Passport to Whole Health: Chapter 8
Chapter 8. Food & Drink: Nourishing & Fueling
Nothing tastes as good as healthy feels.
―Unknown
The Benefits of Healthy Eating
In an average lifetime, people in the United States eat around 35 tons (70,000 pounds) of food. [358] They will spend about 3 years and 8 months of their lives eating and drinking beverages (67 minutes a day), [359] and they will consume 152 pounds of sugar yearly (6 cups a week). [360] We make dozens, if not hundreds, of nutrition-related choices each day.
No one will deny that healthy nutrition is important, and that the choices you make have important consequences for your health. What you eat and drink nourishes your body and mind, and it has an influence on any number of health conditions. A 2015 study of nearly 216,000 people asked people to complete four diet quality surveys. Healthy diet scores were linked to lower risk of death from all causes as well as specifically from cardiovascular disease and cancer,[361] and an estimated 80,000 new cancer cases each year are linked to suboptimal diets.[362] A 2004 study concluded that 9% of mortality in women and 16% in men is linked to poor diet choices and noted that an increase in fruits, vegetables, whole grains, and lean meats markedly lowered one’s risk of dying.[363] Healthy dietary patterns have been associated with better overall health and quality of life.[364]
Obesity and diabetes rates are climbing. In fact, over 2/3 of U.S. adults and 1/3 of children are overweight or obese.[365] Rates of obesity are influenced by disparity; rates are higher in low-income populations and in certain racial and ethnic minority groups who are not socially advantaged.[366] Eating patterns are linked to blood vessel health, bone density, gut function, mental health, cancer risk, blood pressure, skin health, eye disorders, allergies, and many other aspects of health. Depending on what choices we make, our food and drink choices will either contribute to or prevent the development of chronic diseases, and they will influence how long we live.
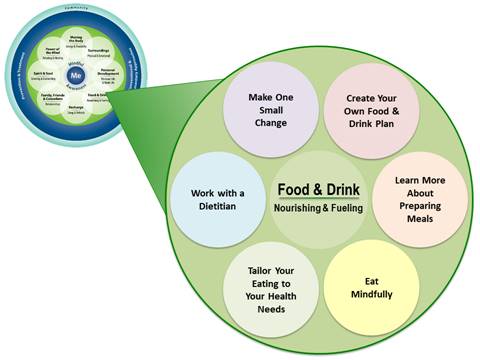
But where to begin? Everyone seems to argue about what good nutrition means. How does a person tailor healthy eating habits to their lifestyle? How do you sort through it all as you create a Personal Health Plan (PHP), respecting what tens of thousands of studies (some of which contradict each other) have to offer? One way is to start with the “subtopics” of Food and Drink, listed in Figure 8-1. As noted in previous chapters, subtopics were developed for each of the 8 self-care areas in the Circle of Health for the Veterans’ skill-building course as a way to get Veterans thinking about different options for the PHP. Note that there is a “Make One Small Change” circle that leaves room for creativity, if Veterans do not see an option that interests them.
Note too, the circle “Work with a Dietitian.” Remember, as you explore Food and Drink, to enlist the support of your local dietitians, keeping in mind that some of the diets listed in this chapter and in other Whole Health resources may be more or less familiar to various colleagues. Dietitians have devoted their careers to becoming experts on Food & Drink! Respect scope of practice as you guide Veterans to the clinicians who can be most helpful to them as they set—and follow through with—their nutritional goals. Many dietitians in the VA are now training or have trained in Integrative Functional Nutrition, allowing them to cultivate even more skills that are closely related to the Whole Health approach.
A useful source of ideas is the Eating for Whole Health: Nutrition for all Clinicians course. In 2017, OPCC&CT collaborated with VA’s Nutrition and Food Services leadership and clinicians with a background in Integrative Health and Functional Nutrition to create the course. The following topics covered in Eating for Whole Health can provide additional ideas about what could be discussed with a Veteran:
General Guidelines
- Follow a specific eating plan
- Macronutrients (fats, carbs, etc.)
- Micronutrients (e.g., vitamins) <>Phytonutrients (from plants)
- Common Diets
- Nutrigenomics
Mindful Eating
- Start a daily practice
- Number of chews
- Pacing eating
- Eating without distractions
- Observing cravings
- Stress management
Cooking Tips
- Grocery shopping
- Try a new recipe
- Cooking classes, including with Healthy Teaching Kitchens
Prevention (seek dietitian support)
- Diet and cancer risk
- Diet and vascular disease
- Diet and blood glucose
- Other health conditions
Nutrition for Specific Health Conditions
- Referrals to dietitians (especially important for this topic)
- Diet and depression
- Diet and sleep
- Diet and pain
- Eliminating certain foods
- Probiotics
Food Preparation Tips
- Grocery shopping
- Using kitchen tools
- Cooking tips to maximize nutrient quality
- Cooking classes, including with Healthy Teaching Kitchens
Food in Context
- Food access and food deserts
- Food safety: nutrition composition, growing methods, toxicity, chemicals
- Food and social connection
Nutrition Resources
- Cookbooks
- Recipes
- Websites
- Nutrition classes
- Community programs
Nutrition Assessment
Healthy eating begins with obtaining good, individualized information about a patient’s eating patterns and preferences. You can do this when you gather a history, and you can also have them complete a food diary or various questionnaires in advance.
Questions to Ask About Food & Drink
When you are talking to someone about Food and Drink, consider asking some of the following questions:
General
- Do you have any concerns that you believe are related to the way you eat?
- How would you describe your relationship with eating?
- Are you satisfied with your eating habits? Why or why not?
- Do you ever skip a meal? How often, and which meals?
- What is typically your biggest meal?
- What are your favorite foods? What don’t you like?
- What would you like to focus on today, in terms of your nutrition?
- Why is healthy nutrition important to you?
Eating and Drinking Patterns
- What is your eating pattern? How many meals do you eat a day, and when do you eat them?
- Have you recently changed the way you eat? If yes, for what reason?
- Do you follow a specific diet? Vegetarian? Low carb? Mediterranean?
- How often do you eat out? What types of restaurants (fast food, fast casual, casual, fine dining)? What do you usually order?
- How often do you eat fast food? What do you usually get?
- How much water do you drink in a day?
- Do you drink anything else regularly (e.g., sodas, alcohol, caffeinated drinks, juice, sports drinks)?
- Do you ever eat when you are not hungry?
- Do you ever wake up in the middle of the night and eat?
- Do you ever binge eat?
- What is the most important thing for me to know about the role food plays in your life?
- What do you typically eat for breakfast? Lunch? Dinner? Snacks?
- Do you ever skip meals or fast?
- What are your comfort foods?
- Are you taking any vitamins, minerals, or other dietary supplements? Why?
Eating and Body Weight
- Have you been eating more or less than normal? If yes, for what reason?
- What is your usual weight?
- Have you gained or lost weight recently?
- What is your highest weight in adulthood? When were you that weight?
- What is your lowest weight? When were you that weight?
- Have you ever tried to intentionally lose weight? How much? If you succeeded, did you ever regain it back? How much? Why was it regained?
- What weight loss strategies (diets, exercise programs, etc.) have you used?
- Do you have the same body type as anyone else in your family?
Context for Eating
- Who are the members of your household? Who does the food shopping and preparation?
- Do you share your meals with others? Who?
- Who participates in food choices and mealtime in your household?
- Are the other members of your household supportive of your efforts to make dietary changes?
- Where do you eat? (At the kitchen/dining room table, in front of the TV/computer, in the car, at your desk, etc.)
Mindful Awareness and Nutrition
- Sometimes hunger is physical, but it can also be emotional or mental. When you eat, what part of yourself are your feeding?
- Are you an emotional or stress eater?
- Are you conscious of your cravings? What do you tend to crave and when?
- What factors influence how you choose your food?
- Do you do other activities, like driving, working, or watching TV while you are eating?
- How do you feel after eating? Physically (e.g., satisfied, stuffed, still hungry)? Emotionally (e.g., content, guilty, angry)?
Nutrition and Symptoms
- Are there any foods that do not agree with you?
- Do you have any food allergies, intolerances, or sensitivities that you are aware of? What reactions have you noticed?
- Do you think what you eat plays a role in how you are feeling?
- Have you noticed that what you eat, and drink affect your sleep?
- Do you ever feel like particular foods cause you to have more or less pain?
- Do any foods give you heartburn, gas, bloating, diarrhea or constipation? How soon after eating these do you notice these symptoms?
Food Diaries
Food diaries can also be a powerful tool for gathering more information about Food and Drink. Having a person keep track of what they eat and drink can help you watch for certain patterns, and this can be done on paper, using web-based tools, or with apps.[367] Ideally, a food diary, kept over 3-5 days, can be useful. However, if that is not possible, doing a 24-hour food recall can also be of value. Assess when they eat, what they eat, and how much they eat. It can also help for people to describe how they were feeling as they ate as well as document times when they were physically active or asleep. Documenting any symptoms, they notice (and when they have them) can also be helpful.
As you look over a completed food recall, consider each of the following as topics to ask them about:
- Overall calorie consumption and portion sizes
- Proportions of macronutrients—carbohydrates fats and proteins—they eat
- Number of servings of fruits, vegetables, and nuts they consume
- Omega-3 fat intake
- Fiber intake
- How often they eat out versus cooking for themselves
- How pro- or anti-inflammatory their diet is (This is discussed in more detail later in this chapter.)
- Meal frequency and timing. Are there any indications of skipped meals, nighttime eating, or binge eating? (There are a number of recent articles about binge-eating disorder.)[368]
- Length of time spent eating
- Whether they primarily eat alone or with others
- The degree to which they are eating mindfully. Are they doing other activities (watching TV, working at their desk) during their meals?
- Where they get their food. Do they have trouble affording good food? Do they live in a “food desert”?
Any of these questions could be a starting point for creating a PHP. It may not be practical to ask them all, but even asking one or two can bring awareness to ways to eat more healthily. The Resources section at the end of this chapter includes links to food diary forms and other resources that can help with Whole Health Assessment for Food and Drink.
The sheer number of suggestions you can make regarding nutrition can feel overwhelming. Take it step by step, and remember, any one suggestion is a step in the right direction. Most people do best making small, incremental changes.[369] Don’t forget about having a dietitian as part of the team, especially if eating is a major stumbling block for someone.
Six Guidelines for Food & Drink
The following are some guidelines you can follow as you incorporate Food and Drink into personal health planning[370]:
- Guideline 1. Be Clear Right Away About Motivation to Change
- Guideline 2. Incorporate Mindful Eating
- Guideline 3. Be Realistic About Vitamins and Minerals
- Guideline 4. Be Able to Discuss Specific Eating Plans
- Guideline 5. Come Up with a List of Your Favorite Cookbooks, Recipes, and Cooking Websites
- Guideline 6. Develop a List of Your Favorite Eating Tips for Patients
Each of these is covered in more detail below.
1. Be Clear Right Away About Motivation to Change
You can ask people to rate the importance of making a Food and Drink change on a scale of 1-10. The Importance Scale is featured in Chapter 3. Most people do best if they focus on one change—one SMART goal—at a time. SMART goals are also discussed in Chapter 3. Examples of goals a person could consider include the following:
- Focus on a certain number of servings of fruits and vegetables each day. Consuming 7-10 servings is a good ultimate goal, but intake can be increased gradually. Starting with one more serving each day may be a good starting point.
- Change away from drinking sweetened sodas or other sugary drinks. Risk of type 2 diabetes increases by 18% for every additional sweetened beverage a person consumes each day.[371] There is a strong association between sugar-sweetened beverages and heart disease that is independent from a person’s weight.[372] There is also a dose-response increase with risk of non-alcoholic fatty liver disease,[373] and mortality rates increase in people who drink sugar-sweetened and artificially-sweetened beverages.[374]
- Choose one high calorie (or otherwise unhealthy) food that may be eliminated or reduced (e.g., peanut butter, cheese, donuts, or a snack food like potato chips). We know that higher intakes of fast foods (e.g., donuts) can increase risks for chronic problems such as depression.[375]
- Discuss modifying their daily or weekly number of servings of red meat, alcohol, simple carbohydrates, etc.
- Increase fiber intake to recommended daily levels, as appropriate. In addition to many other benefits, viscous fiber in the diet helps some with weight loss independently of calorie restriction.[376]
- Drink eight glasses of fluid (being careful about alcohol intake) daily. 20-30% of older adults are affected by dehydration.[377] Even a person who is not active requires an average of 1.5 liters of water daily.[378]
Remember, you aren’t doing this alone. Make use of your team. Specifically, if you are not a dietitian yourself, consider enlisting the help of a dietitian. Whole Health Coaches, if available, can also be incredibly helpful. And always—always—make the patient a part of decision making. If you are working harder than they are to set and achieve a nutrition goal, check back with them about how important the change truly is to them.
2. Incorporate Mindful Eating
Chapter 4 introduces the concept of mindful awareness. There are many ways to cultivate it, and mindful eating can be a powerful tool. People can learn to pay more attention to their eating patterns and why they choose to eat what they do. They are encouraged to explore what “hunger” actually means and how it may or may not connect calorie needs, or cravings, or emotional states.
Systematic reviews related to mindful eating show that it has promise for helping people with binge eating[379] and other eating disorders.[380] It favorably influences food intake.[381] Mindfulness-Based Eating Awareness Training (MB-EAT) is offered with increasing frequency in health care organizations and has shown benefit for stabilizing glucose levels in people with type 2 diabetes.[382] Mindful eating is linked to decreases in depression symptoms.[383] A 2018 review concluded that mindfulness-based interventions are effective for reducing weight and changing behaviors in people who are overweight or obese.[384] A 2020 study found mindful eating is particularly helpful for people who are compulsive eaters.[385] Canada’s national Food Guide now recommends mindful eating.[386]
Examples of mindful eating practices can include the following:
- Carefully observe each phase of eating. This includes noting the appearance, smell, and texture of the food, bringing it slowly to the mouth, and slowly chewing it and swallowing while paying close attention to taste. It may also include considering where the food came from or feeling gratitude for everyone who helped to produce it.
- Chew a certain number of times with each bite. A 2019 study found that specific chewing training had a strong positive effect on energy intake and enjoyment of eating.[387]
- Limit other activities while eating. This could mean not watching TV or reading while eating or being sure to be seated comfortably at a table during a meal.
- Experiment with eating in complete silence.
Electronic interventions to support mindful eating are increasingly available. More studies are needed, but they are a promising option.[388] Mindful eating resources are listed at the end of this chapter. The following Whole Health tool is an example of a mindful eating exercise.
 Whole Health Tool: Mindful Eating Exercise
Whole Health Tool: Mindful Eating Exercise
Eating has far-reaching health consequences for individuals, societies, and the planet. These consequences can be positive or negative depending on our patterns and choices. The following exercise can help you to bring more awareness to your eating behaviors, while helping you to cultivate present-moment awareness. It requires that you have a food of your choice.
- Sit comfortably, facing your food.
2. Minimize distractions. Avoid screens (e.g., phone, computer, television), background noise, printed materials, and other stimuli.
3. Note your internal state.
- Do you feel hungry? Thirsty?
- What is your emotional state—happy, sad, angry, frustrated, anxious, exhausted, energized, or neutral?
4. Look at what is on the table in front of you. Try not to label it as anything specific; rather, ask questions:
- How does it look? Is the color bright, dull, varied, or uniform?
- Does it appear hot, warm, or cold?
- Does it appear dry or moist?
- Do you detect an aroma from the food? How would you describe this aroma?
5. Take the first bite.
6. Put down whatever is in your hand—the food and/or your utensil. Note preliminary aspects of your experience with this first bite of food, including:
- Temperature. Frozen, cold, cool, warm, hot, or super-hot?
- Texture. Is it soft, firm, chewy, creamy, brittle, light, or dense?
- Flavor. Is it mild, bland, sour, sweet, savory, salty, spicy, pungent, or rich?
- Intensity. Mild, moderate, or extreme?
7. Take the first swallow.
- Is the food easy or difficult to swallow?
- How does this food feel passing from the mouth, to the esophagus, to the stomach?
8. Now take the next bite. With each subsequent bite, consider your ongoing experience with this food.
- Continue to note the temperature, texture, flavor, and intensity.
- How does this food feel in your stomach?
- How do you feel, looking at the remainder of your portion?
- At what point do you begin to feel full? At what point do you feel that your hunger is entirely satisfied by this food?
- At what point do you decide to stop eating this food?
9. After eating, note how you feel.
- Do you feel hungry, thirsty, satisfied, full, or overly full?
- What is your emotional state? Did your emotional state influence your eating in this exercise?
10. Close your eating activity with a deep breath before moving on with your day.
Eating with this degree of attention to your experience may initially seem cumbersome or frustrating, but with time you will appreciate a richer, more satisfying eating experience.
3. Be Realistic About Vitamins and Minerals
People tend to assume they need to take multivitamin and mineral supplements and that these are beneficial. It is usually best to get vitamins through food versus supplementation, but some groups may, in fact, need specific nutrients to be supplemented. For instance:
- People who eat limited amounts of animal protein (e.g., vegetarians and especially vegans) may need to supplement vitamin B12.
- Some people—especially women who menstruate heavily—may need iron.
- Prenatal vitamins can be very important for expectant mothers.
- A recent study found that people who are obese tend to be more deficient in fat-soluble vitamins, folic acid, B12, and vitamin C than those who are normal weight.[389]
- Community-dwelling older adults may be at risk for deficiencies of vitamin D, B1 (thiamine), B2 (riboflavin), calcium, magnesium, and selenium.[390]
However, there is limited data to show that vitamin and mineral supplements make a difference for the considerable majority of people.[391] A 2019 study using National Health and Nutrition Examination Survey data found no indication that dietary supplement use provided a mortality benefit.[392] Large-scale studies have not found an association between multivitamin use and mortality from all causes, cancer, or cardiovascular disease.[393] Most recommendations favor getting vitamins and minerals from foods whenever possible. The role of these various chemical compounds in various chemical pathways cannot be understated; they are vital for immune system regulation, production of various signaling molecules, brain function, regulation of pain, and any number of other physiological functions that are fundamental to good health. We know that they play key roles in healthy genetic expression as well; for example, they help to preserve telomere length, which correlates with better overall health and longevity.[394]
Different vitamins and minerals may be helpful in certain circumstances, and this can be explored on an individual basis. For example, a 2020 review and meta-analysis recently concluded that 500 mg of vitamin C daily led to a significant reduction of blood pressure in people with hypertension[395], and people with inflammatory bowel disease tend to be low in vitamin D.[396] Vitamin D is helpful in osteoporosis, but many factors (including dosing and individual fracture risk) come into play.[397]
4. Be Able to Discuss Specific Eating Plans
One of the most common questions that might arise during a Whole Health visit is, “So, what diet should I follow?” This is not an easy question to answer. In general, a simple answer is that any eating plan that is reasonable in terms of calorie content and nutritional quality may prove helpful. (Note that many dietitians and other clinicians prefer to use “eating plan” instead of “diet,” because the word “diet” has so many negative associations for people). The key is that a person must be consistent with following the plan; adherence is key. How well a person sticks to an approach to eating may be as important as the specifics of how they eat.[398] An extensive 2020 review looked at 14 popular diets followed by nearly 22,000 people in 121 trials.[399] They concluded that “Moderate certainty evidence shows that most macronutrient diets, over six months, result in modest weight loss and substantial improvements in cardiovascular risk factors.” At 12 months, the effects—and the benefits—have largely disappeared for most people.
As far as commercial weight-loss programs, a 2015 study reviewed 45 studies to see what programs were supported in the research up to that point.[400] Weight Watchers and Jenny Craig programs were found to lead to an average of 2.6% and 4.9% of weight loss, in studies that were at least 12 weeks long. Nutrisystem was also found to be promising.
A 2017 systematic review involving over 1.5 million participants focused on how much different eating plans affected risk for developing type 2 diabetes.[401] Relative risk of diabetes was 0.87 for people eating a Mediterranean eating plan, 0.79 for those using the Alternate Healthy Eating Index, and 0.81 for Dietary Approaches to Stop Hypertension (DASH).
It can be helpful to know where you can go to learn about the hundreds of different “fad” diets that come in and out of popularity. Some resources to help with that are listed at the end of this chapter.
In terms of recommending specific diets for Whole Health it is perhaps best, in the spirit of personalizing care, to explore with each individual patient what approach to eating might work best for him or her. Here are a few specific eating plans worth considering. They are referred to here as “diets” because that term is used for them in the medical literature. Check at your local facility to see what diets have been formally approved by NFS.
Mediterranean Diet
The Mediterranean Diet (MD) features[402],[403]:
- High consumption of fruits and vegetables
- Monounsaturated fats (mainly from olive oil)
- Whole grains and nuts
- Moderate intake of poultry, fish, and dairy with minimal consumption of red meat
- Good intake of water and moderate amounts of wine
- Cooking and eating at a leisurely pace, in the company of others
Despite some recent questions around methodology of an important 2013 study,[404] the MD has been linked to good overall health since it was first studied in the 1950s.[405] Data continues to come in regarding many of its favorable effects, which include the following:
- Similar weight loss and cardiovascular risk benefits to other popular diets, including the American Diabetes Association diet, low-fat diets, and low-carbohydrate diets.45 2019 Cochrane review noted that currently the data for a “modest benefit” is “low or moderate”[406]
- Reduced incidence of cardiovascular syndromes, neurodegenerative diseases, type 2 diabetes, and allergy,[407] as well as stroke[408]
- More healthy populations of microbes in the gut52
- Reversal of age-related cognitive decline[409] and potentially, prevention of Alzheimer’s disease[410]
- Decreased cancer risk. It lowers risk of overall cancer mortality by 10%, colorectal cancer 14%, prostate cancer 4%, and aerodigestive (e.g., mouth, pharynx, larynx) cancers 56%[411],[412]
The MD is, in essence, an anti-inflammatory diet.[413] The same is true for the Nordic Prudent diet, which is sort of the Baltic Sea/Scandinavian equivalent of the MD.[414] Of course, it is important to tailor a person’s approach to eating to their geographical location, what foods they have access to, and their food preferences. Respect the cultural, religious, and other social influences that affect each person’s food choices.
The Anti-Inflammatory Diet and Elimination Diets
The Anti-Inflammatory Diet (AID) is one of the most commonly used tools in Integrative Health practices. Eliminating problematic foods can also be helpful. Note that both of these are not formal eating plans per se, but overall approaches to eating that can be tailored to individual needs, when appropriate.
 Whole Health Tool: The Anti-Inflammatory Diet
Whole Health Tool: The Anti-Inflammatory Diet
What Is It?
The Anti-Inflammatory Diet (AID) is a general name for an approach to eating that is intended to decrease inflammation (and related pain).[415] It can have an impact on a number of chronic diseases, including asthma, arthritis, hypertension, COPD, diabetes, cardiovascular disease, peripheral arterial disease, obesity, irritable bowel disease (IBD), nonalchoholic fatty liver disease, cancer, dementia, psoriasis, and depression,[416] to name a few.
How It Works
- Certain essential fatty acids, including omega-6s and omega-3s, are used by the body to produce eicosanoids (e.g., prostaglandins and leukotrienes, and thromboxanes). Most omega-6s lead to the production of pro-inflammatory compounds (e.g., PGE2 and LT2) and omega-3s to less inflammatory ones (e.g., PGE1, PGE3, and LTB5).
- Omega-3 fats, which are anti-inflammatory, alter gene expression and cell receptor signaling.
- Certain foods have more antioxidant effects. They are less likely to create free radicals, and they are linked to lower C-reactive protein (CRP) levels.
- Maintaining a healthy glycemic index/load keeps CRP levels down.
- A healthy gut microbiome seems to be linked to lower levels of inflammation.
How to Use It
Key recommendations for eating an AID include the following59:
- Keep non-fish animal fat intake low. They contain arachidonic acid, which is pro-inflammatory and increases clotting, vasoconstriction, and vasospasm. Wild sources of meat seem to be better than farm-raised ones. Visible fat should be trimmed off cuts of meat.
- Eat more fish. Tilapia, anchovies, and wild salmon are safe options, whereas fish higher up the food chain, like sharks, swordfish, and golden bass are less ideal because of mercury levels. Aim for 2-3 servings of fatty, cold-water fish weekly.
- Limit omega-6 fats such as corn, soy and vegetable oil. Coconut oil that hasn’t been hydrogenated is probably okay, because it contains a lot of medium-chain fatty acids that the liver readily absorbs. Extra virgin olive oil is a healthy choice.
- Eat more omega-3s. Go for 1-2 grams of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) daily. Omega-3 eggs are an option. 1 gram of fish oil has about 0.5-1 gram of combined omega-3s, so a standard dose of fish oil is 3-4 grams daily. To treat inflammatory conditions, consider 4-5 grams of fish oil daily.
- Keep vegetable and fruit intake high. This is correlated to lower levels of inflammatory markers. Remember that corn and potatoes really don’t count as vegetables.
- Eating whole grains is linked to lower CRP levels.
- Eating dietary fiber slows digestion and can reduce inflammation—go for at least 22 grams daily.
- Eating legumes, 4 servings per week, has been found to reduce CRP.
- Eating 5 or more servings of nuts and seeds weekly also lowers inflammatory markers.
- Eat anti-inflammatory herbs and spices. Examples include turmeric, rosemary, ginger, oregano, clove, cumin, cayenne, ad boswellia.
- Don’t char food, as charring is linked to inflammation (especially meat).
- Pay attention to glycemic load (discussed in the “Glycemic Index” tool).
- Avoid obesity, which is in and of itself an inflammatory state. Even with healthy eating, portion size should be controlled.
- Ensure adequate magnesium intake (6 mg/kg daily) from foods like spinach, peanuts, almonds, quinoa, mackerel, avocados, and brown rice.
The Mediterranean and Okinawan diets are excellent examples of AIDs.
When to Use It
AIDs can be used in any chronic disease where inflammation is a component. Key examples with good associated research include59:
- Coronary heart disease
- Type 2 diabetes
- Rheumatoid arthritis and other autoimmune diseases
- Chronic obstructive pulmonary disease
- Alzheimer’s
- Inflammatory bowel disease
- Allergies and asthma (including eczema)
- Cancer
- Depression (people with severe depression are especially likely to improve)
What to Watch Out for (Harms)
- This diet is quite safe.
- Remind people that inflammation isn’t all bad. We need it, just not chronically and not in excess. The goal is to decrease “meta-inflammation,” the chronic, low grade damaging processes that use the same pathways as acute inflammation. In acute illness, fevers, swelling, and activation of the immune system are important to our health. It is not helpful to completely eliminate omega-6 fats.
- You may be asked to check levels of omega-3 fats. Most clinicians will have people try the diet first and only consider more investigations if it is not effective over time. People need not have an elevated sedimentation rate or C-reactive protein to benefit.
Tips from Your Whole Health Colleagues
- The AID can take a while to be effective. Patients should try it for at least 6 weeks, if not longer.
- The AID is part of an anti-inflammatory lifestyle that includes many different aspects of good self-care. Be sure to complement an AID with other ways to lower inflammation, such as the following:
- Limit alcohol.
- Balance glucose levels, so that there aren’t large insulin spikes (insulin is pro-inflammatory).
- Ensure adequate sleep.
- Keep stress levels low.
- Stay active.
- Maintain a healthy mix of gut microorganisms. This is discussed in the Whole Health tool, “A Healthy Microbiome,” later in this chapter.
- Many people assume they can just eat or supplement with alpha-linolenic acid (ALA), not to be confused with the other ALA, alpha-lipoic acid. ALA is found in flax oil. Less than 1% of it is converted into DHA and EPA, which are needed for the anti-inflammatory effect.
- For vegetarians, there are algae-derived omega-3 supplements available.
 Whole Health Tool: Eliminating Problematic Foods
Whole Health Tool: Eliminating Problematic Foods
What Is It?
Elimination diets (EDs) involve the strategic removal of a specific food or foods from the diet in an attempt to reduce a given set of symptoms.[417] Like drugs, foods can have both helpful and harmful effects. There are a number of different elimination diets in use. An elimination diet is not a formal diet that everyone follows the same way; it is tailored to each individual. Some of them remove one or more food groups (e.g., dairy, gluten-containing foods, or soy). Others are more specific, such as the Low FODMaP diet, which seems to be most helpful for people with irritable bowel syndrome and other functional bowel problems (go to “The Low FODMaP Diet” for more information).
How Elimination Diets Work
A person may develop intolerance to a particular food. This may be tied to a known structural or functional issue, such as lactose intolerance or celiac disease, but it may also be due to other, less clearly defined, mechanisms. Intolerance can involve an IgE-mediated response or an accumulation of eosinophils, or it may be due to IgG, pseudo-allergies, cross-allergies, psychogenic effects, or other mechanisms.
Inflammation of the lining of the gut can be caused by food intolerances, disruptions in the microbiome, and other processes. It is thought to allow for increased permeability in the gut. If larger molecules are able to enter the bloodstream, immune responses and inflammation, with all their secondary effects, can occur.
How to Use Elimination Diets
There are four steps to an elimination diet.
- The Planning Phase. It helps to use a food diary/log to explore the relationship between foods and symptoms. It details which foods are eaten, as well as symptom timing. Comfort foods and highly craved foods are often the very foods that should be removed first. Work with the patient to create a list of potential culprits. Common ones include gluten, dairy, eggs, soy, citrus, fish, peanuts and/or tree nuts, shellfish, and food additives like the sweetener aspartame.
- The Avoidance Phase. People may just choose to eliminate one food or food group, or (with appropriate guidance) they may remove a number of foods at once and then add one food back every so often. How long to eliminate is controversial, but try for at least 10 days, if not for 2-4 weeks. In some cases, people find it can take several days for the symptoms to improve; they may even describe low-level withdrawal symptoms, or a brief worsening of symptoms, after first stopping a food. It is important to avoid even the smallest amount of the food during this time. For example, if they eliminate dairy, have them stay off of all casein and whey-containing foods too. Label reading is key.
- The Challenge Phase. Next, if symptoms decrease, it is important to re-introduce the food to verify whether or not symptoms recur. In essence, this equivalent to doing an “n of 1” trial. If symptoms come back, one can be fairly sure there is a link with eating the food in question. Add the food back in a small quantity at one meal, then in a larger quantity the next one. If multiple foods have been eliminated, and symptoms don’t recur after a day of adding a specific food (or food group) back, it is still recommended to go back off it while the other foods that have been eliminated have also been tested.
- The Long-Term Plan. It is reasonable to stay off the food for 3-6 months. Sometimes people will become tolerant of an eliminated food after a period of time.
When to Use It
The list of potential indications for EDs is huge.[418] Consider it for chronic conditions, where symptoms are fairly frequent and not likely to spontaneously improve on their own. Use it with people who have the financial (and emotional) resources to make shifts in their diet without too much difficulty. Fatigue, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), allergic symptoms, chronic sinusitis, rheumatoid arthritis, ADHD, gout, rheumatoid arthritis, chronic pelvic pain, asthma, autism, gastroesophageal reflux disease (GERD), migraine headaches, and numerous other health conditions often respond well. Consider it with autoimmune problems, arthritis, and pain of unknown cause as well.
What to Watch Out for (Harms)
- Never reintroduce a food that has previously caused an anaphylactic reaction.
- Use caution in people with eating disorders.
- Pay close attention to weight loss and gain.
- Ensure people are keeping their nutrition balanced. Are nutrient needs being met?
- Take care that people don’t overeat other foods to compensate for the groups they have eliminated.
Tips from Your Whole Health Colleagues
- Experience on the part of Integrative Health clinicians is markedly favorable when it comes to EDs.
- Some patients will ask about lab testing for food intolerances. There are a number of private labs that provide these services. Most of them test for Immunoglobulin G (IgG) reactions to particular foods; many also test for IgE. Insurance rarely covers this testing. See the “Testing to Assess the Gastrointestinal Ecosystem” tool for more information.
- Remember that some people may be bothered by more than one food group. If removing one food helps somewhat but not fully, consider elimination of other foods or food groups as well. Some disorders seem to be affected by specific foods. Try dairy elimination for sinusitis. Headaches are often linked to distinct groups of foods as well.
- Combine EDs with approaches to improving microbiome health. The “Healthy Microbiome” tool later in this chapter has more information.
5. Come Up with a List of Favorite Cookbooks, Recipes, and Cooking Websites
The Resources section at the end of this chapter has suggestions regarding cookbooks, recipes and websites that offer guidance around healthy eating, while respecting a person’s budget.
6. Develop a List of Your Favorite Eating Tips for Patients
In addition to following one or more of the guidelines listed above, another option for the Food and Drink portion of a PHP is to choose one specific eating tip with the patient and focus on it for a set period of time. Here is a brief overview of 10 Whole Health Eating Tips. You can cover one or more tip in your time with someone, depending on each patient’s interest and motivation. Remember, many people will be more successful if they make one SMART Goal-based change at a time. The eating tips covered in the rest of this chapter (by no means an all-inclusive list) include13:
- Whole Health Eating Tip #1: Pay Attention to Calories
- Whole Health Eating Tip #2: Be Careful with Eating Out and Eating Fast Food
- Whole Health Eating Tip #3: Eat Vegetables and Fruits
- Whole Health Eating Tip #4: Eat Healthy Carbohydrates
- Whole Health Eating Tip #5: Keep Glycemic Index and Load in Mind
- Whole Health Eating Tip #6: Choose Healthy Fats
- Whole Health Eating Tip #7: Eat Healthy Sources of Protein
- Whole Health Eating Tip #8: Eat Adequate (Not Excessive) Amounts of Nuts
- Whole Health Eating Tip #9: Choose Healthy Beverages
- Whole Health Eating Tip #10: Remember the Context of Each Meal
- Whole Health Eating Tip #11: Eat in a Way that Keeps Your Microbiome Healthy
Whole Health Eating Tip #1: Pay attention to calories
Cutting back on calories to 500 a day below an amount that maintains weight should lead to a weight loss of roughly a pound a week (though exactly how many calories are actually in a pound is actually a subject of some debate). It can be a hassle to do strict calorie counts, but it can help to remind people of how many calories they need daily to maintain their weight. Keep in mind that it is not just the number of calories, but also the form they are in when a person consumes them (i.e., what specific foods they eat). Table 8-1, below, is a simple guide for calculating caloric needs.
A number of websites and phone apps can assist with calorie counting. Check out the Resources section at the end of this chapter for some suggestions. There are diets that encourage people to fast for brief periods (intermittent fasting), and research on intermittent fasting is increasingly favorable.[419] Animal studies indicate intermittent fasting delays aging, improves cognition, changes microbiome and reduces oxidative stress.[420]
Table 8-1. Calculating Caloric Needs by Weight and Activity Level
|
Lifestyle |
To calculate daily calorie needs, Multiply current body weight by this factor |
|
|
Pounds |
Kilograms |
|
|
Confined to bed |
12 |
20 |
|
Sedentary |
13 |
25 |
|
Moderately active |
15 |
30 |
|
Very active |
17 |
30 |
|
Athlete in training |
20 |
40-45 |
|
For example, a moderately active person who weighs 150 pounds would want to eat 150x15= 2,250 calories to maintain body weight. |
||
Whole Health Eating Tip #2: Be Careful with Eating Out and Eating Fast Food
People who eat away from their homes are at much higher risk of eating more calories and unhealthy fats. Overall intake of some nutrients also decreases.[421] Most studies find a link between the intake of ultra-processed foods (the kind that is usually sold in fast food restaurants) and obesity, cholesterol levels, glucose levels, blood pressure, and metabolic syndrome.[422] Talk with patients about how often they eat out. Encourage them to eat more self-prepared meals, if this is possible. Negotiate with them about a maximum number of meals to eat out weekly and discuss healthy options.
Whole Health Eating Tip #3: Eat Vegetables and Fruits
There has been an increased move toward saying “vegetables and fruits” versus the other way around.[423] Vegetable and fruit consumption decreases mortality in general, and it specifically reduces deaths due to cardiovascular disease. A 2014 systematic review found that risk of death from all causes dropped by 5% and 6%, respectively, for each serving of vegetables or fruits a person eats daily.[424] The benefits started to diminish once people reached more than 5 daily servings of fruits and veggies combined. A 2017 meta-analysis/systematic review found that a graded improvement in risk from cardiovascular disease, cancer, and all-cause mortality.[425] Increased vegetable and fruit intake is also linked to reduced cognitive impairment risk[426] and is protective against depression.[427]
Remind people that corn and potatoes are not really vegetables so much as grains/starches. Green leafy vegetables contain multiple nutrients, including indole-3 carbinol, which facilitates removal of cancer-causing chemicals by the liver. Red, orange, and yellow vegetables also contain carotenoids, which have numerous health benefits. Eating a rainbow of colors of foods (let cauliflower be the white food that is eaten, in place of starches) can be a simple way to vary the types of vegetables and fruits one eats.
Whole Health Eating Tip #4: Eat Healthy Carbohydrates
The National Research Council recommends that people eat 45-65% of calories from carbohydrates, keeping added sugars below 25% of calories.[428] There is some debate about the relative proportion of carbohydrates a person should eat. The PURE study, which included over 135,000 people, found that higher carbohydrate intake is associated with an increased mortality risk, but want found to be linked to cardiovascular disease risk or mortality.[429] Encourage patients not to eat too many simple sugars (e.g., processed foods, or foods that are “white” like donuts, plain bagels, and white bread). In plant-based foods, 90-95% of the calories come from carbohydrates. Carbohydrates are absorbed more slowly, and blood glucose levels stay lower if multiple small meals are eaten, rather than just a few large ones.[430]
Fructose. Fructose is a simple sugar found in fruit, honey, and some vegetables. It is closely related to high fructose corn syrup (HFCS), which contains both fructose and sucrose (table sugar). In small quantities, fructose alone can decrease blood sugars.[431] However, most Americans consume 40 grams of fructose a day, mostly as HFCS. This has been linked to metabolic syndrome and increased cardiac risk,[432],[433] as well as salt-sensitive hypertension,[434] and fatty liver disease.[435]
Fiber. Fiber refers to carbohydrates that are eaten but do not break down into sugars the gut can absorb. Most fiber travels all the way through the intestinal tract, serving a number of purposes as it does so. Fiber helps with bowel movements, controls cholesterol levels, prevents insulin resistance (and type 2 diabetes), reduces cardiovascular disease risk, and supports a healthy gut microbiome (the bacteria that live in the gut).13 People with a high fiber intake, compared to those with poor fiber intake, have a 77% lower risk for all-cause mortality.[436] Fiber intake is protective against colon cancer,[437] pancreatic cancer,[438] ovarian cancer,[439] cardiovascular disease,[440] and stroke.[441] The most beneficial fibers are those from cereals and whole foods.
Most American adults eat insufficient fiber (about 15 grams daily) but the Institute of Medicine recommends that women get 25 grams daily, and men 38. Good sources of fiber include[442]:
|
|
|
There are two types of fiber. Soluble fiber is found in many foods, including apples, beans, blueberries, lentils, nuts, oatmeal, pears, peas, psyllium, and strawberries. It helps with cholesterol and blood sugar control. Insoluble fiber helps with diverticular disease and constipation. It is found in couscous, barley, whole grains, brown rice, wheat bran, nuts, seeds, carrots, cucumbers and many of the other foods listed above.
Whole Health Eating Tip # 5: Keep Glycemic Index and Load in Mind13
Rather than getting caught up in whether or not a carbohydrate is simple or complex, it may be best to focus on glycemic index (GI) and glycemic load (GL). These measures take into account how much glucose a food releases into the blood. Glycemic index (GI) compares how much a particular food that contains 50 grams of carbohydrates will raise blood glucose levels 2 hours after eating, relative to an equivalent amount of glucose (or white bread). The problem with the GI is that different foods have different amounts of carbohydrate by weight. For example, in order to get 50 grams of carbohydrates from carrots, you would have to eat at least 5 cups of them. To allow for more realistic comparisons, GL is used instead. GLs account for serving size.[443]
A large 2014 study found that the quintile of patients with the highest food measures of GI and GL had a 33% higher risk of developing the type 2 diabetes.[444] Low-GI diets have been found to be more effected in controlling A1C and fasting blood glucose levels versus higher-GI diets.[445] There is also a correlation between high-GL diet and ischemic stroke risk, obesity, and chronic inflammation.13 A 2019 meta-analysis found that high GI diets correlated with potentially higher risks of certain cancers, including colorectal, bladder, and kidney cancer),[446] and low GI/GL diets lowered gall bladder and coronary artery disease risk.[447] Low GI diets also seem to favorably affect blood pressure.[448] A few recent studies have questioned if these measures are the best for looking at disease risk or outcomes,[449] but it has been found to be useful for many people. Glycemic index/load resources are featured in the Resources section at the end of this chapter and you can also learn more using the “Glycemic Index” tool in the Whole Health Library.
Whole Health Eating Tip #6: Choose Healthy Fats
While this is controversial, some experts suggest that 20-35% of calories should come from fat.71 For years, we were discouraged from eating fat, and the fat-free foods market boomed. Unfortunately, this eating pattern did not help people to sustainably lose weight.[450] The PURE study (a multi-country study of over 135,500 people) surprised many people when it found that “intake of total fat and each type of fat was associated with a lower risk of total mortality.”72 There are several categories of fats that include the following59:
- Saturated fats do not have double bonds. They are solid at room temperature. Examples are butter, coconut oil, and palm oils. While there is discussion that coconut oil might have some unique properties, most saturated fats are best avoided.
- Monounsaturated fats are liquid at room temperature. They are found in olive, canola, and peanut oils, as well as in avocados. They tend to be a healthy choice.
- Trans fats are the unhealthiest fat choice of all. In many countries, they are now banned as food ingredients. They are fats that have been chemically manipulated so that they will have a longer shelf life. Avoid them entirely, if possible. This requires looking at ingredient lists, because a food can contain small amounts of trans fats and manufacturers can still technically be able to round down to “0” for trans fats per serving when they list contents on the food’s label.
- Polyunsaturated fatty acids (PUFAs) are liquid at room temperature. Our bodies cannot synthesize linoleic (omega-6) or linolenic (omega-3) acids, so they must be obtained in the diet by eating dark leafy greens, purslane, or meat from animals that were fed diets rich in PUFAs. Omega-3s are found in deep-sea fish, like salmon and sardines, as well as in walnuts.
Omega-3s are PUFAs that deserve special mention. They are precursors to anti-inflammatory compounds in the body, but they tend to be eaten in less-than-desired quantities in the American diet. Omega-3s are discussed in the “Anti-Inflammatory Diet” Whole Health tool, earlier in this chapter.
Whole Health Eating Tip #7: Eat Healthy Sources of Protein
Roughly 10-35% of calories should come from protein, according to many expert sources.[451] For adults, the recommendation is 0.8 grams of protein per kilogram of body weight. 2 or 3 servings a day is sufficient, but most Americans eat more protein than is necessary (an average of 100 grams daily).94 It is recommended to eat animal proteins in moderation, as meats commonly contain saturated fats, which may have negative health effects. A 2019 trial questioned whether white meat was superior to red for preventing cardiovascular disease.[452] Protein leads to more satiety than carbohydrates or fats. Encourage people to vary their protein sources to get all their essential amino acids. Meats, beans, lentils, rice, grains, egg whites, soy, and mushrooms all contain a good variety. It is often proteins that seem to trigger not only food allergies, but also food intolerances. The “Elimination Diet” Whole Health tool (earlier in this chapter) has more information.
Whole Health Eating Tip #8: Eat Adequate (Not Excessive) Amounts of Nuts
Eating a handful of nuts daily (not a canful, because they are high in calories) has been found to have health benefits in increasing numbers of studies. A 2016 systematic review and meta-analysis concluded that higher nut consumption is associated with lower risk of all-cause mortality, total cardiovascular disease, cardiovascular disease mortality, and sudden cardiac death.[453] Nut consumption also lowered systolic blood pressure, especially eating pistachios.[454] Nut consumption is also linked to lower cancer mortality.[455]
Whole Health Eating Tip #9: Choose Healthy Beverages
21% of our caloric intake comes in the form of beverages.[456] Cutting out soda, sweetened tea or coffee, juice, alcohol, energy drinks, smoothies, and milk—and replacing them with water—can markedly decrease calorie intake. Always ask how much alcohol and caffeine a person consumes as well. Keep in mind that many sweetened beverages contain HFCS, the effects of which are discussed above (Tip #1). More resources related to beverages are listed at the end of this chapter, and in the Whole Health Library clinical tool, “An Introduction to Food and Drink for Whole Health.”
Whole Health Eating Tip #10: Remember the Context of Each Meal
In addition to what a person eats, there are many other factors that are linked to how Food and Drink influence health. Examples include the following:
- Access. Does a person live in a food desert, with limited access to food in general? Do they experience food insecurity? Do they live in a “food swamp,”[457] where there is food available, but most of it is unhealthy?
- Food safety. Does the person eat whole foods, or processed foods? How many pesticides are they taking in when they eat? To learn more, go to the “Food Safety” tool in the Whole Health Library.
- Culture and nutrition. How do a person’s ethnicity, religious beliefs, family of origin, geographical location, or other factors influence their dietary patterns?
- Context of meals. Food psychology has demonstrated that glass size, plate size and color, number of foods offered during a meal, how many people eat together, and even the speed of the slowest eater at the table can influence our eating patterns.[458]
Whole Health Eating Tip #11: Eat in a Way that Keeps Your Microbiome Healthy
Last but not least, do not forget about probiotics and their potential role. What follows is a tool to guide you if you choose to incorporate probiotics into a PHP.
 Whole Health Tool: A Healthy Microbiome: The Role of Probiotics
Whole Health Tool: A Healthy Microbiome: The Role of Probiotics
What Is the Microbiome?
Trillions of microorganisms—mostly bacteria, and over 30,000 different species—live in the human gut.[459],[460] Which ones live there can have a marked effect on health. You can support a healthy microbiome through your diet as well as by taking various dietary supplements.
Probiotics are living organisms that offer benefits to their host. Prebiotics are the food they need to survive, and postbiotics are their metabolic byproducts (which can include vitamins and other nutrients). They are usually identified by their species. Common examples include Lactobacillus acidophilus and Bifidobacterium bovum.
How It Works
New roles for the gut microbiome are being discovered all the time. Some of the roles we know of so far include direct DNA signaling, vitamin production, interacting with the immune system, protecting the gut from attachment of harmful microbes, impeding the growth of harmful organisms, and modulating central nervous system function.
In order to be effective, probiotic foods and supplements should actually contain organisms that can survive exposure to the stomach acid and bile, and they should be able to effectively colonize once they reach the appropriate part of the gastrointestinal (GI) tract.
How to Use Probiotic Foods and Supplements
Nutrition and the Microbiome. Diets high in fiber, vegetables, and fruits are the best at helping the gut keep a healthy mix of microbes. Avoiding red meat and animal fats is also helpful. Common probiotic foods clinicians can encourage patients to eat include yogurt, milk (if not overly pasteurized), kefir, kombucha tea, sauerkraut, miso and tempeh (forms of soy), and pickles. Frozen foods tend not to have viable bacteria.
Probiotic Supplements. Capsules containing beneficial organisms are dosed based on colony forming units (CFUs). These are normally dosed in powers of 10. Standard doses are 1 billion (109) CFUs, or 10 billion (1010) once or twice a day. There are many brands available, and some of them contain specially patented mixtures or species.
Some of the most-researched strains of probiotics include:
- B. bifidum Malyoth strain
- B. longum
- Bifidobacterium lactis BB12 (abbreviated as B. lactis BB12)
- Lactobacillus acidophilus DDS1 (abbreviated as L. acidophilus DDS1)
- L. acidophilus NAS
- L. bulgaricus LB-51
- L. gasseri
- L. plantarum
- Lactobacillus rhamnosus GG (available as the brand Culturelle)
- Saccharomyces boulardii—this is a yeast found to have several benefits. Keep it in mind for recurrent Clostridium difficile (“C. Diff”) colitis and inflammatory bowel disorders.
Have patients take probiotics on an empty stomach, and if they are taking an antibiotic, separate them by two hours. If they are heat-dried, they should be kept in the fridge, but if they are lyophilized, they can be kept at room temperature. It is unclear how long they should be taken, but 2 weeks to 2 months is typical, or longer if people have chronic conditions such as Crohn’s or irritable bowel syndrome (IBS).
When to Use Probiotics102
Antibiotics, bowel preps, proton pump inhibitors, and exposure to pathogens (e.g., viral gastroenteritis) can all alter bowel flora. Many Integrative Health clinicians will use probiotics whenever they prescribe antibiotics or anytime a person has had an infectious gastrointestinal illness. They also seem to reduce inflammation, so they should be considered in any inflammatory process. Other indications include vulvovaginal candidiasis, eczema, IBS, respiratory infections, prevention of traveler’s diarrhea, and augmentation of H. pylori treatment.
What to Watch Out for (Harms)
Probiotics tend to be quite safe. There are a few case reports about them translocating into the bloodstream to cause abscesses, or infecting people with severe immunocompromise. Untested strains should not be used, nor should strains that are usually classed as pathogens. One study found negative outcomes in patients who were given probiotics when they had severe acute pancreatitis.
Tips from Your Whole Health Colleagues
- A number of clinicians report that the probiotic yeast, Saccharomyces boulardii, can also be helpful.
- While more studies are needed, research indicates that the microbiome affects brain function[461] and emotional states.[462] Research into psychobiotics is showing promise.[463],[464] More studies are needed, but a 2019 study found that probiotics have significant therapeutic effects for people with depression.[465]
- There is a connection between gut flora and obesity as well.[466]
- Lactobacilli tend to do more in the upper GI tract. Bifidobacteria are more likely to affect the colon.
- More details are available in the “Promoting a Healthy Microbiome with Food and Probiotics” tool in the Whole Health Library.
Food & Drink Resources
Websites
VA Whole Health and Related Sites
- A Patient Centered Approach To: Food and Drink. Part of the Components of Health and Well-Being Video Series. https://www.youtube.com/watch?v=Xa6-dyaFddo&feature=youtu.be
- Veterans Whole Health Education Handouts. https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
- An Introduction to Food and Drink for Whole Health
- Carbohydrates and Your Health—Glycemic Index, Glycemic Load, and Blood Sugars
- Deciding How to be a Healthier Eater
- Eating to Reduce Inflammation
- Healthy Tips on Eating Out and Grocery Shopping
- Mindful Eating
- How a Healthy Gut Makes for a Healthier You
- Probiotics for Specific Conditions
- How to Eat a Mediterranean Diet
- Using an Elimination Diet to Help Learn if Certain Foods are Making You Sick
- Eating to Reduce Irritable Bowel Symptoms: The FODMaP Diet
- Whole Health Food, Drink, Activity and Symptom Log
- MOVE! Weight Management Program. http://www.move.va.gov.
- Move! Handouts. Feature diet as well as exercise. http://www.move.va.gov/handouts.asp.
- VA Nutrition and Food Services. Has listing of ways nutrition can influence health for a number of different diagnoses. http://www.nutrition.va.gov
- Get Help from a Dietitian. https://www.nutrition.va.gov/Get_Help_from_a_Dietitian.asp
- Recipe and Cookbooks. https://www.nutrition.va.gov/Recipes.asp
- Additional Resources. https://www.nutrition.va.gov/veteranNutritionLinks.asp
- Oncology Cookbook. Patient Education Site, Cancer and Nutrition. http://vaww.nutrition.va.gov/clinicalNutrition/ptEd.asp#cancer_and_nutrition
Whole Health Library Website
- Food and Drink. Overview. https://wholehealth.wisc.edu/overviews/food-drink
- An Introduction to Food and Drink for Whole Health. va.gov/WHOLEHEALTH/veteran-handouts/docs/IntroFoodDrink-508Final-9-4-2018.pdf Choosing A Diet. https://wholehealth.wisc.edu/tools/choosing-a-diet
- Food Safety. https://wholehealth.wisc.edu/tools/food-safety
- Mindful Eating: Enhancing Your Relationship with Your Food. https://www.va.gov/WHOLEHEALTHLIBRARY/tools/mindful-eating.asp
- Promoting a Healthy Microbiome with Food and Probiotics. https://wholehealth.wisc.edu/tools/promoting-healthy-microbiome-with-food-probiotics
- When Your Food & Drinks Could Be Causing You Problems: Elimination Diets. https://www.va.gov/WHOLEHEALTH/Veteran-Handouts/docs/EliminationDiets-Final508-03-25-2019.pdf
- The Low FODMaP Diet. https://wholehealth.wisc.edu/tools/fodmap-diet
- Achieving a Healthy Weight. https://wholehealth.wisc.edu/tools/achieving-healthy-weight
- Glycemic Index. https://wholehealth.wisc.edu/tools/glycemic-index
- Understanding Sweeteners. https://wholehealth.wisc.edu/tools/understanding-sweeteners
- The DASH Diet. https://wholehealth.wisc.edu/tools/dash-diet
- Testing to Assess the Gastrointestinal Ecosystem. https://wholehealth.wisc.edu/tools/testing-to-assess-the-gastrointestinal-ecosystem/
- Personal Health Plan Template. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/08/Brief-Personal-Health-Plan-Template.pdf
- Whole Health for Skill Building: Food & Drink. https://wholehealth.wisc.edu/courses/whole-health-skill-building/
- Faculty Guide
- Veteran Handout
- PowerPoints
- Mindful Awareness Script: Mindful Eating
- Eating for Whole Health: Nutrition for all Clinicians. https://wholehealth.wisc.edu/courses/eating-for-whole-health/
- Course manual
- PowerPoints
- One-week menu with recipes
- List of resources from course faculty.
Other Websites
- Anti-Inflammatory Diet and Pyramid. Dr. Andrew Weil website. http://www.drweil.com/diet-nutrition/anti-inflammatory-diet-pyramid/
- Dietary Guidelines for Americans 2015-2020. https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/
- FoodData Central. USDA Agricultural Research Service. Search for the contents of various nutrients, including fiber, in any given food. You can do a “Food Search” to see the nutrients in a particular food. https://fdc.nal.usda.gov/
- Food Access Research Atlas. USDA Economic Research Service. Shows urban and rural food deserts on an interactive map. https://www.ers.usda.gov/data-products/food-access-research-atlas/go-to-the-atlas.aspx
- Local Harvest. Search out CSAs in your area or order fresh foods from around the country. http://www.localharvest.org/
- Nutrition and Healthy Eating. Mayo Clinic. http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/basics/nutrition-basics/hlv-20049477
- Oldways Cultural Food Traditions. Guidance on eating within various traditions (e.g., African, Latin American, Asian, Mediterranean, Vegetarian/Vegan styles of eating). https://www.oldwayspt.org.
- The Center for Mindful Eating. Where Mindful Awareness meets Food and Drink. http://thecenterformindfuleating.org.
- The Nutrition Source. Harvard School of Public Health. https://www.hsph.harvard.edu/nutritionsource/
- USProbiotics. California Dairy Research Foundation and Mary Ellen Sanders PhD. Information provides a nice summary of research. http://cdrf.org/home/checkoff-investments/usprobiotics/
- Recipe sites (Note that these are all .com sites. The VA Nutrition and Food Services above features a number of government-approved recipes.)
- Epicurious. http://www.epicurious.com
- My Recipes. http://www.myrecipes.com
- Cooking Light Magazine. http://www.cookinglight.com 101 Cookbooks. Natural foods recipes. http://www.101cookbooks.com
- Sparkpeople. Free registration allows access to a calorie counter and fitness programs. http://www.sparkpeople.com
Books
- Integrative Medicine, 4th edition, David Rakel (2017). Available through VA library system. Includes chapters on food elimination, anti-inflammatory eating, DASH, FODMaP, and prescribing probiotics.
- Eat, Drink, and Be Healthy: The Harvard Medical School Guide to Healthy Eating, Walter Willett (2005)
- Eating Well for Optimum Health: The Essential Guide to Bringing Health and Pleasure Back to Eating, Andrew Weil (2001)
- Good and Cheap: Eat Well on $4/Day, Leanne Brown (2014)
- In Defense of Food: An Eater’s Manifesto, Michael Pollan (2009)
- Mindful Eating: A Guide to Rediscovering a Healthy and Joyful Relationship with Food, Jan Bays (2009)
- Mindless Eating: Why We Eat More Than We Think, Brian Wansink (2007)
- Nutrition in Clinical Practice, 2nd edition, David Katz (2014)
- Passionate Vegetarian, Crescent Dragonwagon (2002)
- The Low Glycemic Index Handbook, Jennie Brand-Miller (2010)
- The New Mediterranean Diet Cookbook, Nancy Jenkins (2008)
- The New Vegetarian Cooking for Everyone, Deborah Madison (2014)
- The Omnivore’s Dilemma: A Natural History of Four Meals, Michael Pollan (2007)
- What I Eat: Around the World in 80 Diets, Peter Menzel (2010)
- Wheat Belly: Lose the Wheat, Lose the Weight, and Find Your Path Back to Health, William Davis (2014). Many patients are reading books like this and have questions about their content.
Apps and Monitoring Software
The phone app listed below is free. Find it by searching online or in your device’s app store.
- MOVE! Coach
Special thanks to Samantha Sharp, MD, who wrote the original Whole Health Library materials on Food and Drink that inspired content for much of this chapter, as well as Sagar Shah, MD, who updated the library materials in 2018, and the entire Eating for Whole Health faculty team, who updated the materials again in 2020. Also, gratitude to the VA dietitians and other Nutrition and Food Service leaders who have offered feedback regarding content.



















