a harmonious flow of energy (qi) in the body so as to improve physical fitness and overall well-being.” External qi is energy directed from trained practitioner to patient in order to accomplish a therapeutic effect.[39]
There is existing research showing that tai chi can help with fibromyalgia pain, osteoarthritis pain and functional status, and chronic low back pain. [40][41][42][43]
Higher quality studies examining effects of tai chi and qi gong on neck pain are beginning to emerge but continue to be limited.
A 2015 systematic review and meta-analysis by Yuan concluded that both tai chi and qi gong may have fair efficacy in regard to chronic neck and low back pain, but more research was necessary to draw more definite conclusions.[44] Qi gong was found to be no better than physical therapy or being placed on a wait list in a 2009 systematic review.[45] Interestingly, a subsequent 2015 systematic review showed that internal qi gong had benefits for treatment of some chronic pain compared to controls, while external qi gong did not.[46]
Another systematic review by Gross and colleagues found moderate evidence that qi gong was beneficial for one in every 4 to 6 patients with chronic neck pain when short-term pain and function were the outcome measures.[22]
Power of the Mind
Patients’ experience of pain is subjective and does not always correlate with the severity of underlying pathology. For instance, multiple studies have examined cervical spine magnetic resonance imaging (MRI) in symptom-free subjects and found that up to one-half of these individuals had findings of at least one bulging disk. The number of asymptomatic disk bulges was even higher in individuals over the age of 60up to 80%.[4][47] Also, despite the wide prevalence of degenerative changes in the cervical spine among people age 70 and older, not everyone in this population develops neck pain.[3][4]
Development of neck pain is correlated to the individual’s emotional health.[48] A large population study found a stronger association between neck pain levels and emotional stress than with repetitive work activities.[49] Another study found that patients’ psychological status correlated with pain presence and intensity, while severity of MRI findings did not.[50] Furthermore, the presence of catastrophizing, somatization, or perceived lack of control make the development of chronic pain more likely.[4][51][52][53] Bottled up emotions, especially unexpressed anger, can also manifest themselves as pain.[54] Therefore, addressing the individual’s emotional health becomes critical for successful pain management. Multidisciplinary approach utilizing a variety of techniques in both individual and group setting can provide the patient with a set of tools that work best for him or her.
Please refer to the following modules for additional information: “Self-Management of Chronic Pain” and “Mindful Awareness.”
Mindfulness- and Acceptance-Based Interventions
A 2016 meta-analysis by Veehof et al. examined the effects of Mindfulness-Based Cognitive Therapy (MBCT), Mindfulness-Based Stress Reduction (MBSR), and Acceptance and Commitment Therapy (ACT) on various pain-related measures (quality of life, depression, anxiety, disability, pain severity) in the chronic pain population. ACT appeared to be more effective for depression and anxiety compared to MBCT and MBSR. The authors concluded that although all three interventions (MBSR, MBCT, and ACT) were no better than the standard cognitive behavior therapy (CBT) pain treatment protocols, they could be an effective alternative.[55] More data is needed regarding the effects of these three modalities on neck pain specifically.
The Role of the Diaphragm
There is an important connection between stress, diaphragm movement and breathing patterns, and development of myofascial pain, including neck pain. There is emerging evidence that the diaphragm plays a role in pain modulation, although further research is needed.[56] Bordoni and Zanier argue that the diaphragm is not just a respiratory organ, but that it also plays an important role in posture and has connections to roof of the mouth, cervical spine, trigeminal system, thoracic outlet, and pelvis as well as to the lymphatic and vascular systems, among others.[57]
When the diaphragm is not moving properly, we tend to recruit secondary muscles of respiration (i.e., sternocleidomastoid, upper trapezius, scalenes, and others) which can lead to neck muscle imbalance and subsequently pain.[58] There is now research showing that respiratory re-education can improve respiratory function and neck range of motion as well as decrease use of accessory respiratory muscles, and decrease neck pain levels.[59]
Keeping in mind all the information above regarding the diaphragm, one can see the utility of breathing exercises, manual adjustments, and other strategies for patients with neck pain. These approaches can help normalize diaphragmatic movement patterns and thus reduce strain on other structures which may be contributing to neck discomfort.
Other Psychological Treatments
A 2015 systematic review by Shearer et al. concluded that there was no strong positive or negative evidence that either relaxation techniques or Cognitive Behavioral Therapy (CBT) improved disability or pain severity in patients with neck pain disorders. Likewise, there was mixed evidence for use of CBT and lack of definitive evidence to support use of relaxation techniques or biofeedback in whiplash patients. More high-quality research was recommended.[60]
However, another 2016 review that did not specifically focus on neck pain concluded that psychological interventions were vital for treating chronic pain in general. CBT was thought to be most beneficial, followed by biofeedback. Exercise interventions produced benefits in pain states of various durations.[61]
Given low potential for side effects, it would be reasonable to recommend a trial of CBT for patients with persistent neck pain resistant to other treatment modalities.
Hypnosis
Research shows that hypnosis can help with chronic pain.[62][63] One study found that hypnosis intervention was slightly more effective than acupuncture for chronic head and neck pain. Receiving healing prompts by an audiotape had an additional benefit for pain reduction.[64]
Journaling
A 2014 study found that physical therapy intervention was more effective for musculoskeletal pain when supplemented with expressive writing about stressful life events. Furthermore, the writing group continued to derive pain reduction benefits 6 months after the interventions, and also had better posture and emotional self-awareness and scored lower on a psychopathology scale.[65] Therapeutic writing may also have a role in reducing pain and inflammation in rheumatoid arthritis patients.[66] Further research regarding the effects of therapeutic writing on neck pain is needed.
Guided Imagery
According to the Academy for Guided Imagery website the term “Guided Imagery” “refers to a variety of techniques, including simple visualization and direct suggestion using imagery, metaphor and storytelling, fantasy exploration and game playing, dream interpretation, drawing, and active imaginations where elements of unconscious are invited to appear as images that can communicate with the conscious mind.” One study found that an emotionally triggering “index image” was present in more than three-fourths of chronic pain patients. When this image was recalled, negative feelings and pain levels increased.[67] Another study found a positive correlation between catastrophizing and higher pain levels in whiplash patients.[68]
A 2011 systematic review by Posadzki pointed out that 8 out of 9 randomized controlled trials (RCTs) found a positive effect of Guided Imagery on musculoskeletal pain. More rigorous RCTs would be required to draw more definitive conclusions.[69]
Nevertheless, Guided Imagery as well as other techniques that can help transform stress-inducing images into more positive ones (including techniques like motivational interviewing, CBT, hypnosis, journaling, and neurolinguistic programming) appear to have an important role in treating pain, including neck pain.[4][67]
Art, Music, and Literature Therapy
Research suggests that the above modalities improve overall well-being and facilitate relaxation.[70] There is evidence that patients with a prior history of psychological trauma may benefit from art therapy, especially when it comes to depression.[71] This may be particularly relevant for Veterans. More research is needed before conclusions can be made regarding the benefit of the above treatments for the neck pain population specifically.
Aromatherapy
Sense of smell can help bridge the connection between the body and the mind. Emerging research shows that aromatherapy can be helpful in a variety of painful and unpainful conditions and is generally well tolerated. It can be a good alternative for populations (i.e., geriatric patients, etc.) who are at higher risk for side effects with standard therapies.[4] One specific RCT found significant improvement in neck pain scores and neck disability index when patients used a topical cream containing lavender, marjoram, black pepper, and peppermint, when compared to use of the placebo cream.[72]
According to Natural Medicines Database, “Early research suggests that impression of pain intensity and unpleasantness may be reduced after treatment with lavender therapy.”[73] Additionally, lavender may have a short-term benefit for low back and neck pain when combined with acupressure or massage, respectively. Some of the contraindications include sensitivity to lavender, history of seizures, bleeding disorders or anemia, and eating disorders.
Other Therapies
Acupuncture
In the practice of acupuncture, needles are used along the body’s energy channels (meridians) to help optimize energy flow.[4] There is some emerging evidence that acupuncture treatments may benefit patients with neck pain.
Furlan et al. found the following in a 2012 systematic review[74]:
- Acupuncture reduced pain intensity (measured by McGill pain questionnaire) significantly more compared to no treatment in subjects with myofascial neck pain of unspecified duration in one trial.
- The difference between acupuncture and sham acupuncture was not statistically significant immediately post-treatment in the individuals with specific or nonspecific chronic neck pain.
- Results of studies measuring pain relief after acupuncture versus pain medications were inconsistent. The same was true when pain scores where compared post-spinal manipulation vs. post-acupuncture. Disability scores were actually better in the manipulation group in the individuals with chronic nonspecific neck pain. One trial found acupuncture to be more effective than massage for short-term pain reduction.
Yuan and colleagues concluded that there was moderate evidence in favor of acupuncture over sham acupuncture for pain relief measured by visual analogue scale immediately and one month after treatment in patients with chronic neck pain.[44]
There is currently limited evidence regarding efficacy of acupuncture for acute neck pain.[4] Evidence continues to be limited regarding use of acupressure, auricular acupuncture, or electroacupuncture for neck pain patients.[44]
A systematic review/meta-analysis by Graham et al. found moderate evidence in favor of acupuncture, laser therapy, and intermittent traction for short-term relief of chronic neck pain. There was moderately good quality evidence showing no benefit of the following modalities: continuous traction, pulsed ultrasound, or infrared light in regard to acute whiplash associated disorder, neck pain ranging in duration from subacute to chronic, or chronic myofascial neck pain.[75]
For patients with cervical radiculopathy, acupuncture was found to be more effective than traction, although the quality of evidence was low.[76] The same authors also mentioned that acupotomy treatment was found to be more effective than acupuncture in a meta-analysis, although the quality of data was also low so no strong conclusions could be drawn.
Acupotomy is a more invasive variation of acupuncture therapy. Knife-sharp needles are used during acupotomy treatments and are inserted along the acupotomy points and also in the areas of tenderness. One of the goals is to help heal tissue adhesions and restore normal tissue movement.[77] Notably, there was at least one report of a fatal pharyngeal hemorrhage after acupotomy. [78] More research would be needed before acupotomy treatments could be recommended for neck pain or other indications. Given that this is a more invasive form of acupuncture treatment with higher potential for side effects, this type of treatment is not recommended. Rather, advise that the patients pursue more traditional, less-invasive forms of acupuncture for treatment of radicular and nonradicular neck pain.
Please refer to the “Whole Systems: Chinese Medicine and Acupuncture,” Chapter 18 of Passport of Whole Health for additional information on the theory behind acupuncture, its mechanisms of actions, and research findings related to other health conditions.
Energy Medicine/Biofield Therapies
Biofield therapies, including Reiki, Healing Touch, and many others, do not have clearly understood mechanisms of action.[79] According to Gonella et al., Biofield therapies (BTs) “are believed to balance out disturbance in the energy field caused by physical and psychological symptoms”.[80] Even though there are currently no studies examining the effects of BTs on neck pain specifically, positive data are starting to emerge regarding the use of these modalities for cancer-related symptoms including physical symptoms such as fatigue and pain, as well as psychological symptoms such as anxiety, and overall quality of life.[80] Similar trends are emerging in studies of end-of-life care.[81] A nonrandomized pilot study by Notte et al. found that Reiki Therapy significantly reduced pain (but not the amount of pain medication) in patients who underwent a total knee replacement procedure compared to a control group.[82]
A 2014 review by Hammerschlag found that a significant benefit for at least one primary outcome was observed when nontouch BTs were used.[4][83] Given that the risk of side effects with BTs is minimal, it is reasonable to incorporate this modality into the treatment program as long as it is not used as a substitute for other life-saving therapies. Please refer to “Energy Medicine: Biofield Therapies,” Chapter 17 in Passport to Whole Health for additional information.
Other Considerations
Like with most pain complaints, it is important to look at the bigger picture and not assume that the cause of musculoskeletal neck pain is originating from the neck itself.[4] Structural disturbances and/or restrictions above or below the neck region can result in compensatory strategies that ultimately trigger neck discomfort. At the basic structural level, one of the body’s and the neck’s main functions is to keep the eyeballs level. Body structures are intimately connected from top to bottom through intricate connective tissue/fascial networks.[84] Thus, something as distal in the body as an ankle sprain may actually lead to a sore neck. Potential contributions of abnormal diaphragmatic movement to development of neck pain were discussed earlier in this overview.
Manual Medicine
The term “manual medicine” refers to a variety of hands-on therapeutic techniques designed to rebalance and realign musculoskeletal, connective, visceral, and other body tissues in order to ensure optimal body function. Manual modalities are commonly used for treatment of neck pain.
Many different health professionals, including physical and massage therapists, chiropractors, osteopathic and traditional/Western medicine physicians, and naprapaths, incorporate numerous manual techniques into their treatment regimens. Techniques can vary greatly among different categories of providers, but there can be also a significant overlap.
One way to categorize manual medicine techniques is into high- versus low-velocity maneuvers.[4] Often, the term “manipulation” is used to refer to high velocity, low amplitude (HVLA) techniques, while the term “mobilization” describes lower velocity, gentler engagement of the joints.[4][85] Osteopathic physicians group more than a hundred different techniques under the umbrella of Osteopathic Manipulative Treatment (OMT), and those are further categorized into different groups, including cranial osteopathy, muscle energy, myofascial release, strain-counterstrain, and many more.[86]
Refer to Passport to Whole Health Chapters 16 “Manipulative and Body-Based Practices” and 18 “Whole Systems of Medicine”.
Most adverse effects associated with manual therapies have been studied in the context of HVLA techniques, since those are considered to be the riskiest. Adverse effects may occur in up to two-thirds of patients and are usually short-lived (less than 24 hours). They may include worsening pain, fatigue, headache, and radicular pain.[4] Disk herniation can worsen after manipulation and is therefore a potential contraindication to manual treatment.[4] Additional contraindications to HVLA treatment of the cervical spine include structural abnormalities of the vertebral arteries; carotid artery disease; fracture; ligamentous instability; infection; primary or metastatic tumors of the neck; low bone density (osteopenia and osteoporosis); previous neck surgery (i.e., fusion or others); anticoagulation; rheumatoid arthritis (RA); and atlantoaxial instability, which can be seen in RA and congenital conditions such as Down syndrome.[4]
In general, manipulations are considered safe when administered by trained professionals and when compared with the side effect profiles of other mainstream treatments, such as anti-inflammatory drugs.[4]
Research studies examining manual medicine carry unique challenges, given the need for individualizing treatment protocol to accommodate unique needs of specific patients and the issue of creating a comparable placebo treatment.[4]
- According to Gross et al. Cochrane Review, there are three mechanisms by which spinal manipulation and mobilization may work[85]: Mechanical effects on the tissues
- The effects on the physiological properties of both autonomic and peripheral nervous system, including analgesia
- Psychological effects of manual touch including placebo effect
An updated 2015 Cochrane review concluded the following:
- Single cervical manipulation provided immediate relief only for subacute and chronic neck pain compared to inactive control treatment. Multiple sessions of cervical manipulation were similar in efficacy to cervical mobilization in regard to quality of life, pain, and functional outcomes for acute and chronic neck pain. They were more effective compared to some medications for acute and subacute neck pain in regard to pain and functional outcomes at immediate and long-term follow up. They were more effective than massage therapy for chronic cervicogenic headaches at short- and intermediate-term follow up, and they were more effective than thoracic manipulations for acute neck pain in regard to function and pain at short and immediate follow up.
- Thoracic manipulations improved acute and subacute neck pain compared to inactive controls and improved function in acute and chronic neck pain patients. Thoracic manipulation may be similar in efficacy compared to thoracic mobilization but better quality research is needed.
- “Given the risk of rare but devastating adverse events linked to cervical manipulation, cervical mobilization may be the technique of choice when treatment of cervical region is needed.”
- Thoracic manipulation and mobilization were both thought to be reasonable neck pain treatment options.
Injections for Neck Pain
Epidural steroid injections (ESIs) have, as mentioned previously, a role in treating neck pain in carefully selected patient populations who do not respond to more conservative measures. In addition to the more interventional techniques described above, other injection techniques can also be utilized for treatment of neck pain resistant to more conservative approaches. It is important to remember that injections should only be one part of the multidisciplinary treatment protocol and will likely have limited efficacy when used alone.
Trigger point injections are often added to the treatment protocol by the patient’s primary care or musculoskeletal medicine clinician. Trapezius muscle trigger points are among the most easily identifiable and safe injection targets, when provided by a skilled clinician. Needling at the time of the injection and ischemic compression for 30 seconds immediately after the procedure appear to be important for optimizing the therapeutic effect.[87][88]
A study by Wang et al. found that lidocaine injections targeting the intramuscular innervation zone in the trapezius muscles appeared to be more effective compared to simply injecting palpable trigger points.[89]
There is some positive evidence regarding using botulinum toxin A injections for myofascial and musculoskeletal neck pain, but additional research is needed before drawing definitive conclusions. Cost of the botulinum toxin A can be a limiting factor.[90][91]
There is little research support for the use of Regenerative Injection Therapy such as Prolotherapy, Platelet-Rich Plasma, and Stem Cell Therapy injections in people with neck pain. Regenerative medicine is still in its early stages, but given positive evidence regarding the utility of Prolotherapy injections for the knee osteoarthritis population, it is reasonable to anticipate that future high-quality research will help define the utility of the novel regenerative therapies for people with neck pain, as well as those suffering from other chronic conditions.[92]
Food and Drink
Making positive dietary changes may not be easy or quick but will definitely have a beneficial impact on the individual’s overall well-being, including symptoms of pain. Anti-inflammatory diets can be described as “whole food-based nutrition that emphasizes omega-3 fats, vegetables and fruits, high fiber, whole grains, and healthy proteins”.[93] The Mediterranean diet is an example of an anti-inflammatory diet. Refer to the “Choosing a Diet” Whole Health tool for more information.
The importance of vegetable and fruit consumption in place of processed and/or foods high in refined sugars cannot be emphasized enough. Eating 5 to 9 servings of vegetables and fruit per day is crucial (more than half of those servings should come from vegetables). Deeply colored fruits and vegetables have more phytonutrients. The goal is to eat a “rainbow” of colors throughout the day. Vegetables should account for at least a half the food on a person’s plate for most of their meals.[93]
In addition to nutritious food, adequate hydration is essential for optimizing the body’s overall function, including circulation of oxygen and nutrients, as well as waste removal. Common advice regarding water intake includes drinking eight 8ounce glasses of fluid per day or drinking the equivalent of half your weight in pounds in number of ounces of fluid (i.e., a 160-lb individual would drink 80 oz of fluids per day). However, there is no perfect formula that fits every individual. Fluid needs may vary depending on the temperature of the surroundings, activity levels, medical status, etc. According to Mayo Clinic recommendations, one should drink enough fluids to rarely feel thirsty and to keep the urine looking colorless or just slightly yellow.[94] Excessive fluid intake has health risks and should also be avoided.
In general, it is best to choose beverages that do not contain added sugar or artificial ingredients. Pure water is an excellent choice, but a variety of other healthy options is available. The “What We Drink” “What We Drink” Whole Health tool offers additional information.
Supplementing the Diet
While it is best to obtain all the essential nutrients through food, it is not always practical or possible. “High-yield” foods, minerals, and nutritional supplements are discussed below.
Omega-3 Fatty Acids
Western diet tends to be high in proinflammatory omega6 fatty acids and relatively poor in anti-inflammatory Omega 3 fatty acids. The ideal omega-6 to omega-3 ratio is approximately 2:1 compared to the typical American diet ratio of 10:1 and up.[93] Increasing consumption of omega-3 fatty-acid-rich foods, while decreasing omega-6 rich foods, can help shift a person’s metabolism toward a less inflammatory state and yield numerous health benefits.
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) have stronger anti-inflammatory properties than their precursor alpha-linolenic acid (ALA). EPA and DHA should be preferentially increased in the diet. The acronym SMASH can be used to remember excellent sources of EPA and DHA: salmon, mackerel, anchovies, sardines, and herring.[93] Preference should be given to fish that is wild-caught in a sustainable way from a clean geographic region.
Most people do not get enough omega-3s from the diet. Fish oil capsules are often standardized to EPA/DHA content, and recommended daily dosing of EPA/DHA can vary from 0.5-1 gm to as much as 8 gm.[93][95]
Generally, fish oil is considered to be well-tolerated at doses of 3-4 gm per day of total fish oil.[95] However, it is important to remember that the risk of side effects is higher with increasing doses. Diarrhea and gastrointestinal upset are the most common side effects. These can be minimized by gradual dose increases and by taking the supplement with meals. Fish oil capsules can also be frozen prior to consumption to minimize “fishy” aftertaste.[95] According to the Therapeutic Research Center (TRC), “Intake of 3 gm or greater of omega-3 fatty acids daily may inhibit platelet aggregation and increase the risk of bleeding,” and caution should be used in with certain patient populations.[95]
Vitamin D
A 2015 Cochrane review found no consistent evidence to support vitamin D treatment in patients with various chronic pain conditions of over 3 months’ duration. Further investigation was recommended before conclusions could be drawn regarding vitamin D supplementation and specific types of pain.[96]
A recent RCT examined the effects of adding 4,000 IU of vitamin D3 compared to placebo to the analgesic medications in patients with musculoskeletal pain. It was found that vitamin D3 group had significantly lower pain scores as measured by Visual Analogue Scale (VAS), lower need for “rescue” analgesics, as well as lower measured serum levels of several pain and inflammatory cytokine markers.[97]
Given the current evidence regarding beneficial effects of vitamin D supplementation on bone mineral density, fall prevention, mood disorders, and overall mortality reduction, it may be important to screen for and correct vitamin D deficiency (commonly defined as levels below 30 ng/ml) to at least the low-normal or mid-normal range in patients with neck pain resistant to other treatments.[95]
Magnesium
Magnesium is an essential mineral that plays a role in over 300 cellular reactions.[95] It is required for “bone, protein, and fatty acid formation, hematopoiesis, muscle contraction, clot formation, and synthesizing ATP,” among other functions. Magnesium works in concert with potassium, sodium and calcium to ensure proper muscle tone and contractility (Parcell). If one of these ions is out of balance, e.g., in the case of mild or frank deficiency, muscles can become hypertonic and painful.[98] Measuring levels of magnesium in the red blood cells rather than in the serum may be more sensitive for detecting magnesium deficiency.
According to the NMD, there is evidence that magnesium is “possibly effective” for chronic fatigue syndrome; fibromyalgia-related pain, tenderness, and depression; pre-menstrual migraine and other PMS symptoms; post-operative pain and cancer-related neuropathic pain.[95] A 2016 study found that magnesium levels are significantly lower in the migraine sufferers between and during migraine episodes.[99]
More research is needed before specific conclusions can be drawn regarding using magnesium for the neck pain population. It would be reasonable to try magnesium supplementation for people with myofascial neck pain complaints that are resistant to first-line approaches. Foods that are rich in magnesium include high-fiber foods such as whole grains, legumes, vegetables.[95] Many clinicians choose to recommend supplementing additional magnesium beyond the diet. Recommended dosing is 400-800 mg per day. Magnesium glycinate and citrate forms are better tolerated and absorbed and cause less gastrointestinal upset compared to magnesium oxide or hydroxide. Another good way to supplement magnesium is by taking an Epsom salt bath or using a topical magnesium cream. These approaches may have additional benefits due to relaxation in warm water or doing self-massage.
Renal disease is a common contraindication to magnesium supplementation. Potential drug interactions should be taken into account as well.
Anti-Inflammatory Herbs, Spices, and Other Agents
Herbal extracts in the form of supplements can provide additional benefit beyond dietary changes alone. Some of the herbs below can also be eaten as part of the daily diet.
The list below will focus on some of the more well-researched agents.[95]
Turmeric (Curcuma longa) is an excellent anti-inflammatory spice that is rated as “possibly effective” for osteoarthritis (OA) symptoms including pain and function by the NMD and should be considered in neck pain patients who have findings of OA. It has been shown to be comparable in efficacy to nonsteroidal anti-inflammatories (NSAIDs) and helped reduce NSAID use in some studies.[95] Common starting doses are 500 mg of turmeric (standardized to curcumin content) three times daily; the dose can be doubled as tolerated. Taking turmeric with black pepper may improve absorption. Possible side effects of turmeric include increased stomach acid production, hypoglycemia, and prolonged bleeding time.
Boswellia or Indian Frankincense (Boswellia serrata) is also rated “possibly effective” by NMD for improvement of OA-related pain and function. There are combination products that use both Turmeric and Boswellia.[95] Boswellia extract is commonly dosed at 200-400 mg three times daily. Improvement can be seen as soon as 7 days after starting the supplement. Side effects are uncommon and are mainly gastrointestinal.
Other Herbs and Spices
Other plant-based agents that have been rated as “possibly effective” or having “good evidence” for OA-related symptoms by NMD include cat’s claw (Uncaria tomentosa), devil’s claw (Harpagophytum procumbens), ginger (Zingiber officinale), and rose hips (from Rosa canina subspecies).
Some of these preparations, including willow bark (Salicis cortex) were found to be helpful for low back pain. This herb is rich in salicylates and was found to have a dose-dependent effect for the patients with back pain. Devil’s claw was also found to be helpful for low back pain in some studies.
Other Agents: Glucosamine and Chondroitin
Singh et al. conducted a 2015 systematic review on use of chondroitin in OA and concluded that, “A review of randomized trials of mostly low quality reveals that chondroitin (alone or in combination with glucosamine) was better than placebo in improving pain in participants with osteoarthritis in short-term studies.” [100]
For all of the preparations above, data regarding neck pain and musculoskeletal pain continues to be absent, limited, or suboptimal quality and further educational studies are needed.
Recharge
Although research regarding the effects of sleep specifically on neck pain is lacking, getting restful sleep on a daily basis is essential for optimizing one’s physical and mental well-being. Decreasing or eliminating caffeine intake, especially toward the end of the day can be very helpful. Avoiding alcohol can also encourage more restful sleep.
Refer to the “Recharge” Whole Health overview for additional information on the value of recharging in general.
Spirit and Soul
There are several underlying themes that come up when trying to define what spirituality is:
- Connecting to something bigger than just ourselves
- Searching for and expressing meaning and purpose in life
- Any experience that allows the individual to experience the divine
In many cases, spiritual pursuits become most relevant during times of emotional or physical stress, such as facing a serious illness, death, or grief.[101] A more specific example of a highly stressful situation would be a Veteran who had to face the possibility of devastating injuries or death on a daily basis.
Although research specifically regarding neck pain is lacking, there are studies showing that contemplative practices such as meditation, prayer, yoga, and journaling are associated with better quality of life and improved health outcomes. For example, mindfulness meditation research showed a significant positive correlation between a regular mindfulness practice and immune function, increased pain tolerance, and maintaining better quality of life in a setting of chronic illness or difficult life situations. There was even a study showing that regular meditation practice was associated with a decreased inflammatory response and decreased activity of genes that turn on inflammatory pathways.[102][103] A study by Kabat-Zinn et al. found statistically significant benefits of mindfulness meditation for the chronic pain population for the following measures: mood disturbances, activity levels, body image, and pain in the present moment.[104]A meta-analysis by Lucchetti et al. found that people with strong spiritual and/or religious lives had at least an 18% reduction in mortality, comparable to benefits of eating a diet rich in fruits and vegetables or taking a statin medication.[105]
Spiritual practices may also provide people with additional supportive networks within their communities, which may further improve the individuals’ well-being, compliance with treatment plans, and health outcomes.
A brief and tactful assessment of the patient’s religious and/or spiritual background and needs can help enhance the interaction between the patient and the practitioner. It can also give the health care clinician some additional clues regarding the best course of treatment for the patient based on the patient’s religious or spiritual practices.[106] The Spirit and Soul portion of the PHI questionnaire helps start this important conversation. The “Spirit & Soul” Whole Health overview offers additional information about this topic.
For the Whole Health topics and modules “Personal Development,” “Surroundings,” and “Family, Friends & Co-Workers,” specific research related to neck pain is limited. However, please refer to these relevant Whole Health overviews, which describe how these three areas impact individuals’ health. For example, in terms of surroundings, smoking is positively associated with presence of chronic pain. Patients with neck pain should be strongly encouraged to minimize or quit smoking.[107]
Appendix 1:
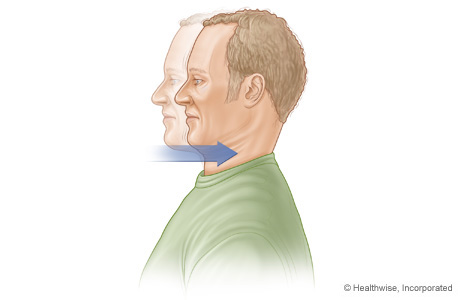
The chin tuck exercise can be a good place to start and can help strengthen and stretch the neck extensor muscles that are often overworked in patients with neck pain, especially the ones with poor postural habits.
This can be done seated or standing with the back against the wall. The patient should keep the mandible level and glide the chin straight back gently until some resistance is encounter. This should be repeated as often as every hour, with 3 repetitions, held for 3-5 seconds each.
Back to Michael
Personal Health Plan
Name: Michael
Date: xx/xx/xxxx
Mission, Aspiration, Purpose (MAP):
- To improve my physical and emotional well-being and life satisfaction through making positive changes in my daily life. To be able to enjoy more quality time with my friends, family, and especially my daughter. To dedicate time to activities that make me feel happy and fulfilled.
My Goals:
- Start a regular exercise program
- Improve nutrition
- Make regular restful sleep a priority
- Consider pursuing a career that’s more in line with my passions and interests in life
Strengths (what’s going right already)/Challenges:
- I have a good relationship with my family and friends. I have a wonderful daughter who makes me want to be my best self for many years to come.
- I am open to trying different strategies to help address my neck pain and other concerns.
My Plan for Skill Building and Support
Mindful Awareness:
- Begin to work with the team to help stay focus on my mission and health goals
Areas of Self-Care:
- Moving the Body
- Take the family for a brisk 30-minute nature walk at least 5 days per week.
- Start jogging at least 2 times per week 5-10 minutes at a time. Increase duration and frequency gradually as tolerated.
- Consider other enjoyable physical activities and consider incorporating them into exercise routine on a regular basis. In the future, incorporate stretching, strength and resistance training into weekly exercise program.
- Consider simple ways to incorporate more activity into my work day, such as taking stairs instead of elevators, taking a walk during lunch, getting up from my work station to pick something up from a printer, etc.
- Surroundings
- Spend time in nature 2-3 times per week or more. Try to incorporate time in nature into my regular walks to help unwind after a stressful day and promote better relaxation and sleep.
- Go fishing at least once before next appointment.
- Personal Development
- Meet with a career counselor to discuss law enforcement education.
- Seek input from trusted family members or friends regarding which career field would best suit my strengths and talents.
- Food and Drink
- Pack healthy lunches to take to work.
- Ask wife for help.
- Replace afternoon soda with a green tea.
- Aim for 5-9 servings of fruit and vegetables per day (preferably more vegetables). Give preference to deeply colored fruits and vegetables. The goal is to “eat the rainbow.”
- Recharge
- Aim for at least 7-8 hours of sleep every night. Go to bed by 10:30 pm every night. Once caught up on sleep, will feel more energized and more likely to participate in family and work life with more enjoyment
- Family, Friends, and Co-Workers
- Aim to spend more time with wife and daughter during regular walks.
- Also, make some time to be alone or with a favorite friend or friends.
- Spirit and Soul and Power of the Mind
- Take a minute every day to check in with body, mind, and spirit and to acknowledge the way things are.
- Consider journaling about what is discovered, to discuss at next appointment.
Professional Care: Conventional and Complementary
- Prevention/Screening
- Up-to-date.
- Treatment (e.g., conventional and complementary approaches, medications, and supplements)
- Medications/Supplements
- Continue current medications (Tylenol as needed, ibuprofen as needed, nortriptyline at bedtime)
- Add turmeric 500 mg three times daily. Increase to 1000 mg three times daily after 1 week if tolerating.
- Add magnesium glycinate or citrate 500 mg daily. In addition to taking magnesium by mouth, consider an Epsom salt bath in the evening (2 cups of Epsom salt dissolved in a tub of comfortably warm/hot water, soak for 20-30 minutes).
- Skill Building and Education
- Chin tuck exercise taught to the patient; handout provided.
- Good sitting mechanics discussed. Printed the patient a handout from United States Department of Labor Occupational Safety and Health Administration website
- Patient Handouts on sleep, nutrition, exercise, and spirit and soul.
- Advised keeping a brief diet, sleep, and activity journal to bring to the follow up appointment
- Patient encouraged to call with any questions or concerns that may arise before the scheduled follow up
- Medications/Supplements
Referrals/Consults
- Return to PT (will request PT with a clinician specializing in spine-related complaints)
- Referral to health psychology to learn different relaxation strategies, including relaxation breathing
Community
Resources
My Support Team
- Principal Professions
- Primary Care Clinician
- Physical Medicine and Rehabilitation Medicine Physician
- Personal
- Wife
- Daughter
- Friends, Steve and Ryan
Please Note: This plan is for my personal use and does not comprise my complete medical or pharmacological data, nor does it replace my medical record.
Follow Up (Next Steps)
Michael was encouraged to follow up in two months. At that time, his clinician will go over his diet, sleep, and activity journal. Depending on progress with PT, other modalities (such as qi gong, osteopathic manipulations, trigger point injections, etc.) might be incorporated into his Personal Health Plan. His clinical team can revisit trying an acupuncture treatment again. Depending on the patient’s progress at follow up his clinician might also consider fish oil supplementation and checking a vitamin D level, with supplementation as needed.
Author(s)
“Neck Pain” was written by Alexandra Ilkevitch, MD, and updated by Vincent Minichiello, MD. (2016, updated 2019)



















