Office of Health Equity
Differences in Cardiovascular Mortality and Home-Based Cardiac Rehabilitation
Differences in Cardiovascular Disease Mortality & Home-Based Cardiac RehabilitationLauren Korshak, DHealth(c), MS, RCEP, Office of Health Equity, Michelle Wong, PhD, Greater Los Angeles VA Medical Center, Arash Harzand, MD Atlanta VA Healthcare System, Amit Shah, MD, MSCR, Atlanta VA Healthcare System, Cate Parrish, MS, ACSM-CEP, Atlanta VA Healthcare System, Phyllis Wright, DNP, AGPCNP Atlanta VA Healthcare System, Donna L. Washington, MD, MPH, Health Equity-QUERI National Partnered Evaluation Center |
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially and ethnically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA healthcare mission. The Office of Health Equity (OHE) champions the elimination of health disparities and achieving health equity for all Veterans.
Heart disease is one of the leading causes of death in the U.S. overall, and among Veterans who use VA health care. Cardiac rehabilitation can help people with heart disease remain healthy. Home-based cardiac rehabilitation provides people with the opportunity to access these services without experiencing barriers secondary to transportation and availability of programs in their community.
HEALTH DISPARITIES
VA healthcare users have higher rates than non-Veterans of cardiovascular risk factors such as diabetes and hypertension, and among both Veterans and non-Veterans, racial/ethnic minority group members have higher rates of these risk factors than White non-Hispanic groups. Notably, more non-Hispanic Black Veterans who receive care at the VHA die from cardiovascular disease than White Veterans after accounting for differences in age and sex between non-Hispanic Black and White Veteran populations. People who have high blood pressure, unhealthy cholesterol levels, or diabetes are at a higher risk for developing cardiovascular disease. Additionally, not getting enough physical activity, smoking, and eating an unhealthy diet are also risk factors for cardiovascular disease.
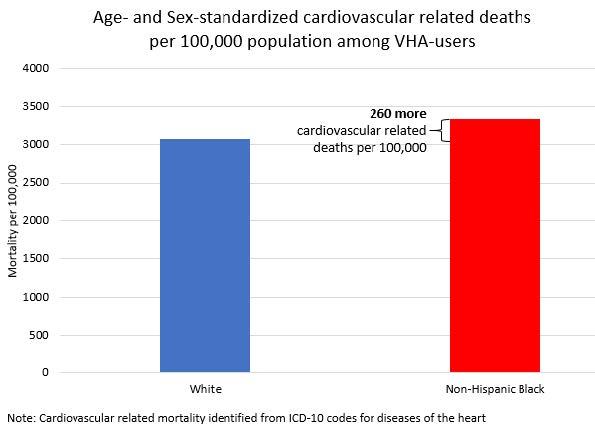
From: Wong MS, et.al. Racial/ethnic disparities in mortality across the Veterans Health Administration. Health Equity. 2019 Apr 8;3(1):99-108. doi.org/10.1089/heq.2018.0086
REDUCING DISPARITIES: HOME-BASED CARDIAC REHABILITATION
The Office of Health Equity supports efforts across VA working to reduce health disparities by targeting interventions aimed at Veteran groups at higher risk for poor health outcomes.
Cardiac rehabilitation (CR) is recommended for individuals who have coronary heart disease (CHD) because it reduces the risk of cardiovascular death and hospital readmission a heart attack. However, despite its lifesaving benefits, less than 10% of eligible Veterans enroll in the cardiac rehabilitation program at their local VA Medical Center (VAMC). Often this is because not all VAMCs have programs so Veterans may have to travel long distances to their nearest program and there can be significant costs associated with this travel from paying for gas, tolls, and other associated costs.
Home-based CR has been proposed as a safe and effective alternative to center-based programs for low to moderate risk Veterans with heart disease. The program at the Atlanta VAMC utilizes remote monitoring and follow up by physician assistants, a nurse practitioner, and a clinical exercise physiologist to ensure that Veterans achieve improved health characteristics through guided lifestyle change programming. Each Veteran’s program is tailored to their individual risks, resources, and health goals. Veterans undergo a detailed initial assessment prior to beginning exercise and other lifestyle change programming after their cardiac event. Their provider carefully coaches them each week for 12 weeks with telehealth calls that consist of education, motivational interviewing, social support, and health tracking to help to veteran become the healthiest version of themselves.
So far 438 Veterans have enrolled in the home-based cardiac rehabilitation program offered at the Atlanta VAMC and 43% of them are African Americans; in addition, 11% are rural and 7% did not graduate high school. Veterans have reported improved exercise capacity, improved blood pressure control and had similar outcomes to Veterans who have participated in cardiac rehabilitation programs that required travel to the VAMC three times a week.

For more information about the Office of Health Equity visit: https://www.va.gov/healthequity.
REFERENCES:
Harzand, A., et al. 2018. Feasibility of a smartphone-enabled cardiac rehabilitation program in male Veterans with previous evidence of coronary heart disease. The American Journal of Cardiology, 122(9): 1471-1476.



















