Office of Health Equity
American Indians/Alaskan Natives Veterans Colorectal Cancer Screening
American Indians/Alaskan Natives Veterans Colorectal Cancer Screening Lauren Korshak, DHealth(c), MS, RCEP, Office of Health Equity
|
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially and ethnically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA healthcare mission. The Office of Health Equity (OHE) champions the elimination of health disparities and achieving health equity for all Veterans.
The Office of Health Equity-QUERI Partnered Evaluation Center examines and evaluates health outcomes and healthcare quality across the entire VA healthcare system paying special attention to whether gender, geographical location, or individuals that are members of minority population groups experience disparities in care.
American Indians and Alaska Natives (AI/AN) serve in the U.S. Armed Services at a higher rate than any other group. Almost three-quarters (74.3%) of American Indian/Alaska Natives who are service-connected utilize VA health care.
COLORECTAL CANCER SCREENING HEALTH DISPARITIES
Colorectal, or colon, cancer (CRC) is cancer that is found in either the colon or the rectum. CRC is the third most common cancer in men and women and the second most common cause of cancer-related mortality. Death rates of AI/AN patients with CRC are significantly higher compared to white patients. However, early detection and prevention through screening reduces the risk of CRC-related poor health outcomes.
VA achieves CRC screening rates that surpass the national benchmark of 80%. While most minority Veteran groups have similar screening rates as white Veterans, rates for AI/AN were 6.2% lower than rates in Whites. More impressively, the odds of being up-to-date with CRC screening among AI/AN Veterans is 23% lower than whites in analyses that control for other factors.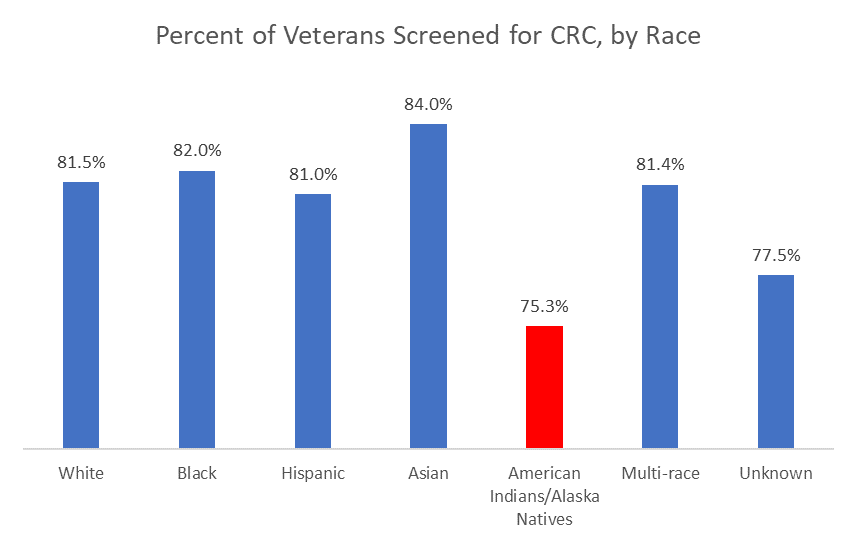
QUALITY OF CARE
There are many types of screening procedures for colorectal cancer. The two most common are:
1. A colonoscopy allows physicians to visually inspect the interior walls of the rectum and the entire colon using a thin, flexible, lighted tube called a colonoscope2. A fecal immunochemical test, which detects blood that is not visible in a stool sample.
The fecal immunochemical test (FIT) is less expensive and perhaps more convenient for patients than other CRC screening methods. This test may be especially important for AI/AN Veterans because they are much more likely to reside in rural and highly rural settings far away from large VA Medical Centers than other Veteran groups.
To complete a FIT, the patient places a small sample of their stool into a small tube. The tube is then sent to a medical laboratory. If the FIT is positive for blood, the Veteran’s health care provider follows up with a prompt diagnostic evaluation—usually through a colonoscopy—and connects the Veteran to the care they need.
High CRC screening rates in VA can be attributed to many system-level factors, including the implementation of the patient-centered medical home model to enhance the delivery of primary care to Veterans and a system-wide emphasis on CRC screening through the national VA Colorectal Cancer Care Collaborative.
Patient-centered medical homes (PCMHs) are used by the VA to deliver primary care through an integrated, team-based approach that can be particularly helpful in managing care and addressing social determinants of health and can continue to help addressing disparities in access to important screenings for conditions like CRC.
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
REFERENCES
May, F. P., et al. 2019. “Race, Poverty, and Mental Health Drive Colorectal Cancer Screening Disparities in the Veterans Health Administration.” Medical Care; 57(10): 773-780. [PMID: 31415338]
Office of Research & Development “VA meeting goals for colorectal cancer screening,” https://www.research.va.gov/news/features/colorectal_cancer.cfm
Alshareef, S. H., et al. 2019. “Association between Race and Cancer-Related Mortality among Patients with Colorectal Cancer in the United States: A Retrospective Cohort Study.” Int. J. Environ. Res. Public Health 2019, 16(2), 240 [PMCID: PMC6352187]



















