Passport to Whole Health: Chapter 11
Chapter 11. Spirit & Soul: Growing & Connecting
The twenty-first century will be all spiritual or it will not be at all.
―André Malraux
The Importance of Spirituality, Meaning, and Purpose
Spirituality, for many people, is at the heart of “what really matters.” It provides the context for health and well-being. It connects us to our deepest values and beliefs. It can be at the core of our resilience, and it can help us make sense of why we suffer, the nature of death and dying, and ultimately, the meaning of life. Drawing on Spirit and Soul can be foundational when it comes to providing individualized, whole-person care.[614] It can also be what we turn to during challenging times.
Roger Walsh, MD, author of Essential Spirituality, defines spirituality as the “…direct experience of the sacred.”[615] Fred Craigie, PhD, who teaches widely about spirituality in medicine, defines spirituality simply as, “what life is about.” “Religion,” in contrast, has been described as “…a body of beliefs and practices defined by a community or society to which its adherents mutually subscribe.”[616] “Religiosity,” a term mainly used in research, is used to describe a person’s being religious. “Soul,” in the most general sense, is what makes something or someone alive.
Each of us experiences the sacred in different ways, and this is even true for those who belong to the same religion. Keeping the definitions of spirituality and religion general allows personal health planning to remain inclusive. That is essential if Whole Health care of “Spirit and Soul” truly is to be personalized to the needs of any given patient.
As you consider how to explore this very broad topic with Veterans, it is important to keep your scope of practice in mind. Many Whole Health team members are uncomfortable with talking about others’ religious or spiritual beliefs. Chaplains are there to help. Whole Health Chaplains are trained and designated to provide Veteran spiritual care. If someone needs a formal spiritual assessment, that should, of course, be done by a chaplain. If concerns about Spirit and Soul arise, it is always a good idea to bring in experts to be part of the Whole Health team. If you are a chaplain, keep educating other members of the team about your role and what you can offer Veterans. A more detailed description of chaplaincy is offered later in this chapter.
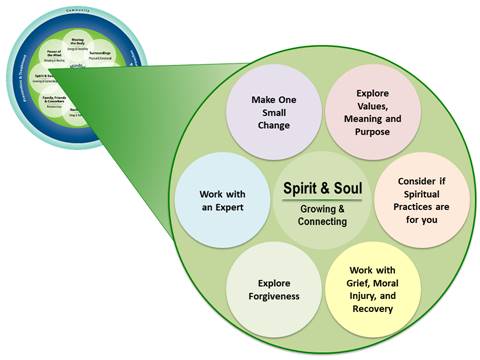
Figure 11-1 highlights some “subtopics” that can be considered when incorporating Spirit and Soul into a Veteran’s Personal Health Plan (PHP). The subtopics were developed for skill-building courses for Veterans and are related to each of the eight self-care topics in the Circle of Health. Note that there is a “Make One Small Change” circle that leaves room for creativity in case Veterans do not see an option that interests them. This chapter explores several of these subtopics in more detail.
Spirituality in Unprecedented Times
Increased isolation resulting from the global pandemic’s required social distancing, canceled spiritual gatherings, and building closures make it challenging to connect spiritually based on traditional practices. 67 Though the public health precautions are necessary, they have caused an unprecedented prevalence of anxiety and uncertainty that has taken a toll on spiritual, physical, emotional, and mental well-being. 66 The pervasive anxiety and uncertainty experienced in light of the pandemic is intensified by disturbing patterns of violence and micro-aggressions due to systemic racism. During these challenging times, relying on spirituality is an essential coping mechanism for living with life-changing and traumatic events. 68 Spirituality, religion, or a connection to a higher power outside of ourselves is a way to practice self-care and elicit positive emotions. Engaging in non-traditional practices of spiritual connection such as nature walks, virtual gatherings, and in-person share circles can be beneficial for overall spiritual and emotional well-being.
Inquiring About Spirituality
If a Veteran is discussing Spirit and Soul for the purposes of creating a PHP, it may be appropriate to do one or more of the following[617]:
- Learn about their spiritual and religious beliefs and how these beliefs influence their Mission, Aspiration, Purpose (MAP).
- Ask if they are experiencing any spiritual distress (described below) and help them to draw upon their strengths and find the support they need. These needs may vary based on lived experiences. Discuss spiritual and religious belief and/or practices.[618] Explore deeply held values or intentions that could affect their treatment preferences. Common examples would be fasting in the hospital for religious reasons or not wishing to receive blood transfusions. Engage in clear communication to understand the Veterans’ thoughts on code status and how involved they want loved ones to be in their care. Refrain from making assumptions on what is most important to the Veteran; if you have questions about the Veteran’s priorities, ask them directly.
- Consider if it is appropriate based on the Veteran’s belief system to use practices such as yoga and meditation, which have their origins in Eastern religious and spiritual traditions.
- Ask Veteran if they are struggling with grief, moral injury, or the need to forgive, and consider what resources are available to support them.
- If spiritual or religious concerns arise, know how to connect the Veteran with chaplains and other spiritual care providers as appropriate.
- Consider the Veteran’s identifiable information. Veterans’ needs may vary based on their lived experiences, gender identity, sexuality, social economic status (SES), race ethnicity, generational trauma, or other factors. Chaplains are in a unique position to offer support for these needs because of their training and focus on spiritual well-being.
To guide clinicians with lines of inquiry regarding spirituality, dozens of assessment tools have been created. Note that these are only used to get general information; again, if a spiritual assessment is needed, connect the Veteran with a chaplain or official in their religious community. Commonly used tools include FICA,[619] HOPE,[620] FAITH,[621] and SPIRIT,[622] which were ranked among the best of 25 different assessment scales in a recent review.
A few questions to ask during this process may be:
- Do you have a sense of meaning and purpose? What gives you that sense?
- What does spirituality mean to you?
- Were you ever a member of a faith community?
- What gives you strength during difficult times in your life?
- What motivates you to fight for your health?
- What are your greatest challenges?
- Are there specific practices or restrictions I should know about in providing care?
If Veterans identify as Black, Indigenous, People of Color (BIPOC), LGBTQIA, or Non-Binary, it is important to understand that they often face unique stress, trauma, and the burden of having the educate others about their lived experiences. To guide clinicians with lines of inquiry regarding spirituality, dozens of assessment tools have been created. Commonly used tools include FICA,[623] HOPE,[624] FAITH,[625] and SPIRIT,[626] which were ranked among the best of 25 different assessment scales in a recent review. Note that these tools are only used to get general information about patients; again, if a spiritual assessment is needed, connect the Veteran with a chaplain or official in their religious community.
Each Veteran’s preference for spiritual care must be screened as part of a complete evaluation of the individual’s health care needs. A spiritual care screening question may be asked by providers for the purpose of determining whether the Veteran has spiritual concerns that affect the Veteran’s health care, has needs for accommodation of free exercise of religion or desires immediate spiritual care. A recommended screening question is: “Are there religious practices or spiritual concerns you want the chaplain, your physician, and other health care team members to know about?” The Veteran may decline to answer a screening question. If the Veteran gives a positive answer to the screening question and a more in-depth spiritual assessment is indicated, the provider must consult Chaplain Service. It is imperative that providers be sensitive and careful in their approach to patients as patients in spiritual or medical distress are often vulnerable. It goes without saying that a clinician should NEVER attempt to impose his or her beliefs on a patient; proselytizing is not appropriate.7,[627] A VHA chaplain is the only subject matter expert authorized to conduct the spiritual assessment, devise a spiritual care plan, and provide appropriate spiritual care as desired by the Veteran.69 (VHA Directive 1111, Spiritual Care, dated July 21, 2021).
If your time is limited and you only have time to ask one specific question about spirituality, consider one of the following:
- Are you at peace? This question has been found in the research to be a useful means for quickly determining if someone is in spiritual distress.[628]
- What gives you your sense of meaning and purpose? This is perhaps more widely used, but not as frequently studied.
- Or, as it is asked in the first question in the Personal Health Inventory (PHI), What really matters to you in your life?
Key Research about Spirituality and Religiosity
Spirituality and religiosity play an important part in health. Data from the Nurses’ Health Study, which focused on over 74,000 participants over 16 years, found that mortality rate for those who attended weekly religious services was 845 deaths per 100,000 people per year, compared to 1,229 for those who had never attended.[629] This represents a hazard ratio of 0.74. There seems to be a dose response too meaning that attending more than one service per week lowered the mortality risk even more.
A 2011 meta-analysis reported an 18% reduction in mortality for people who report being religious and/or spiritual.[630] They noted the benefit of being religious/spiritual was equal in benefit to consuming fruits and vegetables to prevent cardiovascular events. It was also noted that having high levels of religiosity/spirituality had as much or more of an impact on health as having air bags in your car, taking angiotensin receptor blockers for heart failure, taking statin drugs for cholesterol in people without heart disease, or being revived by a defibrillator outside of a hospital. This is not to downplay the importance of those other interventions; rather, it is an acknowledgment that Spirit and Soul can have a powerful effect on health and well-being.
Another study that followed nearly 5,300 adults for 28 years concluded that those who attended religious services one or more times weekly had, on average, a 23% lower mortality rate.[631] This was after correcting for age, sex, education, ethnicity, baseline health, body mass index, and even social connection, which is often thought to be one of the key elements of religious practices that contributes to health benefits. Similarly, a meta-analysis of nearly 126,000 people found that people who met criteria for being “highly religious” had rates of survival that were 30% higher as compared with those who rated themselves as less religious.[632]
Beyond attending religious services, having “a higher purpose in life” is also linked to better survival. A meta-analysis that included 10 studies with over 136,000 participants found that those with a sense of “higher purpose” had a relative risk of death or cardiovascular events of 0.83.19
Coping
Religiosity and spirituality have been found to help people cope with many problems, including the following9,Error! Bookmark not defined.:
|
|
|
Pain
With respect to pain, prayer has been identified as the most frequently or second most frequently-used strategy; over 60% of chronic pain patients report that they use prayer to help them cope.[633] The 2010 Baylor Religion Survey reported that 87% of respondents had prayed for other people, 79% had prayed for themselves at some point, and 26% had tried laying on of hands.[634] In most prayer studies, it seems to be a positive resource for reducing pain and improving well-being and mood.[635] What form prayer takes will vary based on a person’s religious/spiritual background.
Accessing religious and spiritual resources has been linked to decreased severity of arthritis pain, chronic pain, migraines, and acute pain.22 Often, it seems that it is not that the pain level is decreased so much as that a person’s ability to tolerate the pain is improved.[636] A 2020 systematic review concluded that prayer emerged as a preferred option for people who wished to use it prior to having surgery or a painful procedure; researchers noted the effects did not seem to be opioid-mediated.[637]
Mental Health
Over 80% of studies of religion and spirituality focus on mental health-related topics.9 A 2011 meta-analysis of psychotherapy that incorporated religious and spiritual perspectives found “enhanced psychological outcomes.”[638] Two other reviews have concluded the same.[639],[640] The National Health and Resilience in Veterans Study reported in 2017 that high levels of religiosity and spirituality markedly decreased lifetime risk of posttraumatic stress, major depressive disorder, alcohol-related problems, and suicidal ideation.[641] Well-being, hope and optimism, volunteering and altruism, a lower incidence of depression, reduced anxiety, less substance use, and decreased suicide risk are all associated in the literature with higher levels of religiosity and spirituality.Error! Bookmark not defined.,[642] A 2019 review found that about half of 152 prospective studies reviewed predicted a “significant but modest” decrease in depression over time.[643] A European study of nearly 24,00 people found that religiousness is associated with lower odds of depressive symptoms, particularly if people attended religious services.[644] More than 130,000 (73%) addiction treatment programs in the U.S. include a spirituality-based element.[645]
One valuable conclusion of such studies is that “the incorporation of religion and spirituality into psychotherapy should follow the desires and needs of the client.”[646] Table 11-2, later in this chapter, has more information on research regarding religion and spirituality and mental/behavioral health conditions.
Health Behaviors
Religion and spirituality also influence health behaviors.15 Religious people smoke less and exercise more, and in a 2012 review, 13 out of 21 studies found a link between higher levels of religiosity/spirituality and a healthy diet. Of note, religious/spiritual people tend to be at higher risk for obesity, with the exception of people who are Amish, Jewish, or Buddhist.70 42 of 50 good-quality studies found being religious strongly correlated with safer sexual practices as well.
Prayer May Help
Studying prayer is challenging, because there are different ways to pray, and a person may not be focused on something related to health when they are doing it. An early study of a group of coronary care unit patients found that people who were prayed for did NOT have lower mortality rates, but they needed fewer antibiotics, did not require intubation (as did many people in the control group), and were less likely to develop pulmonary edema.[647] A 2019 study involving a “contemporary, multiracial cohort” of 1039 people who were hospitalized for acute coronary syndromes (e.g., heart attacks) found physical and disease specific quality of life was better for those who either prayed for themselves or were prayed for by others.[648] This was after controlling for “sociodemographic, psychosocial, and clinical” characteristics.
Other Benefits
A 2005 systematic review found that religious activity may improve rates of in vitro fertilization, decrease hospital length of stay, increase immune function, improve rheumatoid arthritis symptoms, and reduce anxiety.[649] Religiosity and spirituality improve quality of life in people with cardiovascular disease.[650] A study that followed a diverse group of 16,000 elderly adults over 6 years found that religious attendance and private prayer were independently associated with better cognitive health, particularly in people who were Hispanic or black.[651] Addressing spirituality in both caregivers and patients during palliative cancer care can make care more effective.[652]
Prayer and meditation activate the prefrontal part of the brain, and they increase blood flow to the frontal cortex, the cingulate area, and the thalami.33,[653] Some spiritual practices increase flow to the superior parietal cortices, and this is linked to people having a sense of losing their physical boundaries. Higher dopamine levels correspond to higher levels of religiosity and spirituality. People whose dopamine levels decrease (e.g., with the progression of Parkinson’s disease) often become less religious and spiritual.Error! Bookmark not defined.
Nine Tips for Working with Spirit & Soul in Personal Health Planning
Keep the following tips in mind as you consider how to incorporate Spirit and Soul into health plans.
1. Meet people where they are
According to a study published in 2020, among all U.S. adults 75% subscribe to a religious tradition. Roughly 70% of those are Christian, 5% are other religions (Jewish, Buddhist, Muslim, Hindu), and 23% are unaffiliated (atheist, agnostic, or “nothing in particular”).[654] Of the unaffiliated people, 18% described themselves as religious, 37% said they were spiritual but not religious, and 43% said they were neither.[655] 94% regard their spiritual health to be as important to them as their physical health, and each year, at least 25% of patients use prayer for healing.[656]
In other words, patients are often spiritual and/or religious, and they want that to be reflected in their health care. In one survey, 83% of patients felt that physicians should consider their spiritual needs as a part of medical care.[657] In a survey of 177 outpatients in a pulmonary clinic, two thirds said they would welcome questions about spirituality in a medical history; 16% said that they would not.[658] In another study, 28% of people said they would want their physician to pray silently with them.[659] The sicker people are, the more they seem to want their physicians to discuss spirituality, and the interest increases if people are nearing the end of their lives.46 A 2017 study found that 65% of physicians in a multispecialty referral center believe in God.[660] 45% reported praying regularly, and 21% had prayed with patients.
The Six Types of Spirituality—An ExerciseError! Bookmark not defined.
As you consider spirituality as an element of self-care, it is especially important to appreciate how much variety there is when it comes to people’s beliefs. Some clinicians find it helpful to frame this based on different forms that spirituality can take for people. Six are listed here, but the list is by no means all-inclusive. Note, too, that these are not mutually exclusive. For instance, a person can be very religious and through this, feel the close connection to people that might be called humanistic spirituality. Read about each type, and as you do, ask yourself which of them resonate the most for you personally.
- Religious spirituality—closeness and connection to the sacred as described by a specific religion. It fosters a sense of closeness to a particular Higher Power. Note that the other elements of spirituality listed here are common to many different religious traditions.
- Humanistic spirituality—closeness and connection to humankind. It may involve feelings of love, reflection, service, and altruism.
- Nature spirituality—closeness and connection to nature or the environment, such as the wonder one feels when walking in the woods or watching a sunrise. This is an important focus for many traditional healing approaches.
- Experiential spirituality—shaped by personal life events; it is influenced by our individual stories. Many Veterans’ find their spirituality is profoundly influenced by their experiences during wartime.
- Cosmos spirituality—closeness and connection to the whole of creation. It can arise when one contemplates the magnificence of creation or the vastness of the universe (e.g., while looking skyward on a starry night).
- Spirituality of the mysterious—there is much that we simply cannot know or understand; it is not possible to fully grasp or know all the answers, and it is necessary to allow space for the unknowable.
2. Remember there can sometimes be negative aspects to spirituality and religion
For all the favorable data, keep in mind that not all religious and spiritual practices are without medical consequences. For some, spirituality and religiosity tie in with negative past (or present) experiences. In rare circumstances, because of their beliefs, people may:
- Fail to seek care altogether
- Ignore or promote child abuse or religious abuse
- Refuse blood transfusions
- Refuse prenatal care
- Replace much-needed mental health care with religious practices
- Stop potentially life-saving medications
Spiritual struggles and distress can be linked to poorer health outcomes (mental and physical), and therefore, addressing them is of great importance.[661] Some people may choose—or be forced—to join a group that is more cult-like in nature and likely to have negative effects on health. Once again, the key is to ask questions about this area and tailor the PHP based on each individual’s unique responses. As mentioned previously, it goes without saying that a clinician should NEVER attempt to impose his or her beliefs on a patient; proselytizing is not appropriate.7,[662]
3. Consider “pathologies” of the spirit and soul
Spiritual distress and spiritual crisis occur when individuals are unable to find sources of meaning, hope, love, peace, comfort, strength and connection in life, or when conflict occurs between their beliefs and what is happening in their life. This distress can have a detrimental effect on physical and mental health. Medical illness and impending death can often trigger spiritual distress in patients and family members.7
The previous section described research regarding the health effects of spirituality for specific physical and mental health conditions. In addition, there are many challenges—some refer to them as pathologies—that are specifically spiritual in nature. People experience conditions that may not show up during a physical exam, lab testing, or on a standard health questionnaire, but they are no less important to address.
A review of 11 studies of people’s spiritual needs in health-related situations concluded that there are six aspects of spiritual care that are most important to people and should be high priorities for clinicians (in this study, social workers)[663]:
- Meaning, purpose, and hope
- Relationship with God (or other Higher Power)
- Spiritual practices (and being able to follow them despite health conditions)
- Religious obligations (and, again, being able to meet them despite health conditions)
- Interpersonal connection
- Interactions with health care team members
Table 11-2 lists specific spiritual concerns that may arise for patients and questions they might lead them to ask.[664],[665],[666]
|
Concern |
Examples of Patient Questions or Statements |
|
Spiritual isolation |
“I feel like I don’t belong on this earth.” “Is God pleased with who I am?” “I feel so alone.” |
|
Spiritual disconnection |
“Why do I feel abandoned by my Higher Power?” “I feel disconnected from myself, from others.” “God has forgotten about me.” |
|
Spiritual anxiety |
“Will I ever find forgiveness?” “There is so much that I don’t know.” “Do I have a purpose in life?” |
|
Spiritual guilt |
“Am I being punished?” “Did I not do something well enough or correctly in my life?” “I regret so much.” |
|
Spiritual anger |
“I am angry with God/the Universe.” “I hate God for not answering my prayers.” “I feel betrayed.” |
|
Spiritual loss |
“I feel empty.” “Why don’t I care anymore?” “I am not sure what matters anymore.” “My sorrow is overwhelming.” |
|
Spiritual despair |
“There is no way a Higher Power could ever care about me.” “I have lost my hope.” “Things feel meaningless.” |
Recognizing the presence of these concerns when they arise in a PHI or during a Whole Health conversation will guide what will be included in the PHP, including the decision to consult with a chaplain or other spiritual care expert.
4. Know when to bring in assistance
At some point during an illness, a person may reach a point where self-reflection and trying to come to terms with their values becomes central to their well-being.[667] When true spiritual distress arises, it is important to involve others with additional expertise. The chaplain can provide care for the patient in their spiritual distress or connect the patient with someone from the clergy, a spiritual director, a traditional healer, or others with expertise in these matters, depending on the patient’s background and preferences.
Chaplains. Chaplains can serve as important members of the team. There is an extensive chaplaincy network within the VA system. Chaplains are professionals—members of the clergy—who have received advanced training working with people in health care settings. Board certification, required for all chaplains, requires completion of 1,600 hours of supervised clinical pastoral education training in an accredited hospital-based program. In VA facilities, chaplain coverage is available every day, 24 hours a day.
Chaplains can offer many services, including the following[668]:
- Helping to integrate spiritual care with care of body and mind
- Assisting patients with making difficult decisions (primarily by being a sounding board rather than by telling them what to do)
- Contextualizing illness for a patient in terms of his/her personal spiritual practice or religious perspectives; helping someone explore the question, “Why is this happening to me?”
- Assisting with conflict resolution in patient care
- Supporting hospital staff and family members when they are in need
Important examples of situations when it would be helpful to ask for a chaplain’s assistance include55:
- Someone requires additional assistance exploring the meaning of what is happening to them.
- A patient, family member, or care team member displays symptoms of spiritual distress. These include the following55:
- Expressing a lack of meaning and purpose, peace, love, self-forgiveness, courage, hope, or serenity
- Feeling strong feelings of anger or guilt
- Displaying poor coping strategies
- Struggling with moral injury. For example, profound ethical and moral challenges related to participation in war that can compromise psychosocial and spiritual health in Veterans.[669] Spirituality and religiosity can both exacerbate and ease struggles with moral injury.[670]
- A caregiver or family member needs support with coping with the illness or death of a loved one.
- A patient’s care involves circumstances where ethical uncertainties or challenges have arisen.
- A patient (or family member, with the patient’s permission) desires to connect with clergy from their religious group or wishes to have a particular ceremony, rite, or holiday observance performed.
- It might be helpful if a patient receives a new diagnosis, such as terminal cancer, severe depression, anxiety, or a chronic illness like type 1 diabetes, which can be life-altering.
- A patient is struggling with problems related to forgiveness.
- A patient distrusts medical provider based on long-held beliefs and lived experiences of systematic discrimination in health care.
- A patient is coping with their lived experiences, gender identity, sexuality, SES, race and ethnicity, generational trauma, or mental challenges.
A 2014 study involving a group of primary care centers in England found that, even after controlling for numerous variables, there was a significantly positive relationship between well-being scale scores and having had a consultation with a chaplain.[671] A 2013 survey of VA chaplains found that chaplains most commonly saw patients in the VA for anxiety, alcohol use disorder, depression, guilt, anger, PTSD, and to help them as they struggled with understanding why loss or trauma happened in the first place.56 The “Spirit and Soul” overview provides additional information and research related to chaplains.
5. Discuss forgiveness, if appropriate
This is discussed in more detail in Chapter 7, “Personal Development.” Studies indicate that people who are more inclined to forgive have lower blood pressure, less muscle tension, a healthier heart rate, and lower overall numbers of diagnosed chronic conditions.[672],[673] Interpersonal forgiveness is an important concern for people with cancer.[674] Having “trait forgiveness” reduces risk of burnout in physicians.[675] Of course, how forgiveness fits into a person’s perspective will determine whether or not a clinician raises the topic during personal health planning or refers them to a chaplain or other expert in working with forgiveness. Certainly, forgiveness receives different emphasis in different spiritual traditions. Forgiveness takes time, and clinicians who support the process should be very familiar with what it entails. The Whole Health Library tool, “Forgiveness: The Gift We Give Ourselves,” has more information.
6. Ask if it would be helpful to add a spiritual practice
What a spiritual practice looks like will vary from person to person. It is extremely important that care team members separate their personal practices or beliefs from this discussion. Some people may choose to join a particular spiritual group or community, be it a church, a scripture study group, or even a 12-step program. Others may wish to find a teacher who will work with them individually, or they may choose a solo practice, such as praying or meditating quietly on their own on a regular basis. It may be helpful for clinicians to briefly describe a variety of spiritual practices that other Veterans they have worked with have found helpful. Time in nature can be a rewarding spiritual practice in and of itself, as can various creative pursuits. Trust that patients will have insights into what works best if you simply bring up the topic.
7. Avoid pitfalls along the way
There are some actions it is best not to take when focusing on Spirit and Soul. Take care not to proselytize. It is not helpful to try to impose your perspectives on others. Do not try to resolve unanswerable questions—you do not need to have the answers to help someone else. It also is best not to say any of the following[676]:
- “It could be worse.”
- “We are all out of options.”
- “It’s God’s will.”
- “I understand how you feel.”
- “We all die.”
8. Work with Spiritual Anchors
A spiritual anchor is an object, a person, a practice, or some other item that serves as a trigger to remind you of what matters most. You, your colleagues, and your patients are encouraged to work through the “Spiritual Anchors” Whole Health tool, featured below.
9. Know about values
The straightforward act of asking “What really matters?” can often help you learn about another person’s values. Sometimes, though, people freeze, or they feel overwhelmed by possible answers. It may help for them to do some exercises to help them explore what they value as reviewed in the “Values—Figuring Out What Matters Most” Whole Health tool, which is featured later in this chapter.
 Whole Health Tool: Spiritual Anchors
Whole Health Tool: Spiritual Anchors
As clinicians, we continually witness the highs and lows of human existence; we confront suffering, experience a great deal of stress, and are often pushed to the limits in terms of our emotional and physical stamina. Having spiritual anchors available is one way to ground ourselves in what really matters during challenging times. Spiritual anchors can also serve to bring our patients to bring themselves back to what really matters to them as well.
At the completion of the Healer’s Art elective course, medical students are given a small item, perhaps a small plush heart sewn by a volunteer. This is their “anchor,” something that they can carry with them on the wards to remind them of what matters most to them during challenging times. It can be helpful, as part of a Personal Health Plan (PHP), for a person to choose an anchor and carry it with them. The following are some tips for working with a spiritual anchor:
- Choose an object that reminds you of what gives you meaning and purpose. It should symbolize health and well-being for you in some way. Examples are:
- A photograph of a loved one
- A stone from a favorite place
- A special piece of jewelry
- A copy of a poem or piece of artwork
- Something written by a loved one or teacher
- Keep that object with you. Wear it, carry it in your wallet or purse, put it in your pocket, or display it in a place at work where you spend a significant amount of time. Make a treasured photo into your screen saver. The key is to have it situated where you can bring your awareness to it as needed.
- Tell others about your object, if appropriate. A powerful group activity involves each member of a group sharing about their object with others, if they feel comfortable doing so. Sharing should be done in relatively small groups with a respect for confidentiality. If this is done, remind people not to interrupt the sharing, and designate a specific amount of time for each person to share. When people share, they can describe the history of their anchor (what it is, where they got it), why it matters to them, and how they keep it in their awareness (e.g., they may place a photo where they will always see it when they open a wallet, or keep something in their pocket where they frequently will notice it.)
- Consider other options, if you prefer. While many people find it is helpful to have a physical object as an anchor, there are other types of anchors as well. Examples include the following:
- A breathing exercise that you can use when things become stressful.
- A gesture, hand movement or body position that can serve as an anchor. In some mindful awareness practices, mudras—special hand positions—are used. Placing one’s hand over one’s heart can also be a powerful reminder to bring the heart back into a given experience.
- A mindful awareness practice that can be done routinely. For example, during a difficult situation, a person might do a loving-kindness meditation or compassion practice, as described in Chapter 10. Another option is for clinicians to pause and ground themselves with a deep breath every time they cross a threshold into a new room.
- Going to a specific location can also be helpful. Every VA Hospital has a chapel or meditation room a person can visit from time to time. Many facilities also have gardens or lawns with benches.
- A specific song. In this era of smartphones and laptops that have music files, taking a few minutes to play a favorite piece of music can serve as an excellent anchor.
- Prayer, taking a moment of silence, or simply being still, when appropriate. How this is done is a matter of personal preference. Some clinicians set the intention to simply think “I wish you well,” or “I wish you your highest good” every time they come into contact with a new patient or colleague.
- Working with a word or concept. Examples might include cooperation, determination, appreciation, dedication, investigation, inspiration, passion, compassion, and perfection, among others.[677]
Experiment with using an anchor yourself and explore using them with your patients. Doing so can be a useful means of bringing what really matters into daily life.
 Whole Health Tool: Values—Figuring Out What Matters Most
Whole Health Tool: Values—Figuring Out What Matters Most
When you think about your Whole Health, one of the most important questions to ask yourself is, “What really matters to me?” In other words, what do you value the most?
Each of us has a unique answer to this question. One person might mention loved ones, while another person might mention a dream or goal they have. Some people answer that it is tied to their spiritual beliefs, while others may focus on something they want to do to help other people. The key is to find the best answer for you, and some people need some time to think about this. The exercises below were created to help you learn more about your values.[678] Choose one and see what you learn.
Values Exercise 1: The “Sweet Spot”[679]
Think of a time when you had one the richest, most beautiful experiences of your life. As you remember, use all of your senses. What did things look like? What did you hear? What do you recall in terms of smell, taste and touch? Note what thoughts come up, and what feelings. Write down or say out loud what comes up and talk about it like it is happening right now. “I am noticing…” “I see and hear…”
Ask yourself the following questions. It can help to jot down notes about the following:
- Why you chose that memory?
- What made it special?
- What did you do during this moment?
- What was it about you that helped make the moment so good?
- How were you treating other people, yourself, and the world around you at the time?
The answers that you write down can help you know more about your values, about what really matters to you.
Values Exercise 2: Happy 90th Birthday!
Picture yourself at your 90th birthday party. Everyone your life has ever touched is there. They are talking about you. If they shared a few statements that described the life you led, what would you want them to say? There are no limits. What would you want to be remembered for? Write down, type out, or record a few things you would want people to say about you. The things you make note of can give you some ideas about what really matters, what you value the most.
Values Exercise 3: Top Ten, Three[680]
This exercise takes a bit more time, but it can be very powerful. Below is a list of common values people have. If you don’t know the meaning of a word, just skip to the next one. Start by circling the ten values that matter most to you in your life. Next, narrow it down to five, then three. Why did you choose those? Can you narrow it down to just one?
Important Personal Values
|
|
|
|
Spirit & Soul Resources
Websites
VA Whole Health and Related Sites
- A Patient Centered Approach to: Spirit and Soul. Part of the Components of Health and Well-Being Video Series. https://www.youtube.com/watch?v=pN1tespCmD4&feature=youtu.be
- National VA Chaplain Service. http://www.va.gov/chaplain/
- Veterans Whole Health Education Handouts. https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
- An Introduction to Spirit and Soul for Whole Health
- Deciding What You Need for Spiritual Health
- How Do You Know That? Beliefs and Your Health
- Spiritual Anchors
- Chaplains
Whole Health Library Website
- Spirit and Soul. Overview. https://wholehealth.wisc.edu/overviews/spirit-soul
- Assessing Your Beliefs about Whole Health. https://wholehealth.wisc.edu/tools/assessing-your-beliefs-about-whole-health
- How Do You Know That? Epistemology and Health. https://wholehealth.wisc.edu/tools/how-do-you-know-that
- The Healing Benefits of Humor and Laughter. https://wholehealth.wisc.edu/tools/healing-benefits-humor-laughter
- Creating a Gratitude Practice. https://wholehealth.wisc.edu/tools/creating-gratitude-practice Forgiveness: The Gift We Give Ourselves. https://wholehealth.wisc.edu/tools/forgiveness-the-gift-we-give-ourselves/
- Values. https://wholehealth.wisc.edu/tools/values
- Personal Health Plan Template. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/08/Brief-Personal-Health-Plan-Template.pdf
- Whole Health for Skill Building: Spirit & Soul. https://wholehealth.wisc.edu/courses/whole-health-skill-building/
- Faculty Guide
- Veteran Handout
- PowerPoints
- Mindful Awareness Script: Using Writing in a Mindful Awareness Practice
Other Websites
- Duke Center for Spirituality and Health. http://www.spiritualityandhealth.duke.edu
- Spirituality and Health Magazine. www.spiritualityhealth.com
- Spirituality and Practice. Provides information on books, films, and other media that tie into spirituality. http://www.spiritualityandpractice.com.
- Spiritual Competency Resource Center. The organization also offers course and materials specific to the topic of forgiveness. http://www.spiritualcompetency.com/
- University of Minnesota Earl E. Bakken Center for Spirituality and Healing. www.csh.umn.edu
Books
- A Path with Heart: A Guide Through the Perils and Promises of Spiritual Life, Jack Kornfield (1993)
- A Year to Live: How to Live This Year as if it Were Your Last, Stephen Levine (1998)
- Being Mortal: Medicine and What Matters in the End, Atul Gawande (2014)
- Care of the Soul: A Guide for Cultivating Depth and Sacredness in Everyday Life, Thomas Moore (1994)
- Dying Well: Peace and Possibilities at the End of Life, Ira Byock (1998)
- Essential Spirituality: 7 Essential Practices to Awaken Heart and Mind, Roger Walsh (2000)
- Final Gifts: Understanding the Special Awareness, Needs and Communications of the Dying, Maggie Callanan (2012)
- Healing Words: The Power of Prayer and the Practice of Medicine, Larry Dossey (1997)
- Messy Spirituality, Mike Yaconelli (2007)
- My Grandfathers Blessings: Stories of Strength, Refuge, and Belonging, Rachel Remen (2001)
- Nurturing Spirituality in Children, Peggy Jenkins (2008)
- Spirituality in Patient Care, Harold Koenig (2013)
- The Biology of Belief, Bruce Lipton (2007)



















