Women Veterans and Pregnancy Complications
Women Veterans & Pregnancy ComplicationsCodie Kesler, MPH(c), Office of Health Equity, Lauren Korshak, DHealth(c), MS, RCEP, Office of Health Equity, Jodie G. Katon, PhD, MS VA Puget Sound Health Care System, Amanda Johnson, MD, Office of Reproductive Health Services |
 |
Download PDF
INTRODUCTION
The Veterans Health Administration (VHA) serves a Veteran population that is increasingly racially and ethnically diverse. Equitable access to high-quality care for all Veterans is a major tenet of the VA healthcare mission. The Office of Health Equity (OHE) champions the elimination of health disparities and achieving health equity for all Veterans.
There are 1.9 million women Veterans; making up, 9.4% of the Veteran population. Approximately one quarter (26.4%) of all women Veterans are racial/ethnic minorities.
VETERAN PREGNANCY DISPARITIES
Demand for VA maternity care continues to increase. The number of deliveries that VA paid for has increased 14-fold since 2000. Approximately 4,000 women Veterans are now delivering babies using their VA maternity benefits each year. Maternity Care includes preconception, prenatal, labor and delivery, and postpartum care. Contraceptive use amongst women Veterans is similar to that of non-Veterans. While, the overall rates of pregnancy are lower in women Veterans than in the general population (26.1 versus 34.4 per 1,000), the rates of an unplanned pregnancy in women Veterans is similar to women in the general population (37% compared to 35.2%).
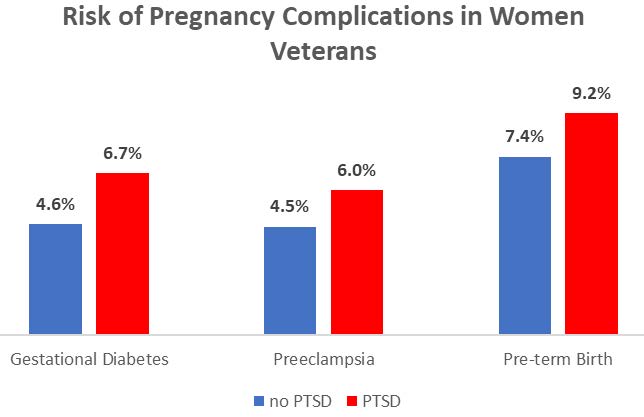
Women Veterans who receive maternity care through VA often have multiple medical conditions that can increase their risk of pregnancy complications. Unique to Veterans, experiencing a military deployment may increase the risk of pre-term birth. It is suggested that one of the reasons for this increased risk of pre-term birth may be that being deployed also increases the risk of developing post traumatic stress disorder (PTSD). Having PTSD can increase the risk of a spontaneous pre-term birth as well as preeclampsia and gestational diabetes.
REDUCING DISPARITIES AND IMPROVING ACCESS TO CARE
The Office of Health Equity supports national and local efforts by VA to reduce health disparities and increase access to services among Women Veterans.
VA MATERNITY CARE
VA is supportive of women Veterans deciding when motherhood is right for them. Maternity care coordination programs are associated with increased utilization of beneficial health services, improved maternal and birth outcomes, and decreased costs, especially for women with chronic or pregnancy-related physical or mental health conditions or social vulnerabilities.
VA offers a full range of services for women Veterans to support their reproductive goals, including providing Maternity Care Coordinators (MCC) for those women Veterans looking to start or expand their family. MCC understand women Veteran's needs and can help them navigate health care services inside and outside of VA throughout pregnancy to ensure timely and continuous care. MCC responsibilities include tracking and coordinating care for pregnant Veterans using VA maternity care benefits as well as acting as a liaison between the patient and VA and community providers caring for her. In addition, the MCC acts as a specialized care manager for pregnant Veterans, assessing pregnant veterans’ needs, supporting self-management, and linking the veteran to needed resources.
In 2015, the MCC program served 957 pregnant Veterans across the 11 VA healthcare systems in which the MCC program was implemented. 2,748 calls to pregnant Veterans were completed and over the course of a pregnancy, MCCs spent on average 150 minutes per Veteran implementing the program. Women Veterans deserve the best care anywhere. The MCC program at VA ensures that pregnant Veterans receive the care and services they need to have a healthy pregnancy.

For more information on maternity care services provided through VA, click here.
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
For more information about the Office of Health Equity visit: https://www.va.gov/healthequity/
REFERENCES
Katon, J. Reproductive Health of Women Veterans:A Systematic Review of the Literature from 2008 to 2017. Semin Reprod Med 2018;36:315–322
Cordasco, K., et al. Care coordination for pregnant veterans: VA's Maternity Care Coordinator Telephone Care Program. Transl Behav Med 2018 May 23;8(3):419-428
Women’s Health Evaluation Initiative (WHEI), Center for Innovation to Implementation (Ci2i) VA Palo Alto Health Care System and Women’s Health Services Office of Patient Care Services Veterans Health Administration. 2018. Sourcebook: Women Veterans in the Veterans Health Administration; Volume 4: Longitudinal Trends in Sociodemographics, Utilization, Health Profile, and Geographic Distribution



















