Depression Complicating Diabetes Among Veterans
Depression Complicating Diabetes Among Veterans Jessly Joy, MPH(c), Health Equity Fellow, Office of Health Equity
|
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA healthcare mission. The Office of Health Equity (OHE) champions the elimination of health disparities and ensuring that no Veteran is left behind.
The OHE-QUERI Partnered Evaluation Center examines and evaluates health outcomes and healthcare quality across the entire VA healthcare system, paying special attention to whether gender, geographical location, or individuals that are members of minority population groups experience disparities in care.
In people with diabetes and depression, up to half of them may not receive treatment for their depression symptoms. Depression often makes it hard to self-manage chronic health conditions. Therefore, it is important that both these conditions are addressed and treated by an individual’s health care providers to ensure that they remain healthy.
HEALTH DISPARITIES
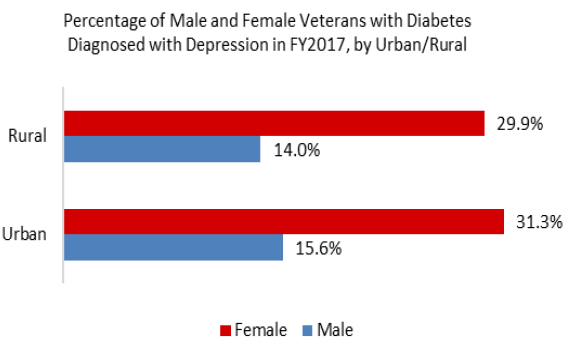
There are, over 1.4 million Veterans with diabetes receiving care through the VA. Of these Veterans, 15.6% are also diagnosed with depression and there are disparities in which groups have both these conditions.
Female Veterans with diabetes are twice as likely to be also diagnosed with depression than male Veterans with diabetes. Additionally, Veterans with diabetes who live in urban areas are more likely to also have depression than Veterans living in rural areas. Therefore, improving health outcomes in these special Veteran groups may require uniquely tailored initiatives customized to the specific needs of these Veteran populations.
REDUCING DISPARITIES
The Office of Health Equity supports research interventions at local VA Medical Centers to reduce health disparities in Veteran groups that are at higher risk for poor health outcomes.
The Healthy Outcomes Through Patient Empowerment (HOPE) intervention is based out of the Veterans Healthcare System that serves Southeast Texas. HOPE explored the impact collaborative goal setting delivered through telehealth may have on Veterans with uncontrolled diabetes and depression. Utilizing telehealth ensured that participants could access the goal setting sessions with their health care providers by reducing transportation barriers for Veterans participating.
Collaborative goal setting can help empower people to take an active role in their health and improve health outcomes. Collaborative goal setting is a process where individuals identify what matters most to them. They then they work with their health care providers to develop health goals based on these values and the best course of treatment and self-care practices to achieve these individual goals.
Veterans who participated in HOPE received nine 1:1 telephone-based coaching appointments with a health care provider over 6 months. Compared to Veterans who didn’t receive the coaching sessions, Veterans who participated in collaborative goal setting had a significant improvement in their depression symptoms. They also had a small improvement in their hemoglobin A1c, a lab value that represents long term diabetes control. Although, since it was a small improvement, it might take longer to improve diabetes outcomes than depression symptoms.
These improvements in depression symptoms can also impact other health conditions and may, over time, result in greater improvements in diabetes and other chronic health conditions. The HOPE Intervention showed that when Veterans can work closely with their health care providers towards health care goals that they identify as important to them, Veterans can be empowered to be healthier versions of themselves.
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
For additional OHE information briefs and fact sheets visit: https://www.va.gov/HEALTHEQUITY/Publications_and_Research.asp
REFERENCES
Naik A.D., et al. 2019. “Effect of Telephone-Delivered Collaborative Goal Setting and Behavioral Activation vs Enhanced Usual Care for Depression Among Adults With Uncontrolled Diabetes: A Randomized Clinical Trial.” JAMA Network Open. [PMCID: PMC6686779]