Nausea and vomiting are the most distressing side effects of chemotherapy and are experienced by up to three-fourths of patients receiving chemotherapy. They can interfere with the ability to perform normal household tasks, enjoy meals, and maintain daily function and activities, thereby reducing their quality of life. The severity of these symptoms can also reduce adherence to chemotherapy regimens and lead to malnutrition. In addition to the numerous antiemetics that are available, several integrative therapies also significantly reduce chemotherapy-induced nausea and vomiting (CINV).
Acupuncture
Several acupressure points, when stimulated by needles, electricity, or pressure, reduce CINV.[1][2][3] Acupressure reduces the severity of acute and delayed nausea, however, it has no benefit on the incidence and severity of vomiting.[4] For the prevention of nausea, needles should be placed at least 30 minutes before the chemotherapy session and continued for as long as required. Acupuncture can also be done the day before and day after chemotherapy, and should be administered by acupuncturists specially trained in oncology who will have knowledge of contraindications. Some specific acupuncture points are described below. For general information, refer to Passport to Whole Health Chapter 18, Whole Systems: Chinese Medicine and Acupuncture.
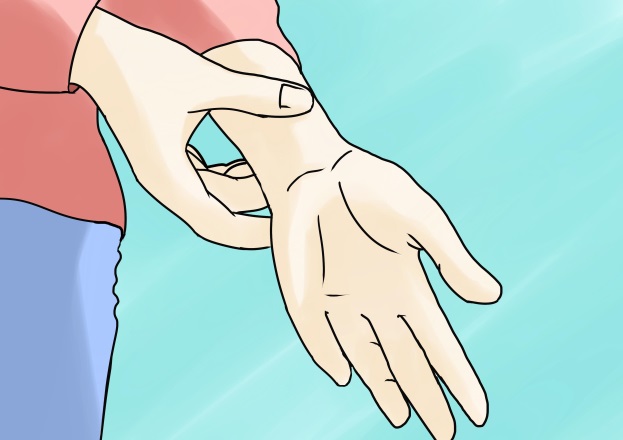
The PC6 (P6) acupressure point alleviates nausea and is easy to find:[5]
- Take your index finger and middle finger and place them on your wrist at the base of your palm to measure where your nausea acupressure point is.

- Two or three finger widths down from the top crease in the wrist, centered in the groove between the two large tendons is the PC6 point.

- Take your thumb and index or middle finger and press firmly on the points on both sides of the wrist when you feel nauseous. You should feel relief in 10-30 seconds, but it can take up to 5 minutes.
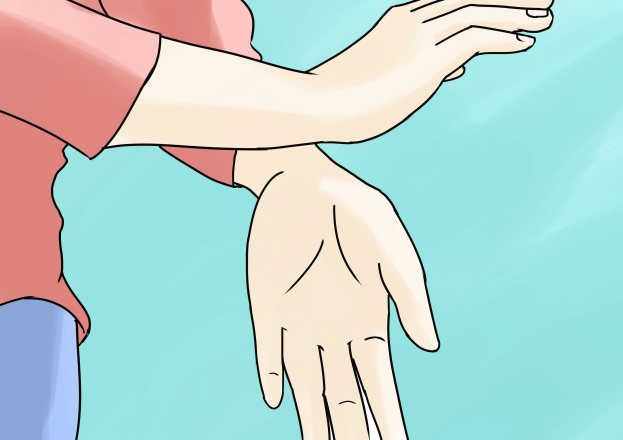
- You can also tap your wrists together gently at the acupressure points while taking deep breaths. Alternate with tapping the outsides of your hands together.
- Purchase a wristband that applies pressure to the correct spot. They usually have a knob or flat button positioned over the acupressure point. You might feel relief as soon as you put it on, but after your body grows accustomed to the pressure, youll need to press down on the acupressure point for extra relief.

- Another acupressure point that is commonly used for gastrointestinal discomfort, nausea and vomiting, and stress and fatigue is ST36. Measure four finger-widths down from the bottom of your kneecap, along the outer boundary of the shinbone.
If you are in the right place, a muscle should pop out as you move your foot up and down. To use this acupressure point, (1) locate the point then (2) apply downward pressure on the muscle, stimulating the area for 4-5 seconds.[6][7]
Acupressure Point stomach-36. Reprinted with permission from John Kirkwood. https://www.acupressure.com.au/wprss/?p=44
Aromatherapy
Inhalation and massage aromatherapy are beneficial for chemotherapy-induced nausea and retching.[8] Peppermint essential oil can be very helpful for nausea.[9] Patients may carry a bottle and sniff it throughout the day when needed. One to two drops of peppermint oil can be added to a 12-oz bottle of water and consumed throughout the day.
Botanicals
Note: Please refer to the Passport to Whole Health, Chapter 15 on Dietary Supplements for more information about how to determine whether or not a specific supplement is appropriate for a given individual. Supplements are not regulated with the same degree of oversight as medications, and it is important that clinicians keep this in mind. Products vary greatly in terms of accuracy of labeling, presence of adulterants, and the legitimacy of claims made by the manufacturer.
Ginger
Ginger (Zingiber officinale) is a well-known antiemetic and several studies have found it effective for CINV.[10] It appears to be more effective for acute nausea and vomiting rather than delayed.[11][12] The dose is powdered ginger root 1000 mg daily starting on the first day of chemotherapy and continued for 5 days. Another dosing is 500 mg every 4 hours starting on the first day of chemotherapy and continuing as long as needed. It may be consumed in capsule form, candied ginger, ginger ale (made from real ginger), and tea. Freshly diced ginger tea can be consumed on the day of chemotherapy and continued for as long as needed. Ginger is an anticoagulant, so use with caution in patients who are on blood thinners and avoid high doses in patients with a low platelet count.
Astragalus
Astragalus (Astragalus membranaceus) is a traditional Chinese medicinal herb that has also been found effective in reducing CINV.[13][14] Since astragalus is often given in combination with other herbs, a dose as not been established.
Mind-Body
Most patients who experience CINV attribute these side effects to a psychological etiology, justifying the need for mind-body therapies in managing symptoms. Effective therapies include clinical hypnosis,[15] Guided Imagery, progressive muscle relaxation[16], systematic desensitization, yoga,[17] and healing touch.[18] A health psychologist or a practitioner trained in these modalities can teach several of these techniques to patients. Patients may perform progressive muscle relaxation in conjunction to listening to Guided Imagery CDs before and during chemotherapy. (For more information, go to Progressive Muscle Relaxation Whole Health tool.) Guided Imagery CDs and MP3s for chemotherapy can be purchased at the Healthy Journeys website. Music therapy can have positive effects when used in conjunction with other mind-body techniques, but the data is inconsistent.[19][20] During chemotherapy treatment, encourage patients to use simple distractions, such as listening to a relaxation tape or soft music, drawing, knitting, reading, or doing crossword puzzles.
Manual Therapy
A study found that 20-minute hand or foot massage sessions given to breast cancer patients during chemotherapy significantly reduced nausea.[21]
General Dietary Recommendations
- Eat several small meals frequently throughout the day.
- Drink plenty of water, at least 8 cups per day, to stay well hydrated. Natural electrolyte-restoring drinks are also beneficial, but avoid ones high in sugar and artificial ingredients. Try sucking on ice chips with a little salt or fruit juice. Avoid drinking a lot of liquids during mealtime, as they increase the sensations of fullness and bloating.
- Decrease spicy, fatty, fried, and acidic foods in the diet. Avoid foods with strong odors and high sugar content.
- Room temperature and cold foods are easier to tolerate.
- Eat slowly and try to relax. Avoid stressful situations and environments before and after eating. Use distractions while eating such as listening to music, watching TV, or engaging in conversation. Avoid lying down for 1 to 2 hours after eating. If foods have a metallic taste, try eating with plastic utensils.
- Rinse your mouth to eliminate bad tastes, and suck on hard candies such as peppermints and lemon drops.
- Avoid strong scents, smelly cooking areas, smoke, perfume, and warm stuffy rooms, especially while eating. Get plenty of fresh air while eating and wear loose-fitting clothing. Use unscented deodorants and soaps.
- Eat soft, bland, easy-to-digest foods such as plain crackers, toast, dry cereals, plain yogurt, broth and clear soups, sorbets, rice cakes, pretzels, pita bread, plain rice, potatoes, oatmeal, applesauce, egg whites, and cooked vegetables. Choose nutritious, high-protein snacks such as nuts, and peanut butter on crackers. Use meal replacements or shakes when not tolerating food. Try eating some bland snacks in the morning before getting out of bed if the nausea occurs when you wake up.
- For oral rehydration, start with sips of clear liquids 1 tbsp at a time. And increase to 1/4 cup at a time. Once food is tolerated, advance to the bland, starchy foods mentioned above.
- Gentle exercise may be helpful in decreasing nausea and increasing appetite. Try to walk for 15 minutes when nausea hits.[22]
Summary of Treatments
Supplements & Botanicals
- Ginger
- Astragalus
- Peppermint Oil
Other Complementary Therapies
- Acupuncture and acupressure
- Massage
- Healing touch
- Music therapy
Mind-Body
- Clinical hypnosis
- Guided Imagery
- Progressive muscle relaxation
- Systematic desensitization
- Yoga
Author(s)
Managing Chemotherapy-Induced Nausea and Vomiting was written by Srivani Sridhar, MD (2014, updated 2020).



















