The In-Center Hemodialysis Option
Hemodialysis (HD) is one way to replace the function of kidneys that don’t work. HD is most often done in a clinic in one of two ways:
- Three days a week (standard in-center HD)
- Three nights a week while you sleep (nocturnal in-center HD)
It is sometimes called “in-center” HD.
Hemodialysis Access
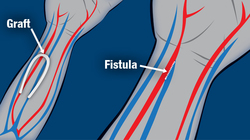
All HD requires a way to take blood out of the body to be cleaned, and then put it back in. This is called a vascular access, or just access. There are three types of access:
- A fistula, which is your artery + your vein
- A graft, which is your artery + your vein + a piece of man-made vein
- A catheter, which is a plastic tube placed into a large vein that ends in your heart
A fistula is the safest type, if you can have one.
HD Access: Fistulas
Dialysis needs the strong blood flow of an artery (the blood vessels that carry blood away from the heart). But veins (the blood vessels that carry blood to the heart) are closer to the surface of your skin and easier to reach. Linking an artery to a vein gives you the best of both: strong blood flow that is easy to reach.
Some ways of linking the artery and vein to make an access for HD are better than others. A fistula connects your artery directly to your vein. A graft connects an artery to a vein with a piece of man-made vein.
Fistulas can last the longest (sometimes decades) and they have the least chance of developing blood clots or infections that could put you in the hospital. If you want to do HD, a fistula is ideal. Plan ahead! A fistula needs to be made at least a few months before dialysis starts, so it has time to “mature” and be ready to use. It is wise to get a fistula made about 6 months before you need to start HD.
HD Access: Catheters
HD catheters are plastic tubes that are placed in a large vein in the neck, chest, or groin. They are used if someone needs dialysis right away, or has no other choice. A catheter is partly out of your body and partly inside your blood vessels. The tip is in your heart.
Catheters have several problems:
- Germs can climb up the tubing and get into your bloodstream. If this happens, a serious blood infection, called sepsis can occur.
- Catheters are linked to a risk of death that is many times higher than other types of HD access.
- Catheters can’t get wet. So, you may not be able to shower with an HD catheter.
- There may be a scar where the catheter enters your body.
HD Cleans Your Blood Outside Your Body
When you do HD, two needles are placed in your access. A nurse or technician connects the needles to tubing that carries your blood to a dialyzer, or artificial kidney. The dialyzer has filters inside to clean your blood. Wastes and extra water are removed, and then your cleaned blood comes back to you. A blood pump pushes your blood through the tubing at a rate that your doctor prescribes.
3 Days or 3 Nights a Week
HD in a center can be done in two ways:
- Standard HD is done in a clinic three days a week for about 4 hours at a time. You would get a time slot on a Monday, Wednesday, and Friday, or a Tuesday, Thursday, and Saturday. A nurse or technician sets up the treatments, or you may be able to learn to do the set-up yourself. (This is called in-center self-care.)
- Nocturnal HD can be done in a clinic three nights a week, for about 8 hours while you sleep. These treatments are most often done on Mondays, Wednesdays, and Fridays. As with standard HD, a nurse or technician most often sets up the treatments, or they can teach you to do it yourself. Since nighttime treatments are twice as long as standard ones, they are very gentle. And, nighttime treatments don’t take time out of your day.
Keeping Your Body in Balance
The job of healthy kidneys is to keep substances in your blood in balance. The closer to balance a treatment for kidney failure brings you, the better you may feel. When you feel better, you can do more of what matters to you. Nocturnal HD in a center gives you about twice as much treatment as standard HD.
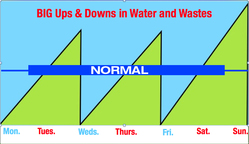
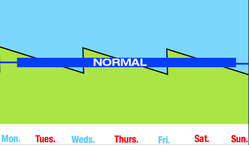
Standard HD: Big Ups & Downs
Between dialysis treatments, wastes and excess water build up in your blood. If you have a 4-hour treatment on Mondays, Wednesdays, and Fridays, you have no treatment on Tuesdays, Thursdays, Saturdays, or Sundays. The ups and downs when wastes and water build up are big with standard in-center HD—and they are hard on the heart.
Nocturnal HD: Very Small Ups & Downs
Nocturnal HD in a center removes much more water and wastes from your blood than standard HD. And, since the treatments are twice as long, it is much more gentle, as you can see from the very small spikes in water and wastes (green) in the picture on the right.
This means that even with three treatments per week, you may feel good from day to day, with fewer symptoms from kidney failure. In fact, most people feel like themselves again about 10 minutes after doing a nocturnal HD treatment.
In-center HD and Your Lifestyle
Now that we’ve seen the basics of how in-center HD works, let’s look at how it might affect your life in the areas of:
- What you can eat and drink
- How many medications you might need to take each day
- How much control you would have over your time
- How work-friendly it is
- How travel-friendly it is
- How it may affect your sex life and ability to carry or father children
Standard HD and What You Eat
Since standard HD is done 3 times a week for only 4 hours, it requires more strict diet and fluid limits than any other option. Your dietitian will go over your lab test results with you each month and help you come up with a plan that includes as many of your favorite foods as possible. To learn more about lab tests, visit the Laboratory.
Nocturnal HD in a clinic is done 3 times a week for about 8 hours. More treatment means you have fewer diet and fluid limits. You can eat more of what you like best with this treatment option.
Standard HD Means Limits on Some Foods & Fluids
Most people who do HD must limit their intake of:
- Salty foods, like french fries
- High potassium foods, like fruits
- High phosphorus foods like beans, nuts, and dairy
- Fluids—to about 1 quart per day
If you have diabetes, you still need to limit starchy foods.
If you choose standard in-center treatment, you MUST follow the strict limits to feel your best. If an unrestricted diet is important to you, talk with your care team about other dialysis options that have fewer limits.
Standard HD and Medications
If you choose standard HD, you may need to take as many as 19 pills each day. Most people on standard in-center need phosphate binders and blood pressure pills. You may also need EPO to help treat anemia. If you have diabetes or other health problems, you will still need to take prescribed drugs for them, though the dose may change when your kidneys don’t work.
If you do nocturnal HD in a clinic, you may need fewer—or no—phosphate binders or blood pressure pills. You may need EPO to help treat anemia, but may be able to use a lower dose. If you have diabetes or other health problems, you will still need to take prescribed drugs for them, though the dose may change when your kidneys don’t work.
Standard HD and Your Schedule
If you do standard in-center HD, the clinic will work with you to assign a time slot. Your treatments will be done at the same time on Mondays, Wednesdays, and Fridays or Tuesdays, Thursdays, and Saturdays. If the time slot you are given is not a good fit for your life, your job, your childcare, or your ride to the clinic, talk to your care team.
Standard HD and Your Job
Do you want to be able to work? A work-friendly treatment:
- Is not done during the work day—or can be done at work
- Does not cause symptoms that might make you miss work
- Reduces the chance that you might need to go to the hospital—and miss work
- Helps you to have enough energy to work
Standard in-center HD is not very work-friendly for all of these reasons. It takes time out of the day, when most people need to be at work. It can cause symptoms that make it hard to work, and can lead to more hospital stays than other treatment options. People DO work on standard in-center HD—but it is more of a challenge than it would be with other treatment options.
Standard HD and Travel
When you do HD in a center—during the day or at night—you can travel by finding a clinic at your destination that has a time slot open and can take you. This is best done a few months before you want to travel. Your social worker can help you plan and send the clinic your medical records. You will need to be up-to-date with your vaccines, too.
Standard HD, Fertility, and Your Sex Life
People who do standard in-center HD report more problems with sexuality and fertility than those who do any other treatment option. For men, about half who do this treatment report problems with erections. It is also more difficult to father a child.
Women have problems, too. It is harder to carry a child using this treatment option. Women who become pregnant on standard in-center HD may have a chance of carrying a baby to term if they do longer and/or more frequent treatments.
There are few studies on the sexuality of people who do nocturnal HD treatments. People who do dialysis this way say they feel better, and there are some reports of women being able to carry babies to term.
Standard HD: Facts to Consider
There are things to think about when you do HD in a clinic—during the day or at night. Your risk of infection is very high if you start treatment with a catheter. If you know you want to do HD, get a fistula or graft well ahead of time.
You need to be at the clinic for each treatment at the time that is set for you. If this time is not a good fit for your life, talk to your care team. You may be able to switch to a time that fits better, or to a clinic that has a better time for you. You may have to wait until the time slot you want opens up. Don’t miss any dialysis! Missed treatment time can cost you your life when you are on dialysis.
Some people have a hard time sleeping in a clinic at night. Wearing earplugs and a sleep mask may help. Some even bring in a foam pad for the chair to make it easier to sleep.
Dealing with HD Needles
Fistulas and grafts for HD use needles. If needles bother you, there are lots of things you can do to help:
- You can put a numbing cream on your skin 1–2 hours before treatment. Some numbing creams are prescription and some are not. Talk to your care team.
- A freezing spray can numb just the top of your skin very quickly.
- You can try to relax and take deep breaths.
- Putting in your own needles puts you in charge and distracts you, so the needles hurt much less. No one else can put in your needles as well as you can—you are the only person who can feel both ends of the needle. The clinic staff can teach you how if you want to learn.
- The “Buttonhole technique” is a way of putting dialysis needles into the exact same spots every time to form tunnel tracts (like pierced earring holes). Once Buttonholes form, you can use blunt needles for dialysis, for less pain.
You've reached the end of this topic:
Hemodialysis in a Clinic
- Which of these is the safest type of blood access for hemodialysis (HD)?
Not scored A fistula is made only of your own artery and vein. This makes it much less prone to problems with blood clots or germs than any other access choice.
- When you do HD, tubing takes your blood to and from:
Not scored The artificial kidney (or dialyzer) is a clear plastic tube filled with hair-thin hollow fibers that clean your blood.
- HD can be done in a clinic:
Not scored Some clinics offer HD treatments at night as well as during the day. Nighttime (nocturnal) treatments are twice as long, so they are much more gentle.
- What type of diet and fluid limits does standard in-center HD require?
Not scored Treatments are only done three times a week for a few hours—while healthy kidneys worked 24/7. So, standard in-center HD requires the most diet and fluid limits of any treatment option.
- Nocturnal in-center HD is work-friendly, because:
Not scored When you do your treatments at night while you sleep, you have your days free to do other things, like work or take care of loved ones.