Overview
The thyroid is a vitally important hormonal gland that plays an essential role in metabolism, growth, and maturation of the human body. The thyroid produces and releases into the circulation at least two potent hormones, thyroxine (T4) and triiodothyronine (T3), which influence basal metabolic processes and enhance oxygen consumption in nearly all body tissues. Thyroid hormones also influence growth, temperature regulation, lipid and carbohydrate metabolism, cardiac myocyte activity, reproduction, cognitive functioning, and bone development.
Hypothyroidism is the insufficient production of thyroid hormone. Overt hypothyroidism is present in 0.1-2% of all adults, with 15% of older women meeting the criteria for subclinical hypothyroidism.[1] Worldwide, iodine deficiency is the most common cause of hypothyroidism. In the United States, where salt is fortified with iodine, autoimmune thyroiditis or Hashimoto’s thyroiditis is the most common type of hypothyroidism. In autoimmune thyroiditis there is cell-mediated antibody destruction of the thyroid gland. The second leading cause of hypothyroidism is iatrogenicincluding situations when surgery, medications, or radiation have affected the functioning of the gland.[2]
Because the thyroid affects so many different physiologic processes in the body, the clinical signs of hypothyroidism are variable from one individual to another. Some patients present with mild symptoms in spite of having low levels of circulating thyroid hormones, while some patients have more significant symptoms despite only mildly abnormal lab testing.
Common Symptoms of Hypothyroidism
- Fatigue
- Dry skin and nails
- Cold intolerance
- Hair loss
- Concentration or memory problems
- Constipation
- Weight gain
- Bradycardia and hypothermia
- Carpal tunnel symptoms
- Menorrhagia, irregular menses, or infertility
- Depression[2]
Diagnosis
The diagnosis of hypothyroidism is based on the combination of clinical context and laboratory tests including TSH and Free T4. In primary hypothyroidism, serum TSH is elevated (typically >4.5mI/L) and serum free T4 is decreased.
There is a continuum between the euthyroid state and hypothyroidism and it is suggested that the range be further contracted to an upper limit of normal of 2.5 mIU/L to more appropriately diagnose people with hypothyroidism. Approximately 80% of adults have a TSH below 2.5mml/L suggesting that the normal cut-off should be lower to better capture all cases of hypothyroidism. However, natural history data shows us that up to half of older people (ages 50-70) with upper limit TSH 3.0-5.0 and thyroid antibodies will go on to develop hypothyroidism. As few as 10% of people of younger age (ages 20-40) without antibodies will go on to develop hypothyroidism. Many endocrinologists argue that the TSH limit should not be adjusted as the normalization of TSH is common and there are no health consequences for those with a mildly elevated TSH but normal thyroxine levels.[3][4]
Treatment of subclinical hypothyroidism (TSH 5.0-10.0 mIU/L) is also not recommended by conventional medicine as there is no compelling evidence that treatment with levothyroxine improves symptoms compared with placebo in individuals with TSH in the 5.010 mIU/L range. Treatment of subclinical hypothyroidism when serum TSH is between 5 and 10 mIU/liter generally does not have a beneficial effect on serum lipid profiles and does not affect cardiac risk. In addition, use of thyroid hormone therapy in nonpregnant adults with subclinical hypothyroidism was not associated with improved quality of life or thyroid-related symptoms.[5] The only documented adverse health outcome for individuals with TSH levels between 3.0 and 5.0 mIU/L is progression to overt hypothyroidism.[6] In general, treatment can be considered in the following situations:
- Patients who have TSH levels higher than 10 mIU/L on repeated measurements
- Patients who have symptoms or signs (e.g., goiter) associated with thyroid failure
- Patients who have convincing family history of thyroid disease
- Pregnant patients
- Patients who have severe hyperlipidemia[2]
Some practitioners feel conventional methods of diagnosis of hypothyroidism are too narrow and miss many cases of hypothyroidism in patients who are clinically symptomatic. An alternative practice is to look at the absolute levels of T3 and T4, not just TSH. If T3 and T4 are low, regardless of TSH, a patient may be diagnosed by these practitioners with hypothyroidism.
Nutrition
Goitrogens
Goitrogens are food substances that block thyroid hormone synthesis. Thiocyanate and isothiocyanate are compounds found in cruciferous/brassica vegetables (cabbage, broccoli, cauliflower, and Brussels sprouts) and they have been found to block the iodination of thyroglobulin if they are consumed in high amounts. This is especially true if a person is iodine deficient.[7] Studies also show suppression of thyroid peroxidase activity, TSH elevation, and increase in thyroid symptoms in people eating high quantities of soy isoflavones.[8] When eating a reasonable amount of soy and Brassica vegetables (less than 30 gm daily), steaming or cooking these foods briefly may help reduce their goitrogenic effect while preserving their nutrient content.[9]
Gluten and Thyroid
The link between celiac and other autoimmune diseases, including autoimmune thyroiditis is well-established. Treatment of celiac disease with the avoidance of gluten can improve absorption of levothyroxine and enhance subsequent treatment effects.[10] While current evidence does not suggest that a gluten-free diet mediates thyroid symptoms in patients with celiac disease or gluten intolerance, many patients do find this to be helpful.
The Anti-Inflammatory Diet
A number of medical conditions are linked to too much inflammation, including autoimmune thyroiditis. Any long-term, healthy eating plan should try and incorporate the principles of the anti-inflammatory diet. The pertinent aspects of this diet include: avoiding trans-fats, limiting fats that are high in omega-6 fatty acids including many saturated fats, increasing monounsaturated fats and omega-3 in the diet, aiming for 8-10 servings of fruits and vegetables, and eating at least 30 gm of fiber daily, choosing whole grains whenever possible.
Vitamins & Minerals
Iodine
Iodine is an essential element for humans and is required for the synthesis of thyroid hormones (refer to Table 1). Iodine deficiency is common in many land-locked developing areas of the world, but not in the United States and other industrialized countries, where table salt is fortified with iodine. Ironically, ingestion of too much iodine can lead to iodine-induced hyperthyroidism (the Jod-Basedow phenomenon) or iodine induced hypothyroidism (the Wolff-Chaikoff effect) in patients who are iodine deficient. In patients without iodine deficiency, chronic exposure to high levels of iodine reduces binding over time and can also cause hypothyroidism.[11]
Sea vegetables and seaweed including kelp, nori, and dulse are natural sources of iodine. The quantity of iodine in each serving will vary based on where they were grown, species, part of plant, climate they grew in and how they were prepared.
Iodine testing is typically not necessary, though it can be considered in patients with dietary restrictions, medication use or heavy metal toxicity. The unprovoked 24-hour urine iodine test is currently the best method to evaluate iodine levels. A provoked 24-hour urine iodine test with a 50 mcg iodine load can be done, but is rarely necessary.[12]
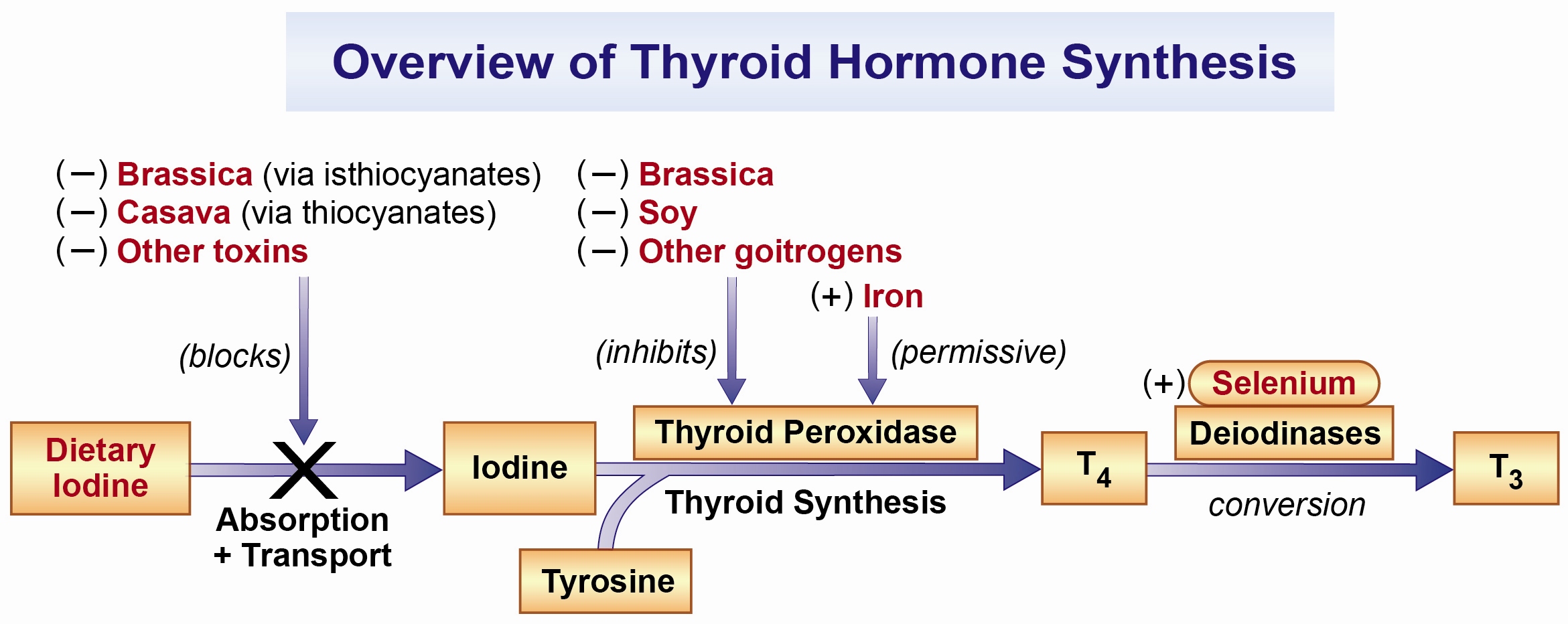
Selenium
Adequate selenium is also required for proper thyroid function.[13] (Refer to Figure 1, above.) Specifically, selenium facilitates conversion of T4 to the active T3 through selenium dependent deiodinases.[14] A 2019 review found that patients with hypothyroidism exhibited lower selenium levels than healthy controls.[15] Selenium supplementation may improve thyroid dysfunction in patients who are deficient. It is unclear to what extent selenium benefits patients with hypothyroidism in the absence of a selenium deficiency.
Other nutrients: vitamin A, iron, and zinc
Many other vitamins and nutrients influence thyroid function, most notably vitamin A, iron, and zinc (refer to Figure 1). A 2019 review found that patients with hypothyroidism had lower levels of zinc compared with healthy controls.[15] Consider supplementing with them in hypothyroidism, especially if deficiency states are suspected.[12]
L-Tyrosine
L-Tyrosine is an amino acid and is important for thyroid function. Thyroxine (T4) is produced through the iodination of tyrosine (Figure 1). Tyrosine is absorbed through diet and also created by the conversion of phenylalanine. Tyrosine supplementation may be helpful in patients for hypothyroid symptoms in patients who are deficient.[16] The recommended dose of L-Tyrosine is 500 mg three times daily.
Recommended daily doses based on the Recommended Daily Allowances (RDAs) and Tolerable Upper Intake (TUI) levels for adults are listed in Table 1.
Table 1. Recommended Daily Allowances (RDA) and Tolerable Upper Intakes (TUI) for Thyroid-Related Nutrients
| Vitamin/Mineral | RDA | TUI |
|---|---|---|
| Iodine | 150mcg/day | 1100mcg/day |
| Selenium | 55mcg/day | 400mcg/day |
| Vitamin A | 800mg/day | 3000mg/day |
| Iron | 12mg/day elemental | 45mg/day elemental |
| Zinc | 10mg/day | 40mg/day |



















