Estrogen dominance is the condition of increased estrogen levels relative to progesterone levels in the body. Estrogen dominance may be the result of overproduction of estrogen by the body, changes in estrogen metabolism and excretion, or an imbalance in the estrogen to progesterone ratio. Many conditions are thought to be associated with or exacerbated by estrogen dominance, including breast and uterine cancers, fibroids, endometriosis, and polycystic ovarian syndrome.
The body makes three main estrogens:
- Estrone (E1)
- Estradiol (E2)
- Estriol (E3)
Estrone (E1) is the main type of estrogen present in the body after menopause, made primarily in adipose tissue. Estradiol (E2) is the strongest estrogen, made by the ovaries and present in the body before menopause. Estriol (E3) is the weakest estrogen, present in the body primarily during pregnancy.
The body has two main receptors to which estrogen binds: alpha receptors that promote cell growth and beta receptors that inhibit cell growth. Each type of estrogen binds with varying affinity to these receptors, resulting in either cell proliferation or cell inhibition. Besides the direct effects of estrogen in the body, its metabolites are also important.
Estrogen is broken down along two major pathways, into 2-hydroxyestrone and into16-hydroxyestrone. Each of these metabolites has distinct functions in the body. 2-hydroxyestrone has multiple health benefits, working to block stronger estrogens that promote cell proliferation and possible cancer growth. Conversely, 16-hydroxyestrone increases cell proliferation. Higher levels of 16-hydroxyestrone are associated with inflammation, excess levels of omega-6 fatty acids, obesity, hypothyroidism, and pesticide toxicity.[1] A small amount of estrogen is metabolized to 4-hydroxyestrone, which is thought to promote cancer by damaging DNA. (Figure 1 outlines how estrogens fit into the steroid metabolism pathway.)
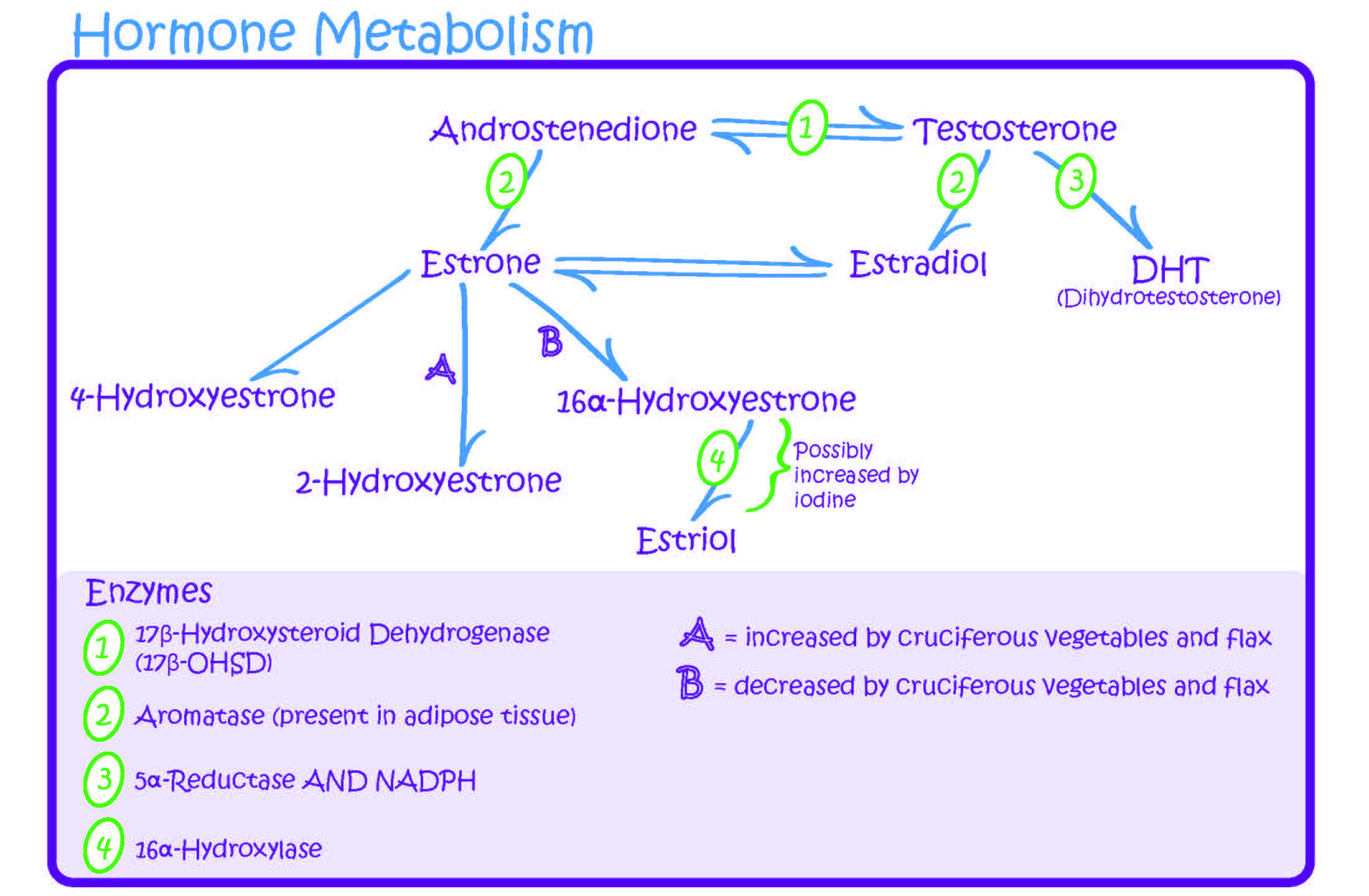
Figure 1. Estrogen and the Steroid Metabolism Pathway.
For these reasons, a healthy estrogen balance favoring production of 2-hydroxyestrone is important for womens health. Although lab testing can determine a womens estrogen ratio, testing is likely unnecessary for most women. Women with an increased risk of estrogen-sensitive conditions and who have behaviors that promote estrogen dominance should be counseled in healthy lifestyle changes. The following have been shown to shift estrogen metabolism toward the 2-hydroxyestrone pathway[2]:
- Exercise and weight loss
- Isoflavones such as soy and flaxseed
- Omega-3 fatty acids
- Green tea polyphenol
- Cruciferous vegetables and broccoli derivatives, including indole-3-carbinol (I3C) and diindolylmethane (DIM, result of I3C after activation by stomach acid)
A healthy lifestyle that allows for a normal weight helps to decrease the risk of insulin resistance from metabolic syndrome. Insulin resistance results in increased estrogen levelsboth by increasing aromatase activity, resulting in the conversion of testosterone into estrogen, and by decreasing sex-hormone-binding globulin, resulting in greater amounts of free circulating estrogen.[2] Insulin resistance also causes increased production of inflammatory mediators, which likely contributes to estrogen-sensitive conditions including fibroids. For these reasons, regular exercise and anti-inflammatory supplements are often used in treatment of estrogen-dominant conditions.
Lifestyle habits also influence estrogen excretion. Women eating a vegetarian diet have a three-fold increase in fecal estrogen excretion and have lower serum estrogen levels by 15%-20%.[3] Intestinal dysbiosis, or an imbalance of the gut microflora, may also contribute to estrogen dominance. Overgrowth of certain gut bacteria increases levels of the enzyme beta-glucuronidase, which cleaves estrogen from glucuronic acid, preventing its excretion and allowing for reabsorption.[2] Diet and gut microflora influence estrogen absorption and its enterohepatic recirculation. Therefore, clinicians should address intestinal health when considering conditions of estrogen dominance. For more information, refer to Promoting a Healthy Microbiome with Food and Probiotics.
Stress can also influence the balance of hormone levels in the body. Cortisol, the bodys stress hormone, is made from precursors that include progesterone. With an increasing need for cortisol production because of high stress, progesterone levels may decrease, disrupting the balance of estrogen and progesterone in the body. For this reason, stress management should be addressed.
In summary, the following healthy lifestyles should be encouraged to support a positive estrogen balance in women at risk or with diagnoses of estrogen-sensitive conditions.
1. Engage in moderate exercise daily to maintain a healthy weight.
2. Eat an anti-inflammatory (or vegetarian) diet to avoid hormone exposure. Consume foods high in omega-3 fatty acids from both fish and flaxseed. Consider anti-inflammatory botanicals such as ginger (Zingiber officinale) and turmeric (Curcuma longa), in addition to omega-3 supplementation of 1,000-2,000 mg of EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) daily if inadequate dietary intake.
3. Eat a high-fiber diet, as fiber decreases the amount of estrogen absorbed and increases the amount of estrogen excreted.[4]
4. Eat a diet high in cruciferous vegetables, including cabbage, broccoli, cauliflower, and Brussels sprouts. Consider supplementing indole-3-carbinol 300 mg daily if inadequate dietary intake.
5. Eat a diet high in whole soy foods which help to shift estrogen metabolism toward increased levels of 2-hydroyestrone. For more information, refer to the Phytoestrogens Whole Health tool, as well as the food and drink section of the Cancer Care Whole Health overview.
Note: Please refer to the Passport to Whole Health, Chapter 15, Complementary Integrative Health: Dietary Supplements for more information about how to determine whether or not a specific supplement is appropriate for a given individual. Supplements are not regulated with the same degree of oversight as medications, and it is important that clinicians keep this in mind. Products vary greatly in terms of accuracy of labeling, presence of adulterants, and the legitimacy of claims made by the manufacturer.
6. Avoid excessive alcohol intake, which inhibits estrogen detoxification and increases estradiol levels.
7. Avoid xenoestrogens, or environmental compounds that imitate estrogen in the body. Examples include PCBs (polychlorinated biphenyls), BPA (bisphenol A), and phthalates.
8. Promote a healthy intestinal microbiome, addressing possible food intolerances and supplementing with probiotics if necessary. Refer to the Whole Health tool Promoting a Healthy Microbiome with Food and Probiotics.
9. Engage in a healthy approach to stress management. Consider coping techniques, relaxation exercises, and mind-body practices.
Author(s)
Estrogen Dominance was written by Anne Kolan, MD (2014, updated 2020).



















