Hepatitis C Treatment in Minority Veterans
Hepatitis C Treatment
|
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially and ethnically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA health care mission. The Office of Health Equity (OHE) champions the elimination of health disparities, connecting all eligible Veterans to Hepatitis C treatment, to achieve health equity for all Veterans.
ELIMINATING DISPARITIES
Hepatitis C virus (HCV) is four times more common in Veterans than the general U.S. population. Treating HCV can prevent liver cancer, cirrhosis and end stage liver disease.
VA has treated more than 123, 000 Veterans and cured more than 105,000 Veterans with HCV. VA and continues to make testing, treating, and curing HCV infection a priority. The hepatitis C test is available for all Veterans enrolled in VA health care. The newest treatments can cure most patients in about 8-12 weeks. There are no injections with the new treatments, only once daily oral medications.
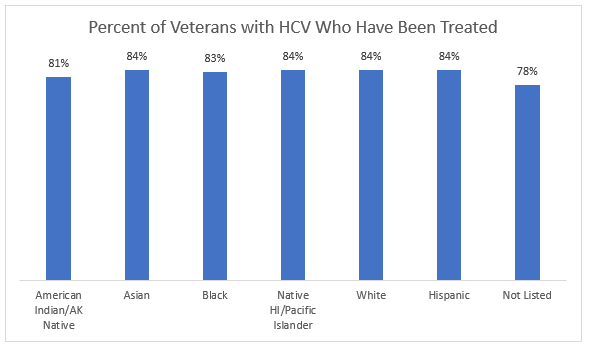
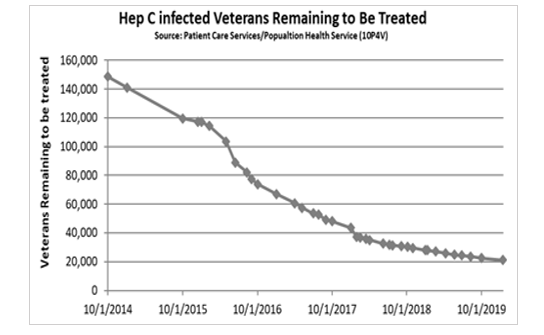
VA began using these potent medications shortly after they became available in 2014 and under the leadership of the HIV, Hepatitis and Related Conditions (HHRC) Program, quickly implemented a collaborative program to identify and treat Veterans with HCV who were both willing and able to be treated. The program included extensive outreach to Veterans in VA known to have HCV infection, and increased testing of those at highest risk for HCV. VA has been continuously tracking HCV treatment among Veterans and no disparities have been identified in the Veterans treated for HCV (Figure 1).
ENSURING UNIFORM ACCESS TO HCV TREATMENT
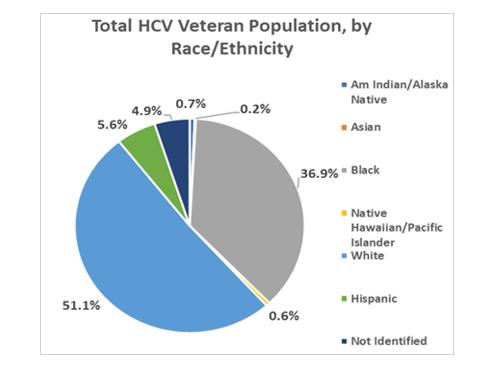
The proportion of those treated by race is essentially identical to the proportion that each race contributes to the total HCV population. No race/ethnicity is being treated at a higher rate relative to the baseline population (Figure 2).
Although not every Veteran with HCV has been treated, there are no disparities with this cohort either. Currently, fewer than 22,000 Veterans in VA care remain to be treated (Figure 3).
Key actions advancing the VA's aggressive treatment of HCV infection include expansion of treatment capacity using nonphysician providers, video telehealth, and electronic technologies; expansion of integrated care to address psychiatric and substance use comorbidities; and electronic data tools for patient tracking and outreach. A critical component of effective implementation has been building infrastructure through the creation of regional multidisciplinary HCV Innovation Teams, whose system redesign efforts have produced innovative HCV practice models addressing gaps in care while providing more efficient and effective HCV management for the populations they serve.
For more information about VA's Hepatitis C treatment efforts visit: https://www.hepatitis.va.gov/
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
For additional OHE information briefs and fact sheets visit: https://www.va.gov/HEALTHEQUITY/Publications_and_Research.asp
REFERENCE
Belperio, P.S., et al. 2017. “Curing Hepatitis C Virus Infection: Best Practices From the U.S. Department of Veterans Affairs” Annals of Internal Medicine. 167(7): 499-504. [PMID: 28973196]