Office of Health Equity
Health Literacy to Achieve Health Equity in Minority Veterans
|
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially, ethnically, and socioeconomically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA health care mission. The Office of Health Equity (OHE) champions the elimination of health disparities to achieve health equity for all Veterans.
ELIMINATING DISPARITIES
Health literacy refers to how well an individual understands their health condition and information provided by health care providers. Health literacy is important because if patients and providers cannot communicate with each other in a way they both understand, an incorrect diagnosis or treatment plan may be made, and individuals might not know what they should do to manage their health conditions. This may ultimately result in poor health outcomes.
Some racial/ethnic minorities and older populations often have limited health literacy; however, it is seen in all populations. In the United States, low health literacy is associated with greater emergency room use and higher rates of hospitalization. Additionally, individuals with low health literacy are less likely to seek out
preventive medicine care, such as immunizations and cancer screenings.
A survey conducted at VHA facilities concluded that only 45% of Veterans receiving their healthcare at these facilities had adequate health literacy skills. African American Veterans were less likely to have high levels of health literacy than white Veterans.
At the VA Chicago Healthcare System, Veterans were asked how much they knew about colorectal cancer screening. Veterans with limited health literacy were more likely to not be aware of colorectal cancer or the importance of fecal occult testing and responded that they were less willing to undergo testing when their physician recommended it.
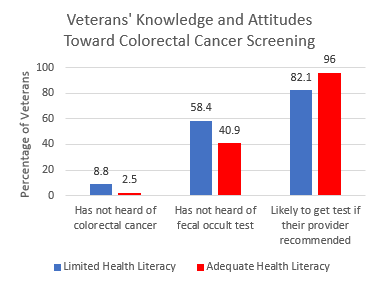
From Dolan, N. C., et al. (2004). Colorectal cancer screening knowledge, attitudes, and beliefs among veterans: does literacy make a difference?.
Journal of Clinical Oncology, 22(13), 2617-2622.
PROMOTING HEALTH LITERACY
The VA is working to ensure that Veterans have access to important health information so that they can achieve their optimal health. These efforts aim to simplify complex health information and empower Veterans to seek out health information that can help them play an active role in their health care.
NATIONAL EFFORTS
VA's Learning University developed trainings that teach VA health care providers and other employees how to apply plain language techniques in their writing. These trainings include lessons on presenting data and summarizing findings for all audiences, writing clearly and succinctly, and testing documents for readability. This helps the VA produce written materials that are understandable to all audiences.
LOCAL EFFORTS
At local VA facilities, providers have an intimate understanding of the unique needs of their patient population. At the VA Chicago Healthcare System, health care providers attended quality improvement workshops where they were trained to communicate with Veterans who have low health literacy by delivering short, personal messages to
Veterans about their health. These workshops resulted in more Veterans agreeing to be referred for cancer screenings.
Another effort sought to improve high blood pressure amongst African American Veterans by harnessing the power of storytelling. At 3 VA Medical Centers, Veterans with a history of hypertension watched videos of other African American Veterans, who also shared a high blood pressure diagnosis, tell stories of how they were successful in achieving a controlled blood pressure. Notably, Veterans with low health literacy who watched the videos had lower blood pressure readings at their 6-month follow-up appointments.
HEALTH LITERACY UNIVERSAL PRECAUTIONS APPROACH
It is difficult to recognize which patients may have low health literacy. Therefore, health care providers should utilize health literacy universal precautions with all their patients – they should assume that all the patients and caregivers they interact with may have difficulty comprehending health information. Communicating clearly helps people feel more involved in their health care and increases the chances of patients following through on their treatment plans.
The AHRQ Health Literacy Universal Precautions Tool Kit can be found at: https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/index.html
To access the Journeys with High Blood Pressure videos, go to: https://www.va.gov/HEALTHEQUITY/For_Veterans.asp.
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
For additional OHE information briefs and fact sheets visit: https://www.va.gov/HEALTHEQUITY/Publications_and_Research.asp
REFERENCES
Ferreira, M. R., et al. (2005). Health care provider-directed intervention to increase colorectal cancer screening among veterans: results of a randomized controlled trial. Journal of Clinical Oncology, 23(7), 1548-1554.
Houston, T. K., et al. (2017). African American veterans storytelling: a multisite randomized trial to improve hypertension. Medical care, 55, S50-S58.
Rodríguez, V., et al. (2013). Health literacy, numeracy, and graphical literacy among veterans in primary care and their effect on shared decision making and trust in physicians. Journal of health communication, 18(sup1), 273-289.



















