Kidney Disease in Veterans
|
 |
Download PDF
INTRODUCTION
The Office of Health Equity-QUERI Partnered Evaluation Center examines and evaluates health outcomes and healthcare quality across the entire VA healthcare system paying special attention to whether gender, geographical location, or individuals that are members of minority population groups experience disparities in care.
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially and ethnically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA healthcare mission. The Office of Health Equity (OHE) champions the elimination of health disparities, including addressing social determinants of health, such as employment status, to achieve health equity for all Veterans.
KIDNEY DISEASE DISPARITIES
There are age, sex, and race/ethnicity differences in the diagnosed prevalence of chronic kidney disease (CKD) in Veterans. Overall, 7.7% of Veterans are diagnosed with chronic kidney disease over the course of the year. Rates of CKD increases with age. Also, more male Veterans (8.2%) have CKD than female Veterans (2.7%).
After accounting for age and sex, there are statistically significant racial/ethnicity disparities in the percentage of Veterans with diagnosed CKD compared to White Veterans. African American Veterans have the highest rates of CKD (12.7%) followed by Native Hawaiian/Pacific Islanders (10.1%).
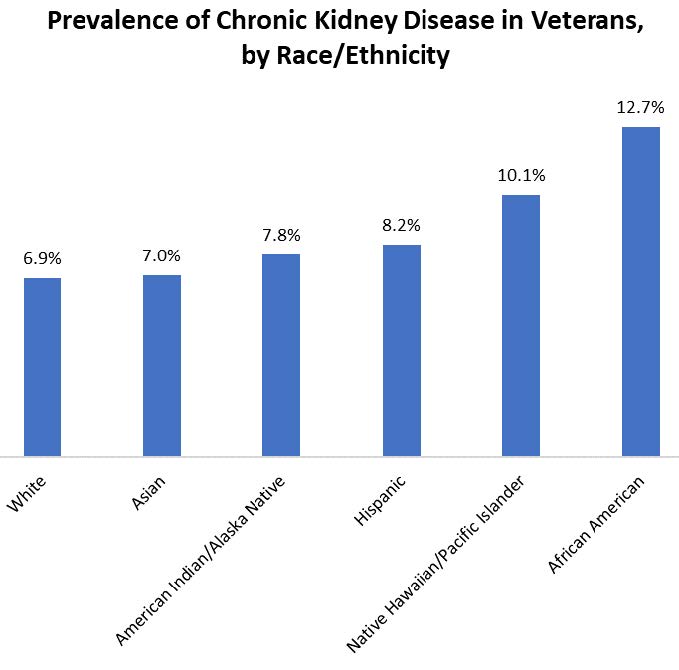
*Data includes all VHA users, adjusted for age and sex
REDUCING RISK OF KIDNEY DISEASE
The Office of Health Equity supports national and local efforts by VA to help reduce the risk of Veterans developing chronic diseases, like kidney disease. Researchers at the Washington, DC VA Medical Center are working to determine if a Veteran’s fitness level impacted their risk of developing kidney disease.
They identified almost 10,000 Veterans who had type 2 diabetes or high blood pressure - both conditions are risk factors for developing chronic kidney disease - and received care at the Washington, DC VA Medical Center or the Palo Alto VA Medical Center in California. These Veterans underwent a treadmill exercise test to determine their peak exercise capacity. Researchers then determined if, over the last 12 years, any of these Veterans received a diagnosis of chronic kidney disease.

They found that the higher a Veteran’s fitness level, the lower their risk of developing chronic kidney disease, even if they already had high blood pressure or type 2 diabetes. In fact, being considered high fit resulted in an 80% reduced risk of developing chronic kidney disease.
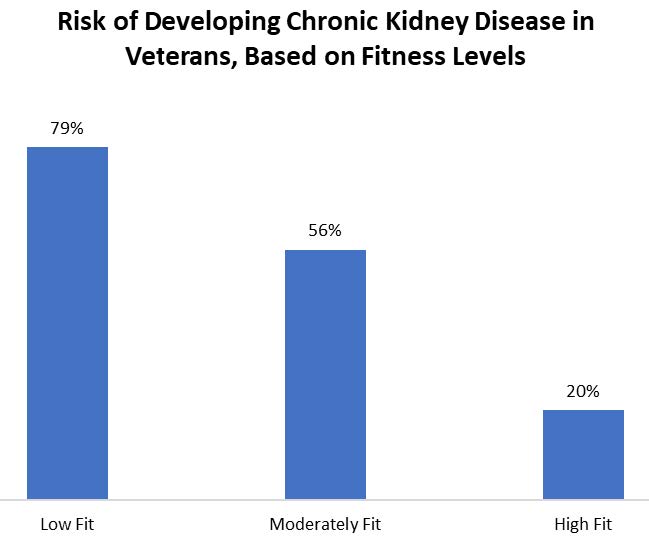
Exercise guidelines recommend engaging in 150 minutes per week, or 30 minutes per day, 5 days per week of a physical activity that feels moderately hard, like brisk walking, biking, or jogging. Through the work of these researchers, there is now evidence showing that by being physically active, Veterans can also protect their kidneys.
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
For additional OHE information briefs and fact sheets visit: https://www.va.gov/HEALTHEQUITY/Publications_and_Research.asp
REFERENCE
Powell, J., et al. “Chronic Kidney Disease Incidence and Cardiorespiratory Fitness Association in Patients with Type 2 Diabetes or Hypertension.” Submitted for Review.



















