Multiple Sclerosis Centers of Excellence
The Urinary Tract in Multiple Sclerosis
Nina Davis, MD, FACS
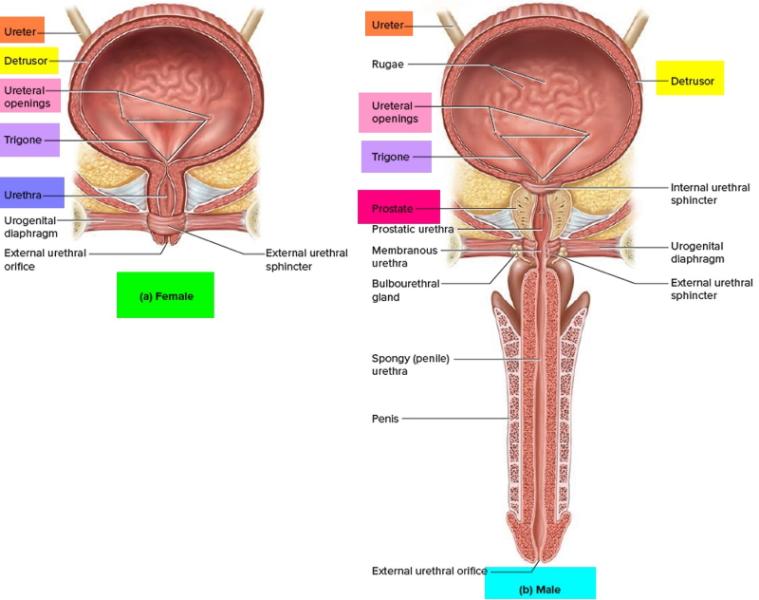
For normal urination to occur, the bladder and the urethra (the tube that conducts urine from the bladder to the outside) must work together in a coordinated fashion. When the bladder is full and there is an urge to urinate, the bladder neck (internal urethral sphincter or valve) and the external urethral sphincter (muscle valve in the urethra) open, then the bladder muscle contracts (squeezes) to push the urine out. When the bladder is finished emptying, it relaxes, then the external urethral sphincter and bladder neck close. Please see illustration below for normal anatomy.
 However, between 50-90% of people with MS experience nerve-mediated dysfunction of the bladder or external urethral sphincter or both, causing them to have bothersome urinary tract symptoms. These symptoms include:
However, between 50-90% of people with MS experience nerve-mediated dysfunction of the bladder or external urethral sphincter or both, causing them to have bothersome urinary tract symptoms. These symptoms include:
OVERACTIVE BLADDER or "spastic" bladder. With an overactive bladder, abnormal nerve signals cause the bladder to contract or spasm before it is full which can cause involuntary urine leakage called urgency incontinence. Overactive bladder is the most common urinary disorder associated with MS. It occurs in about 66% of people with MS.
DETRUSOR SPHINCTER DYSSYNERGIA (DESD). This is when the external urethral sphincter is not in sync with the bladder. Just like the bladder, the external urethral sphincter can be spastic so that it doesn't open correctly to allow the bladder to empty. This can cause hesitancy – problems getting the urine stream going, or weak stream - making emptying slow and more difficult. The sphincter can also close early, not allowing the bladder to finish emptying. When DESD is present, the bladder's inability to empty can lead to urinary infections. DESD occurs in about 47% of people with MS. Most often, there is a combination of bladder spasticity and external urethral sphincter spasticity and each of these disorders must be treated separately to restore good urinary function.
The least common form of bladder impairment in MS is a HYPOTONIC BLADDER (weak bladder) which occurs in about 20% of people with MS. This is the most difficult to treat because the bladder is not strong enough to squeeze the urine out, and there are no treatments to make the bladder muscle stronger. Patients with hypotonic bladders need some form of catheterization to empty their bladders.
When the bladder is unable to empty adequately because it is weak or because the external urinary sphincter doesn't open correctly to allow the bladder to empty, retention of urine occurs. This means the bladder always has urine left after urination. It is never empty. People with retention are at greater risk of infection because the bladder is not being flushed out.
Fortunately, with greater understanding of the effects of MS on the urinary tract and advances in medical care, there are now a number of treatments for these disorders ranging from minimally invasive treatments like pelvic floor physical therapy, medications alone or in combination, various devices for collection of urine or for nerve stimulation and, use of Botox in the bladder wall.



















