Passport to Whole Health: Chapter 12
Chapter 12. Power of the Mind: Relaxing & Healing

Peace.
It does not mean to be in a place where there is
no noise, trouble, or hard work.
It means to be in the midst of those things
and still be calm in your heart.
―Unknown
Importance of the Power of the Mind
Some people have problems that are labeled as “incurable.” Some injuries—physical, emotional, mental—cannot be undone or reversed. We cannot regrow a lost limb, or make it so that a traumatic brain injury never happened. We cannot make it so that bad past experiences never occurred. Most of the time, we cannot truly get rid of chronic diseases, either. However—and this is crucial—even if people are so sick as to be terminally ill, it is still possible for them to heal. They can be resilient, and they can move toward wholeness even with their diseases and disabilities. They can learn to cope with pain and move toward greater peace and joy, despite all that might be “wrong” or “broken.” The Power of the Mind helps to make that possible.[681]
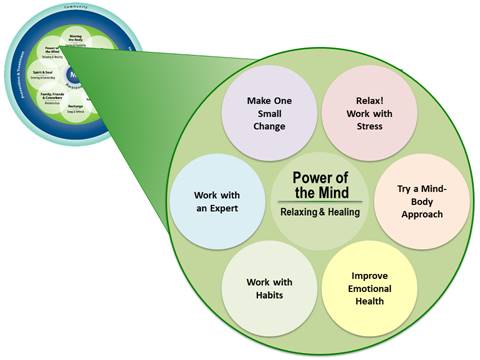
Figure 12-1 highlights some “subtopics” that could be covered when incorporating Power of the Mind into a Personal Health Plan (PHP). These subtopics were developed to encourage Veterans to think about a variety of options and help them zero in on ones that could be used for their PHP. There is a “Make One Small Change” circle that leaves room for creativity, if Veterans do not see an option that interests them. Note that there is also a circle that relates to asking for professional support. This chapter explores these options in more detail.
Historical Perspectives
The healing traditions of China and India have viewed the mind and body as an integrated whole for millennia, but only in recent decades has the mind-body relationship been the focus of Western medical research. The Cartesian concept of mind-body dualism treated the physical body as separate from mind and emotions. Only now are the two being reconnected in Western medicine, as research teaches us more about the complex interrelationship of the mental and the physical. Rather than trying to focus on the “physical” or the “mental,” we are learning that perhaps it is best to focus attention on the whole person. After all, Whole Health is the goal.
Understanding of the Power of the Mind has slowly advanced in the West in the past few centuries.
- In the late 1800s people began to appreciate that one’s mental life can have a significant impact on physical health. With the help of Freud, Jung, and others, Psychology was born.
- In the 1940s, Henry Beecher found that saline injections reduced pain for wounded soldiers, and he coined the term “placebo effect.” We are only just beginning to understand how placebos can reduce pain, improve sleep, improve depression, and help with diagnoses like irritable bowel syndrome (IBS), asthma, heart problems, and headaches.1 Even giving someone a placebo and telling them it is a placebo in advance still works in many studies.[682] For example, a 2016 study of 97 people with chronic low back pain found that they had an average of 1.5 points of improvement in their pain rating on a 10 point pain rating scale (versus 0.2 in controls) after being given an open-label placebo for three weeks. Knowing they were getting a “sugar pill” did not stop the power of their minds from allowing for healing to occur.[683] Disability ratings also markedly improved. The bottom line is that we know that perceptions and beliefs have a powerful effect on health.
- In the 1970s, Herbert Benson began to study what he described as the “relaxation response,” the body’s natural state of relaxation.[684] As it happens, eliciting the relaxation response is what most mind-body approaches have in common.
- Psychoneuroimmunology (or psychoneuroendocrinology) looks at the relationship between our nervous system, our immune system, and our endocrine systems.[685] We are discovering new ways thoughts and emotions have biochemical effects.[686] When we think or feel emotion, our body chemistry changes. We know that inflammation has an important role in depression and fatigue related to chronic disorders; in fact, among other things, antidepressants decrease inflammation.[687]
- Neuroplasticity research has taught us that the nervous system can change in response to the environment, our behaviors, and the natural world.[688] Once considered to be static, our brains are now understood to be undergoing constant changes. For example, parts of the brain can shrink in response to chronic pain (gray matter is lost),[689] and they can also regrow with the use of mind-body techniques like meditation[690] and Cognitive Behavioral Therapy (CBT).[691] Aerobic exercise influences the neuroplasticity of the motor cortex,[692] and calorie restriction and certain dietary approaches can prevent Alzheimer’s disease[693].
- Epigenetics has taught us that our genetic expression changes in response to our environment. Study participants who use mind-body practices experience genetic and molecular changes that are not experienced by people in control groups.[694] Avoiding or preventing adverse childhood experiences can help prevent a large number of future health problems, and avoiding socioeconomic deprivation is also hugely beneficial.[695],[696]
Ten Key Mind-Body Approaches
With greater understanding of the Power of the Mind has come the development of techniques that use the mind-body connection to enhance health and well-being. This chapter introduces a number of these approaches, describing what they are and what we know so far from the research about their safety and efficacy. For the purposes of personal health planning, there are several useful key mind-body approaches to know about. These include the following:
- Psychotherapies (This chapter highlights several that are popular in the VA.)
- Autogenic Training
- Breathing Exercises
- Creative Arts Therapies (These include music therapy, visual arts therapy, and dance therapy, among others.)
- Journaling (and other forms of therapeutic disclosure)
- Progressive Muscle Relaxation and Progressive Relaxation
- Biofeedback
- Guided Imagery
- Clinical Hypnosis
- Meditation
Note that all of these techniques—these tools for your practice—share some common characteristics. Many of them can be introduced as part of a routine office visit or hospital stay. Many of them make use of the power of the relaxation response; if a person can move out of sympathetic activation (fight or flight mode), their physiology and emotional state change. Heart rate and blood pressure decrease, brain waves change, and stress hormone levels go down.[697] A simple way to put it is that all of these approaches reduce stress, which matters a great deal, since stress can contribute to any number of health conditions.
In general, all of these techniques can be beneficial in that they give patients more control over improving their health and they tend to be cost-effective. They can be more effective for managing chronic conditions, they are effective approaches for mental health challenges, and they can foster resilience and enhance wellness.[698] Generally, mind-body approaches can be helpful for heart disease, headaches, low back pain, chronic pain in general, and cancer-related symptoms, as well as postoperative outcomes, hypertension, arthritis, insomnia, incontinence, cognitive impairment, substance use disorders, and posttraumatic stress.[699],[700],[701] More specifically, eliciting the relaxation response (through whatever means is helpful) can be effective for those disorders too. Doing so also decreases anxiety, depression, anger and hostility, premenstrual problems, rheumatoid arthritis, temporomandibular joint pain, and IBS, to name just a few conditions.21,[702],[703],[704]
Note that as of 2018, meditation, clinical hypnosis, biofeedback, and guided imagery (all featured in more detail as Whole Health tools below) are on List One, the list of complementary and integrative health (CIH) approaches that are now covered by the VA in accordance with VHA Directive 1137. Sites are still determining specifically how these approaches will be offered, in terms of classes versus individual care, Telehealth versus live teaching, and overall decisions about what indications these approaches are best used for. This is discussed in more detail in Chapter 14.
If you want to learn more, refer to “Power of the Mind” overview and related Whole Health tools on the Whole Health Library website.
1. Psychotherapies: Important Examples
Psychotherapy is a general term for the treatment of mental health conditions that involves some sort of conversation/exploration with a mental health professional. A person may be asked to do “homework” to explore what is discussed in greater depth. It is important to be familiar with the different types available, so that you can suggest whichever type of therapy will be most useful for a given individual’s situation.1
Evidence-based psychotherapy[705] is a high priority related to VA mental health care,[706] and research supporting its use for an array of conditions is promising.[707],[708] Listed below are some of the most commonly used (and effective) psychotherapies available to Veterans through the VA. The list is by no means exhaustive. Find out which ones are available locally in your area.
Acceptance and Commitment Therapy[709]
Acceptance and Commitment Therapy (ACT) focuses on the function of a person’s thoughts, as opposed to trying to change their accuracy. Using mindful awareness and other techniques, people work to neutralize, or defuse, negative thoughts. The idea is to see a “…bad thought as a thought, no more, no less…”[710] ACT is popular in the VA for work with patients in pain and seems to be effective.[711] A 2015 review concluded that “…ACT is more effective than treatment as usual or placebo and...may be as effective in treating anxiety disorders, depression, addiction, and somatic health problems as established psychological interventions.”[712],[713] A 2017 review found ACT to be as effective as Cognitive Behavioral Therapy (CBT) in the treatment of anxiety and depression.33 More research is needed,[714] but ACT has also shown promise for seizure control, increasing psychological flexibility, and disease self-management, to name just a few areas of ACT research.[715] It is also showing promise for substance use disorders[716], fibromyalgia,[717] and cancer care.[718] It has been shown to be effective in group therapy for conditions like anxiety and depression.[719] A 2020 review concluded that it can help maintain long-term lifestyle and behavioral changes.[720]
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is built on the principle that our feelings and behaviors are influenced by our thinking patterns, not just by external people and events. It focuses on analyzing one’s thinking to identify thought patterns that cause harm and then modify them. Changing our thinking patterns can foster greater happiness and well-being.[721]
CBT uses a number of techniques. People might keep records of negative thoughts, feelings, and behaviors so that they can identify them and replace them. If they notice automatic thoughts about themselves, others, or life experiences, it is possible to begin to shift their responses. Negative thoughts are replaced with more adaptive thoughts. This is called cognitive restructuring, and it can be helpful with many psychological disorders. Once unhelpful thinking patterns, or cognitive distortions, are brought into a person’s awareness, a person can replace them with healthier patterns.
CBT is comparable with medications when it comes to depression treatment,[722] and it has been found to be helpful with preventing depression reoccurance.[723] It is effective as a treatment for both depression and anxiety in primary care.[724] It is also beneficial to people with PTSD, social anxiety, obsessive-compulsive disorder, panic disorder, generalized anxiety, and overall anxiety about their health.1 Recent 2018 reviews found it is also beneficial for subacute low back pain,[725] eating disorders,[726] treatment-resistant depression,[727] and insomnia.[728] It is also likely useful for addictions[729] and IBS[730] as well as numerous other indications. Cognitive Behavioral Therapy for Insomnia (CBT-I) is discussed in Chapter 9. There is also CBT-CP (for chronic pain) and CBT-SUD, which is specifically for substance use disorders.
CBT practitioners watch for a variety of different cognitive distortions. Examples include the following[731]:
|
|
While CBT-informed apps may not be as effective as face-to-face encounters, they have shown benefit in recent reviews.[732] Internet-Assisted CBT has good evidence in its favor.[733]
Cognitive Processing Therapy and Prolonged Exposure Techniques
Cognitive Processing Therapy (CPT)[734] and Prolonged Exposure Techniques (PE)[735] have been found to produce clinically significant improvement in PTSD symptoms in multiple randomized controlled trials.[736],[737] CPT focuses on changing maladaptive thoughts, while the main mechanism of PE is exposure exercises. Both CPT and PE are offered by the VHA, with CPT being the more widespread. The VA is actively studying the two for treatment of PTSD. Both have shown promise in research to date.[738],[739] A review of 750 Veteran charts, belonging to a diverse array of Veterans, found those who completed either therapy had significant reductions on their PTSD Checklist scores.[740]
CPT typically involves 12 sessions. The focus is modifying unhelpful thought patterns that developed after a person experienced one or more traumas. These may include thoughts about safety, trust, control, self-esteem, other people, and relationships. Developing a more balanced and healthy understanding of the traumatic experience, oneself, and the external world helps to promote recovery. CPT is frequently used with people with PTSD.
PE typically involves 8-15 sessions. Patients talk through a traumatic memory and do exercises where they repeatedly imagine being exposed to the traumatic experience in a safe environment. The exercises call up the fear associated with the trauma and they learn to change, or correct, what they experience. With time, the repeated exposures lead to the habituation and/or extinction of conditioned fear responses. The traumatic memories lose their power.
Dialectical Behavior Therapy
Initially developed in the 1990s as a treatment for borderline personality disorder, Dialectical Behavior Therapy (DBT) is now used for an array of diagnoses.[741] Therapists characterize a person’s behaviors as a natural reaction to reinforcers in the environment and focuses on shaping and reinforcing more adaptive behaviors while also offering a validating environment. In addition to being an effective treatment for people with borderline personality disorder,[742] DBT has also been found to reduce self-inflicted violence in people who are suicidal,[743] though a trial specifically with high-risk suicidal Veterans did not find benefit.[744] It seems to show some benefit in reducing suicidal ideation.[745]
Eye Movement Desensitization and Reprocessing[746]
Developed in the 1980s specifically to help people with traumatic memories and PTSD, Eye Movement Desensitization and Reprocessing (EMDR) involves a series of therapy sessions. During those sessions, a person receives bilateral stimulation, typically in the form of eye movements, tapping, and/or sound. Many practitioners follow a protocol that includes having people recall distressing images while receiving sensory inputs such as moving the eyes from side to side. The goal is to process negative memories and cope more effectively. It is not clear why moving the eyes in specific ways while working with distressing memories can be helpful.
Research indicates that the eye movements in EMDR do indeed have a beneficial effect.[747] Research indicates that EMDR is beneficial for PTSD, and the level of benefit is similar to that for other types of psychotherapy. EMDR seems to be more effective than medication alone.[748] It has comparable benefits with CBT for the treatment of obsessive-compulsive disorder.[749]
Interpersonal Therapy
Developed in the 1970s, Interpersonal Therapy (IPT) is based on the idea that many psychological symptoms arise through interpersonal distress. Treatment usually is offered for 12-16 weeks and focuses on exploring relationships and how they influence—and are influenced by—one’s behavior and mood. IPT’s efficacy, particularly for depression, has been shown in randomized controlled trials.[750],[751] It was found to be comparable to problem solving therapy and brief supportive psychotherapy in major depressive disorder for women with breast cancer.[752] It is one of several psychotherapies noted in a 2018 Cochrane review to be beneficial for treatment-resistant depression.[753]
Marital therapy
Marital therapy (MT), or couple’s therapy, involves working with both an individual and his/her significant other. If relationship problems are present, this can be a powerful approach. Several reviews have found that marital therapy is effective for treating depressive symptoms and reducing risk of reoccurance.[754] Involving a Veteran’s entire family in care can be helpful. Other examples of therapies that include loved ones include Behavioral Family Therapy, Integrative Behavioral Couples Therapy, Cognitive Behavioral Conjoint Therapy for PTSD.
Positive Psychology[755]
Established in 1998 by Seligman and colleagues, positive psychology focuses on a person’s skills and positive attributes, emphasizing how they can promote mental, physical, and emotional well-being. The focus is on strengths and positive qualities, rather than on what is wrong. Positive Psychology interventions have been found to lead to lasting increases in happiness and decreased depressive symptoms in numerous studies.75
The Best Possible Self exercise used in Positive Psychology, encourages people to envision themselves in their best possible future, after they have worked hard to get there; it has been found to have a significant effect on well-being.[756] Remember, when you are working with others (or yourself), it is important to celebrate successes and focus on the positive in addition to looking at what might be “wrong” with them.
Problem-Solving Therapy
Problem-Solving Therapy (PST) is a brief intervention, done in 4 to 8 sessions. A therapist reviews the problems a person is experiencing in his or her life and then focuses on solving one or more of those problems to teach the patient more effective problem-solving techniques. PST has shown modest improvement in study participants with depressive symptoms; most studies have been done in geriatric populations.[757],[758],[759] It was also found in one trial to prolong survival in older adults who have had a stroke,[760] and it can help with caregiver stress.[761]
Psychodynamic Therapy
Psychodynamic Therapy (PT) is defined differently in various studies. Also known as insight-oriented therapy, it focuses on gaining insight into unconscious processes and how they manifest in the way a person behaves.[762] PT has been used widely in clinical practice for the treatment of depressive disorders, and it seems to be effective.[763] Recent meta-analyses suggest that both short-term and long-term psychodynamic psychotherapy are effective for depressed patients. It also has benefit for people with personality disorders and anxiety disorders.[764],[765]
2. Autogenic Training
Autogenic Training (AT) was developed in 1932. Autogenic means “generated from within,” and many consider AT a form of self-hypnosis.[766] It involves a series of simple exercises people can do on their own to increase relaxation without having to rely on a trained hypnotherapist.
AT practice involves repeatedly thinking of several specific phrases, with the goal of producing feelings of warmth, heaviness, and calm throughout the body. The goal is to activate the parasympathetic nervous system (that is, to elicit the relaxation response). At the core of AT is a set of standard exercises which focus on six physical manifestations of relaxation in the body1:
- Heaviness in the musculoskeletal system
- Warmth in the circulatory system
- Awareness of the heartbeat
- Slowing down the breath
- Relaxing the abdomen
- Cooling the forehead
These exercises build on each other weekly. First, a person learns to relax the arms and legs. Next, they learn to regulate heart rate and breathing. Finally, relaxing the stomach, cooling the forehead, and feeling overall peace in the mind and body are added. Not everyone who does AT will experience all those sensations. In research studies, participants report overall effects of relaxation, such as reduced heart rate, lessening of muscular tension, and slower breathing, as well as reduced gastrointestinal activity, better concentration, less irritability, improved sleep, and other positive experiences.[767]
A Brief Autogenic Training Experience1
Try feeling each of the six AT manifestations as you read through this exercise. If you have difficulty, start by just focusing on one specific part of the body, like your hands.
- Musculoskeletal system. Allow yourself to feel heaviness in the muscles and bones. Can you tune in to specific bones or muscles?
- Warmth. Focus on blood flow. It might help to focus on your hands or feet at first. Can you make them warmer?
- Pulse. Can you tune in to your pulse? Where do you feel it?
- Breathing. Note your respiratory rate. Take a few slow deep breaths to slow it down, as you feel comfortable.
- Abdomen. Imagine your abdomen softening, like melting snow. Feel the breath in the abdomen.
- Forehead. Allow your forehead to cool down. You might imagine an ice cube melting on it, or a gentle breeze blowing across it.
A meta-analysis of 60 studies found significant positive effects of AT treatment for a number of diagnoses, including[768]:
- Anxiety
- Bronchial asthma
- Coronary heart disease
- Functional sleep disorders
- Migraine
- Mild-to-moderate depression
- Mild-to-moderate essential hypertension
- Raynaud's
- Somatoform pain disorder (unspecified type)
- Tension headache
For more information on AT, go to the Resources section at the end of this chapter.
3. Breathing Exercises
Breathing is essential to our survival, but most of the time we are not even aware we are doing it.[769] Focusing on breath is an excellent way to bring our awareness into our bodies and into the present moment, and different breathing techniques can help us move out of a hyperaroused, fight-or-flight state into a more relaxed parasympathetic state. Breathwork is often combined with other mind-body approaches.
The qualities of relaxed breathing make up the acronym DASS: Deep, Abdominal, Slow, and Smooth.89 Abdominal (diaphragmatic) breathing involves expanding the abdomen (instead of the chest) first when a breath is taken. Feeling motion when a hand is placed on the abdomen indicates it is being done correctly. Breathing is rapid and shallow during stressful situations, anxiety, and panic attacks, but within just a few minutes a person can learn how to deepen and slow breathing and ease their stress. Start with taking up to 10 slow, deep breaths. Deep breathing typically involves breathing in through the nose and out through the mouth. Start by both inhaling and exhaling for a count of 10.
There are many variations on rhythmic breathing.89 You can simply count to the same number (e.g., 10) on the inhale and the exhale, or you can count in for 4 and out for 6 (the 4-6 breath). The 4-7-8 breath has been used in Eastern practices for centuries. You breathe in for a count of 4, hold for a count of 7, and exhale for a count of 8. If you do it for more than a few breathing cycles when you are first learning, it may make you a bit light-headed. In general, however, breathing exercises are quite safe, and nearly everyone can learn to do them.
Slowing breathing rate can lower blood pressure.[770] A review of research on several specific breathing techniques found a trend toward improvement in asthma symptoms, noting more study is needed.[771] A review of trials involving hyperventilation also found a trend toward improvement.[772] Breathing exercises can also significantly improve pulmonary function and quality of life for lung cancer patients.[773] Practicing breathing against an appropriate positive end-expiratory pressure can improve function in COPD.[774] Breathing exercises can also relieve the symptoms of gastroesophageal reflux[775] and help with coping with chronic osteoarthritis pain.[776]
For more information, including a number of clinical tools you can use, go to the Resources section at the end of this chapter.
4. Creative Arts Therapies
Creative arts therapies (CATs), also known as expressive therapies, come in many forms.
- Art therapy is the therapeutic use of art making, with the support of a professional, by people living with illness, trauma, or other challenges. It can also be used by healthy people who seek personal development. Through creating art and reflecting on the experience, as well as on what they create, people can increase mindful awareness of themselves and others and learnt to cope better.
- Music therapy makes use of music to improve psychological, physical, cognitive, or social functioning.
- provides people the opportunity to tell their stories, set goals, solve problems, express feelings, and release pent-up emotions. Inner experience can be explored in greater depth, and social skills can be enhanced.
- Dance therapy/movement therapy is the psychotherapeutic use of movement to promote emotional, cognitive, social, and physical integration.
CATs during cancer treatment improve anxiety, depression, and overall quality of life.[777] Pain is significantly reduced as well, although fatigue is not, according to some studies. Art therapy leads to sustained improvement in cognitive function in elderly people.[778] Dance therapy improved gait and speed for Parkinson’s patients and healthy elderly people.[779] It also helped with executive function in Parkinson’s in one trial.[780] It may also help people with schizophrenia to function better,[781] and it seems to have some benefits for people with heart failure.[782] Movement and body awareness therapies also seem to have benefit as adjunct therapies for fibromyalgia.[783] Music therapy led to a mild reduction in post-operative pain[784] and depression,[785] and it improved performance during physical activity.[786] It seems to be beneficial in schizophrenia[787] and other mental health conditions,[788],[789] as well as for disruptive behavior, depression, and anxiety in dementia patients.[790],[791] Music therapy is beneficial in many ways to people at different stages of cancer care.[792] A 2018 systematic review did not find benefits of CATs for PTSD.[793]
In 2019, VA Health Services Research and Development (HSR&D) created the Evidence Map of Art Therapy.[794] The conclusion was that methodological issues in studies are common, but there are preliminary positive effects for a range of health conditions.
5. Journaling and Therapeutic Disclosure
Writing about stressful, upsetting and traumatic experiences has been found to improve physical and mental health.[795] Even just writing about emotionally difficult events or feelings for just 20 minutes at a time over four consecutive days has been found to be associated with relaxation and improvements with various health problems. The key is to “vent” emotionally when you write; therapeutic journaling is not merely about listing facts.
In general, journaling has comparable effects with other psychological interventions, but it can easily be done outside of a clinical environment. It may be useful for people in need of mental health support who live in remote areas, or who are unwilling/unable to do other forms of psychotherapy.
Expressive writing has shown to benefit for the following health concerns1,[796],[797],[798]:
- Depression
- Overall immune system functioning and immune response in HIV infection
- IBS
- Lung functioning in asthma
- Numbers of hospitalizations for people with cystic fibrosis
- Pain intensity with chronic pelvic pain
- Pain level and overall physical health in cancer patients
- Post-operative complications
- PTSD
- Rheumatoid arthritis severity
- Time to fall asleep in poor sleepers
- Wound healing rates
For more information, refer to the Resources section at the end of this chapter.
6. Progressive Muscle Relaxation and Progressive Relaxation
Progressive Muscle Relaxation (PMR) was developed in the 1920s.[799] It involves tensing and then relaxing various muscle groups in a sequential way. As the muscles relax, a person is encouraged to notice what it feels like when tension drains away. Early on, people are encouraged to repeatedly create tension and relaxation in different muscle groups; tension decreases with each repetition. At the end, a person may return to areas that are still carrying tension and relax them further. This technique can easily be taught to patients, and it can be adapted when a person has areas of tenderness or pain. PMR has been found to be useful with conditions such as chronic insomnia, migraines, cancer-related distress, IBS, and coping with inflammatory arthritis.119,[800] A recent study found that it can also reduce anxiety and improve sleep in people with COVID-19.[801] Combined with music, it reduced fatigue, lowered stress, and improved coping among intensive care nurses.[802]
Progressive Relaxation (PR) is similar to PMR, except it involves simply bringing awareness to muscle groups without increasing tension. It can be used by people who either cannot contract some of their muscles or find it uncomfortable to do so because of pain, recent surgery, or other reasons. It has not been studied as extensively, but it can be used for the same indications as PMR.
 Whole Health Tool: Biofeedback
Whole Health Tool: Biofeedback
What Is It?
Biofeedback uses various devices to measure physiological activities, with the intent of improving health or performance by learning to consciously control those activities. Clinical biofeedback emerged as a discipline starting in the late 1950s, as increasing numbers of technologies were developed to measure different body functions. Since that time, it has expanded dramatically.
Any number of body functions can be monitored in biofeedback. Certain biofeedback devices work best for different conditions. For example, measuring muscle tension can help with tension headaches, while neurofeedback works well for ADHD. Important examples of biofeedback devices include the following:
- Hand temperature (thermal biofeedback therapy)
- Skin conductance (electrodermal response)
- Respiratory rate and chest wall expansion
- Cardiovascular measurements, including heart rate (pulse) and heart rate variability (HRV), which are the beat-to-beat differences noted on a heart monitor
- Electroencephalography (EEG). EEG biofeedback is typically referred to as neurofeedback
- Muscle tension (electromyelography)
- Number of steps, measured on a pedometer or other wearable device
- Body weight (even your scale is a biofeedback device of sorts)
-
A variety of qualified professionals can offer biofeedback, ranging from psychologists and physicians to dentists, nurses, social workers, occupational therapists, physical therapists, and social workers.
How It Works
Seeing how these measurements change in real time in response to different emotions, thoughts, or behaviors empowers a person to mentally control physical functions they may not have previously been aware they could control. The end goal is to learn how to change body functions to improve health and/or performance, in a way where ideally the changes will endure without continued use of an instrument.
In a clinical setting, a practitioner might combine biofeedback with other treatments, such as Cognitive Behavioral Therapy (CBT) or relaxation techniques. Biofeedback can provide one element of a multi-faceted intervention, enhancing the efficacy of other treatments by drawing a person’s awareness to their own ability to consciously change their body functions.
How to Use It
Biofeedback is often offered by various mental health providers, particularly psychologists who have done additional certification. There are various products a person can use on their own to do biofeedback as well, but it is best to have support from a trained professional, especially early on.
When to Use It
Consider biofeedback for people who tend to be more technology-minded or like to see concrete data related to how their mental efforts affect them physically.
The Evidence Map of Biofeedback, as created by VA Health Services Research & Development (HSR&D), is shown below. This was based on comprehensive literature review up through March 2018.[803]
 Evidence Map of Biofeedback[804]
Evidence Map of Biofeedback[804]Recent studies have been especially favorable regarding the potential for biofeedback to treat various types of chronic pain[805] and swallowing function.[806] HRV can be useful for enhancing sports performance125 and improving pulmonary function during asthma attacks.[807] A recent, large-scale review and meta-analysis found no benefit for biofeedback for stress urinary incontinence in women.[808] A 2018 study found benefit of muscle tension biofeedback for stroke rehabilitation.[809] More studies are needed, but biofeedback shows potential benefit for treating OCD as well.129 Neurofeedback was found to benefit people with uncontrolled seizures.[810] Biofeedback helps with various types of headaches and has been given a “Grade A” evidence rating by various national organizations.[811] A recent systematic review found support for visual biofeedback for balance in elderly populations.[812] A 2019 Cochrane review concluded more irritable bowel syndrome (IBS) studies were needed to draw conclusions,[813] but a study indicates that home biofeedback helps with dyssynergic defecation.[814] Electrodermal feedback shows promise with reducing pain and chronic inflammation.[815]
A 2017 meta-analysis found benefit for HRV training for stress and anxiety.[816] One study found benefit for chronic back pain,125 another found it may help with reducing cravings in substance use disorders,[817] and still another found it reduced risk of admissions, emergency room visits, and depression in people with coronary artery disease.[818] Phone-based HRV interventions can improve cardiovagal function.[819]
A rating system for efficacy for biofeedback is used by national and international groups. Some of their ratings, as featured on the website of the Association for Applied Psychophysiology and Biofeedback, are as follows[820],[821]:
Biofeedback Research: A Summary
Level 5: Efficacious and Specific
- Constipation and fecal incontinence in females
- Fecal elimination disorders in females
- Urinary incontinence in females
Level 4: Efficacious
- Anxiety
- ADD and ADHD
- Constipation and fecal incontinence in males
- Fecal elimination disorders in males
- Headache in adults
- Hypertension
- Jaw area pain
- Temporomandibular disorders
- Urinary incontinence in males
Level 3: Probably efficacious
- Alcohol use disorder/substance use disorder
- Arthritis
- Asthma and other breathing problems
- Chest pain (non-cardiac)
- Chronic pain
- Epilepsy
- Hyperventilation
- Insomnia
- Low back pain
- Pediatric migraines
- Phantom limb pain
- Posture-related pain
- Stump pain
Level 2: Possibly efficacious
- Cancer and HIV, immune function</p\li>
- Cerebral palsy
- Chronic obstructive pulmonary disease</\li>
- Depressive disorders
- Diabetes mellitus
- Fibromyalgia
- Foot ulcers
- Hand dystonia
- Irritable bowel syndrome
- Knee pain
- Kneecap subluxation
- Mechanical ventilation
- Motion sickness
- Myocardial infarction
- PTSD
- Raynaud’s
- Repetitive strain injury
- Stroke
- Traumatic brain injury
- Tinnitus
- Urinary incontinence in children
- Vulvar vestibulitis
Level 1: Not empirically supported
- Autism
- Eating disorders
- Multiple sclerosis
- Spinal cord injury
The ratings of efficacy presented are compiled from The Association for Applied Psychophysiology and Biofeedback’s list of disorders and treatments as well as Yucha and Gilbert’s 2004 book on biofeedback and neurofeedback.
Biofeedback can enhance the effectiveness of other treatments by helping individuals become more aware of their own role in influencing health and disease; it can be quite empowering to patients.
What to Watch Out for (Harms)
Biofeedback is very safe, provided that instrumentation is operated correctly, and practitioners are able to set reasonable and safe parameters and goals for a person to aim for in terms of various physiological measures.
Tips from Your Whole Health Colleagues
Most experts would agree that it is best to obtain biofeedback from a qualified health care professional. Get to know practitioners at your site and in your local community. To find biofeedback professionals who practice in a certain part of the country, use the following as resources:
- Association for Applied Psychophysiology and Biofeedback
- Biofeedback Certification International Alliance. The BCIA was established to provide certification for biofeedback providers worldwide.
- International Society for Neuroregulation & Research (ISNR). Organization built around neurofeedback.
 Whole Health Tool: Guided Imagery
Whole Health Tool: Guided Imagery
What Is It?[822]
Guided imagery is a mind-body approach that uses the “mind’s eye”—one’s internal processes—to support healing. It is closely related to hypnosis, psychotherapy, and biofeedback, which may also incorporate the use of images as part of therapy. Also known as guided visualization, this mind-body practice has been used throughout history to change behaviors, perspectives, and physiology.
How It Works
A typical session might start with a person being guided through relaxation exercises. After that, the clinician and the patient begin exploring visual images, as the clinician offers various cues. Initially, a positive image might be created to help the patient relax more; for example, they may be encouraged to visit a safe or beautiful place. Sometimes the patient comes up with the image, and sometimes the practitioner does. Most often, they collaborate. Ultimately, guided imagery is controlled by the person experiencing it. This allows for a sense of mastery and control, which can fuel self-directed change efforts.[823]
Guided imagery promotes an altered state of awareness. It is a means by which a person can communicate with their subconscious, or unconscious, mind. Images can distract from pain, as people work with and even alter imagery related to their discomfort; a person may visualize a change in the pain’s color, or replace the pain with a different feeling, such as warmth. Imagery can also induce relaxation and help people cope more effectively with stress.
As they are working with an image, a person is encouraged to be very descriptive and to use all their senses. They are also encouraged to note emotions that arise. Different people gravitate more to focusing on senses.
Imagery can affect almost all major physiologic control systems of the body, including[824]:
- Respiration, heart rate and blood pressure
- Metabolic rate
- Digestive system motility and secretion
- Cortisol (stress hormone) levels
- Cholesterol levels
- Immune system activity
- Mood, including levels of anxiety and depression
How to Use It
Imagery can be taught one-on-one or in groups. A practitioner may record a session so that their patient/client will be able to do a given activity or exercise repeatedly.
Imagery can be used to bring about general stress reduction, to focus on a specific outcome, and to gain insight, particularly by interactively exploring imagery. A person might intentionally shift the imagery, and in so doing, shift what the imagery represents.
When to Use It
According to the VA Health Services Research & Development (VA HSR&D) group, based on a large-scale review of all imagery related studies up to March 2018, “There is moderate-level confidence that guided imagery is effective in improving diagnosis-related outcomes in patients with arthritis or other rheumatic diseases. The levels of confidence of guided imagery's effectiveness for other conditions was generally low, due to heterogeneity among the intervention modalities, high risk of bias, lack of blinding, and limited generalizability in some studies.”123 Evidence from the VA HSR&D review is also shown below.
While more study is clearly needed, guided imagery has shown particular promise with the following (noting that studies have their limitations)[825],[826],[827]:
|
|
A 2019 study found that a combination of PMR and Interactive Guided Imagery significantly reduced stress in cancer patients.[829]
It is possible for nearly anyone to use this technique. Some people prefer to work with a trained professional if they are using imagery to guide them through a physical or mental health issue. Professionals can teach patients to do ongoing work on their own. CDs and online downloads with imagery exercises are widely available. Refer to the Resources section at the end of this chapter for more information.
What to Watch Out for (Harms)
Guided imagery is not advised (or should be used with extreme care) for individuals who have psychosis, hallucinations, delusions, delirium, dementia, religious beliefs that might be in conflict with the use of imagery, or a history of unprocessed trauma that might come up during the session.
Tips from Your Whole Health Colleagues
A number of organizations offer information about Guided Imagery online. The VA Whole Health Mobile Apps and Online Tools suggests Health Journeys for Guided Imagery-related blogs and online imagery sessions.
9.  Whole Health Tool: Hypnosis
Whole Health Tool: Hypnosis
What Is It?
Hypnosis has been used for thousands of years, but Western scientists first became familiar with it in the 1770s. It is derived from the Greek word hypnos, “to sleep.” Hypnosis had its start in the 18th century with Franz Anton Mesmer, who used it to treat a variety of mental health disorders.[830] Most clinical hypnotherapists use approaches developed by Milton Erickson in the early 20th century. Erickson viewed hypnosis as a way to calm and quiet the conscious mind so that the subconscious could be accessed. A recent demographically balanced survey of 1000 American adults found that 7.6% of them had had hypnosis, and 63% of those reported benefit.[831]
The goal of hypnosis is to trigger, strengthen, and then make use of a trance state. Trance is a naturally occurring state during which unconscious thought and symbolic logic are more dominant, while “higher” thought and logic are less so. When a person is in a trance state, nonvoluntary and involuntary body process become more easily controlled and changeable.
How It Works
People are guided into the trance state through induction procedures which foster relaxation and an altered state of consciousness.1,[832] Attention becomes more focused, and distractions diminish. It is a similar state to being lost in thought, daydreaming, or being caught up in a good book.
Hypnosis uses two strategies while a person is in the trance-like state, in order to change sensations, perceptions, thoughts, feelings, and behaviors. First, mental imagery and symbolism are used. For example, a person may be asked to imagine what his/her pain looks like. If they describe it as a sharp red object, they might be encouraged to shift the imagery, so that colors represent a healthier state (e.g., soft and cool blue). A person may also envision certain desired behaviors or visualize a procedure or surgery going smoothly in advance.
The second of the two hypnotic strategies is the use of suggestions. Ideas and suggestions are brought up to support the goals of the session. They are most likely to be effective when a person is (1) relaxed, (2) open to suggestions, (3) able to experience sensations related to the suggestions, and (4) able to envision the suggestions leading to results.
People vary in terms of how well they can enter trance. Hypnotic ability is a relatively stable trait that often runs in families.[833]
When to Use It
Hypnosis is most often used for improving sleep, changing habits, and reducing pain, anxiety, and irritable bowel syndrome (IBS) symptoms.1 It has been found to provide non-pharmacological analgesia for invasive medical procedures,[834] and it reduced anesthesia needs, pain intensity, nausea, fatigue, and emotional upset in women undergoing breast surgery.[835] While it shows promise, more research is needed to support its use. In 2018, the VA Health Services Research & Development (VA HSR&D) group concluded, “There is low-confidence evidence that hypnosis provides benefit over comparator interventions for anxiety in patients with cancer, breast cancer care (i.e., pain, distress, fatigue, nausea/vomiting, and hot flashes), and weight loss in obese participants. Limitations to the body of evidence include small, combined sample sizes, poor study quality, and inconsistencies among the studies that were included in the systematic reviews.”123 The evidence gathered by VA HSR&D is shown in the graphic below.
The American Society of Clinical Hypnosis compiles hypnotherapy research. In general, they conclude evidence is supportive for the following (and the list is by no means exhaustive)[836],[837],[838],[839],[840]:
|
|
A 2019 Cochrane review concluded that, while there is no evidence that hypnosis is harmful, evidence is insufficient to tell if clinical hypnosis is more effective than other approaches for smoking cessation, and if it has benefit, the benefit is small.[842]
Often, hypnosis sessions are recorded so a person can use them repeatedly. Self-hypnosis can be a powerful approach itself.[843] Recent studies have also indicated that online hypnosis interventions may be effective for conditions such as migraines.[844]
What to Watch Out for (Harms)
Hypnosis tends to be very safe, according to number of meta-analyses.159,[845],[846] A 2018 review found no adverse event reports, noting that some studies did not report on safety at all.[847] Using hypnosis to work through events in one’s past may lead to the creation of false memories and trigger strong emotional reactions. Rarely, it can cause drowsiness, headache, dizziness, and/or anxiety.
Clinical hypnosis is very different from stage hypnosis. People may joke about not wanting to “cluck like a chicken,” and they can be gently reminded that people in trance never lose control.
Tips from Your Whole Health Colleagues
The American Society of Clinical Hypnosis and other groups offer certifications programs in hypnotherapy.
10.  Whole Health Tool: Meditation
Whole Health Tool: Meditation
What Is It?
Throughout human history, different forms of meditation have been developed in many cultures worldwide, often in association with religious traditions. Meditation’s broad scope makes defining and studying it challenging, because there are so many different types, with different styles, techniques, and goals. Some forms of meditation focus on mindful awareness, which is described in depth in Chapter 4. Others focus in different directions.
The word meditation derives from the Latin word “meditari” which means to engage in contemplation or reflection; the term is closely related to the word “measure,” as in doing things according to proper measure. In modern health care, it typically refers to a practice in which the mind is trained to maintain focused attention for various reasons, including to cultivate positive states of mind or to increase concentration and focus. As one description put it, “through the active and intentional shaping of our brains (neuroplasticity), we can shape well-being.”[848] There are meditations to foster awareness, and there are also meditations to enhance compassion and loving-kindness (as discussed in Chapter 10).
From the perspective of many contemplative traditions, meditation may be defined as spiritual practices intended to bring about enlightenment, self-actualization, or transcendence.168 From the perspective of neuroscience, meditation is frequently defined by researchers as one or more techniques for training attention, concentration, and/or awareness of how one’s own mind works, with the intent of enhancing self-regulation in some way.[849] Depending on their scientific background, spiritual or religious perspectives, and personal experience, people will resonate with different definitions, and it is important for meditation instructors (and clinical team members who discuss meditation with others) to be respectful of this.
Herbert Benson, who introduced the concept of the relaxation response, focused on the mental and physical effects of different forms of meditation, noting that many of them have certain features in common, in terms of their effect on the body.[850] They enlist a quiet environment, and many forms encourage people to settle down their bodies. People are encouraged to simply watch—but not get caught up in—distracting thoughts, and often they are encouraged to focus their attention on one specific thing, like a word (a mantram) or the breath. Of course, while appreciating these points of commonality, it is important to recognize that the variety and richness of different ways to meditate is born of thousands of years of human experience from around the world. As you discuss meditation as an option, remember that it is not simply a therapy, or a “one size fits all” approach to care. Different people will gravitate toward different approaches, and often, after meditation training, people tend to explore how it might fit into their overall worldview and, if relevant for them, their perspectives on spirituality and religion.
Meditation approaches have been classified in various ways. For example, practices may be based on one or more of the following overarching approaches168:
- Focused attention. The goal is to enhance concentration. Techniques use a single focus. Examples include breathing meditations, mantra meditation, and candle gazing.
- Open monitoring. Rather than one focus of concentration, these approaches encourage people to pay attention more broadly, noting what is happening with their thoughts, images, emotions, sensations, etc. Vipassana meditation, which informed the development of Mindfulness-Based Stress Reduction (MBSR), is an example.
- Non-dual. These approaches attempt to remove the distinction between self and other, to move into a more unified understanding of experience. These are taught, especially in Eastern traditions, to reduce attachments.
- Loving-kindness and compassion. These approaches move focus to well-being, often using mental imagery techniques. They focus on manipulating thoughts and emotions. A growing body of research supports their use.[851]
How It Works
An entire multidisciplinary field has arisen in the past few decades related to the scientific study of various types of meditation. Research in contemplative neuroscience, which often involves the use of measurement devices to study the brain (and occasionally other parts of the body) when a person is meditating, has been taking us in new directions with our understanding of the brain and its function. As described in Chapter 4, “Mindful Awareness,” various techniques can be used to alter brain activity in different areas
How to Use It
In developing a practice, here are some important considerations:
- Type of meditation. Remember that meditation is not always the stereotypical sitting on a cushion chanting; there are many options. The more familiar a team member is with different types of meditation, the more effective they will be at discussing options. Try different meditations yourself so you can speak from experience. Ask meditation teachers (in VA, they are often mental health professionals) for guidance.
- Whether or not to take a class. It can help for beginners to start out in a group environment.
- Frequency (once a week, three times a week, daily).
- How long? Many people start with a few minutes and build up. MBSR courses encourage people to meditate for 45 minutes six days a week.
Several different types of meditation commonly used in VA are listed here:
Mindfulness-Based Stress Reduction (MBSR) is one of the most common meditation-based training approaches used in U.S. health care settings.[852],[853] Jon Kabat-Zinn, who developed the course based on Buddhist meditation practices for the purpose of providing a secular experience for people in a hospital setting, introduced MBSR in the 1980s as an 8-week course that introduces learners to a number of different methods for cultivating mindful awareness, including seated meditation, movement approaches (hatha yoga), compassion meditation, and eating meditation, among others. It is taught in over 200 medical centers nationwide, and it is widely taught in the VA.
Mindfulness-Based Cognitive Therapy (MBCT) is an adaptation of the MBSR. It features cognitive therapy-based exercises linking thinking and its result impact on feelings. It has been found to be beneficial for depression.[854],[855],[856] MBCT has also been found to help Veterans with PTSD,[857] diabetes,[858] tinnitus,[859] irritable bowel syndrome (IBS),[860] and weight loss.[861]
iRest® Yoga Nidra. “iRest” is short for Integrative Restoration. This practice was developed specifically for a military/Veteran population in the early 2000s,[862] based on the ancient practice of Yoga Nidra. Richard Miller developed a ten-step protocol for “meditative self-inquiry.”[863] iRest Yoga Nidra is used regularly as part of weekly care at Walter Reed, and has been adopted in a number of VA medical centers too. Research indicates it is helpful with a variety of conditions, including depression, anxiety, quality of life, insomnia, pain, traumatic brain injury sequelae, low self-esteem, and overall patient satisfaction.[864]
Transcendental Meditation® (TM) reduces blood pressure[865] as well as anxiety and stress.[866] It decreases need for anxiety and PTSD medications in active military personnel.[867] In fMRI studies, it has been found to increase blood flow to attentional system of the brain and decrease flow to arousal areas.[868],[869]
Mantram Meditation (MM) was brought to the United States from India by Eknath Easwaran. A word, sound, or phrase is chanted repeatedly as a way to redirect thoughts, enhance concentration, and improve emotion. (If the person thinks the word/sound/phrase rather than speaking it aloud, it is called a “mantra” instead.) Mantram repetition elicits the relaxation response and helps with PTSD, insomnia, anxiety, and depression.[870],[871] It also improves pain and quality of life.[872] Several trainings for VA staff are available on TMS. Research indicates MM may work on certain areas of the brain differently from other forms of meditation, because of the use of language it requires.168
When to Use It
The number of studies of meditation has been increasing rapidly in recent years. The majority of the studies featured in Chapter 4, “Mindful Awareness,” describe the effects of various types of meditation in the context of cultivating mindfulness. The VA HSR&D’s Evidence-Based Synthesis Program created an Evidence Map of Mindfulness to offer a quick overview of the state of the research up through early 2014[873] (which is also featured in Chapter 4). In general, it is clear that meditation has great potential to be beneficial for many health concerns, and more research is needed because the quality of some of the research to date is varied.
Recent meta-analyses and reviews have noted the following about meditation:
- Many of the benefits seen in the research to date are related to psychological health and functioning. [874] Meditation reduces stress and improves capacity to cope with any number of chronic disorders. Anxiety and depression benefit, for example, as does chronic pain.[875],[876] PTSD does as well.191 Suicidal ideation decreases in Veterans.[877]
- Physical aspects of illnesses that are strongly influenced by emotions are also significantly affected.[878] Sleep and chronic pain both benefit,[879],[880],[881] as do blood pressure, fatigue, and quality of life after stroke.[882] Meditation seems, in general, to enhance resilience to stress.[883]
- The American Heart Association noted that “studies of meditation suggest a possible benefit on cardiovascular risk” (though quality and quantity of data are limited).[884]
- Meditation, at least in part because it regulates the stress response, suppresses chronic inflammation, alters immune system function and favorably influences the gut microbiome.[885],[886] It lengthens telomeres, which correlates to reduced morbidity and mortality.[887]
- It has been calculated, based on study data, that having people over 60 do TM regularly “...could avert nearly 200,000 stroke cases and 50,000 stroke-related deaths over the course of 15 years.”[888]
- The VA has done pioneering research focusing on MM, which has shown promise for a number of conditions.193
- TM drops blood pressure and average of 4/2 mm Hg, which is comparable to other lifestyle interventions.185
- Going on meditation retreats also has benefit, including on depression, anxiety, stress, and quality of life.[889]
What to Watch Out for (Harms)
Meditation tends to be safe overall. If someone has severe mental illness, they might be best served by training in a group environment with a well-trained instructor. Hallucinations can make meditation a challenge. It should be used carefully in people with significant trauma histories, psychosis, or hallucinations.
Tips from Your Whole Health Colleagues
Keep in mind that meditation is not, in itself, intended to be a therapy for a specific health condition or conditions. Rather, it is an overall approach to living and being in the world, and it can potentially be useful for everyone. Again, tailor the type of meditation used to the person. Some people prefer to be active, and tai chi and yoga (discussed in Chapter 5) are often referred to as movement-based meditations. Other activities can be meditative as well, but playing a sport, gardening, or other activities that involve focusing on the activity are not strictly types of meditation, based on the more specific sense of the term.
Research continues to confirm that even eight weeks of meditation training will lead to significant changes in brain function.[890]
Certification in meditation instruction is offered through a number of institutions, including the Oasis Institute Center for Mindfulness, University of Massachusetts Medical School, and the VA CALM program. See the Resources list at the end of this chapter.
Power of the Mind Resources
Websites
VA Whole Health and Related Sites
- A Patient Centered Approach To: Power of the Mind. Part of the Components of Health and Well-Being Video Series. https://www.youtube.com/watch?v=dbPNgJ4YkpM&feature=youtu.be
- Veterans Whole Health Education Handouts. https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
- An Introduction to the Power of the Mind
- Breathing and Health
- Progressive Muscle Relaxation and Progressive Relaxation
- Seated Meditation
- Biofeedback
- Mantram Meditation
- Autogenic Training
- Hypnotherapy
- Evidence Maps. Compilation of systematic review data by VA Health Services Research and Development (HSR&D). https://www.hsrd.research.va.gov/publications/esp/reports.cfm
- Evidence Map of Guided Imagery, Biofeedback, and Hypnosis. Summary of findings. https://www.hsrd.research.va.gov/publications/management_briefs/default.cfm?ManagementBriefsMenu=eBrief-no153&eBriefTitle=Guided+Imagery%2C+Biofeedback%2C+and+Hypnosis
- Cyber Seminar on Guided Imagery, Biofeedback, and Hypnosis. Includes detailed Evidence Maps for each intervention. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/3631-notes.pdf
- Evidence Map of Mindfulness. https://www.hsrd.research.va.gov/publications/esp/cam_mindfulness-REPORT.pdf
- Integrative Health Coordinating Center SharePoint Communities.
- Integrative Health Coordinating Center SharePoint on Biofeedback.
- https://www.va.gov/WHOLEHEALTH/professional-resources/Biofeedback.asp
- Integrative Health Coordinating Center SharePoint on Clinical Hypnosis.
- https://dvagov.sharepoint.com/sites/VHAOPCC/IHCC/SitePages/Clinical-Hypnosis.aspx
- Integrative Health Coordinating Center SharePoint on Guided Imagery. https://www.va.gov/WHOLEHEALTH/professional-resources/Guided_Imagery.asp
- CIH Listservs. To be added, contact:
- Biofeedback listserv: vhabiofeedback-cop@DVAGOV.onmicrosoft.com
- Clinical Hypnosis listserv: vhahypnosis@DVAGOV.onmicrosoft.com
- Guided Imagery listserv: vhaguided-imagery-community@DVAGOV.onmicrosoft.com
- Meditation listserv: vhameditation-community@DVAGOV.onmicrosoft.com
- Other listservs: Lana.Frankenfield@va.gov
- National CIH Subject Matter Experts, as of FY20.
- Biofeedback: David Gaffney. David.Gaffney@va.gov
- Clinical Hypnosis: David Gaffney. David.Gaffney@va.gov
- Guided Imagery: David Gaffney. David.Gaffney@va.gov
- Meditation: Kavitha Reddy Kavitha.Reddy@va.gov; or Alison Whitehead Alison.Whitehead@va.gov
- Guided Meditation Audio Files. https://www.va.gov/WHOLEHEALTH/circle-of-health/mindful-awareness.asp
- Introduction to Meditation with Dr. Greg Sherpa (5 minutes)
- Grounding Meditation (5 minutes)
- Mindfulness of Breathing Meditation (10 minutes)
- Mindfulness of Sounds Meditation (10 minutes)
- Compassionate Breathing Meditation (10 minutes)
- Loving Kindness Meditation (10 minutes)
- Body Scan Meditation (15 minutes)
- Body Scan with Loving Kindness Phrases (15 minutes)
- An Intro on Mindfulness and Using the Personal Health Inventory (22 minutes)
- Paced Breathing (7 minutes)
- Mental Muscle Relaxation (5 minutes)
- Mini Mental Vacation (7 ½ minutes)
- CALM Program. This training course for mindfulness instructors is offered through the OPCC&CT. The course contact person is Dr. Greg Serpa, at John.Serpa@va.gov.
- STAR Well-Kit. http://www.warrelatedillness.va.gov/education/STAR/
- Meditation materials include: Richard Miller’s “Guided Meditation” and Patrick Crehan—Mindfulness Meditation (where a Veteran describes his experience).
- Breathing materials include: James Gordon’s “Soft Belly Breathing” and Ben King, a Veteran who describes his experience with breathing exercises.
- National Center for Health Promotion and Disease Prevention. A number of resources for stress management as part of the Healthy Living messages. http://www.prevention.va.gov/Healthy_Living/
Whole Health Library Website
- Power of the Mind. Overview. https://wholehealth.wisc.edu/overviews/power-of-the-mind
- Working with Our Thinking. https://wholehealth.wisc.edu/tools/working-with-our-thinking
- Therapeutic Journaling. https://wholehealth.wisc.edu/tools/therapeutic-journaling
- Autogenic Training. https://wholehealth.wisc.edu/tools/autogenic-training
- Progressive Muscle Relaxation. https://www.va.gov/WHOLEHEALTHLIBRARY/tools/progressive-muscle-relaxation.asp
- Progressive Muscle Relaxation and Progressive Relaxation. https://www.va.gov/WHOLEHEALTH/veteran-handouts/docs/ProgressMuscleRelax__Final508_11-13-2018.pdf
- Breathing and Health (General). https://www.va.gov/WHOLEHEALTH/veteran-handouts/docs/BreathingAndHealth-508Final-9-4-2018.pdf
- The Power of Breath: Diaphragmatic Breathing. https://wholehealth.wisc.edu/tools/diaphragmatic-breathing/
- Power of the Mind: Additional Resources. Refer to this link for an even more detailed list of resources related to different mind-body approaches.
- https://wholehealth.wisc.edu/tools/power-of-the-mind
- Balloon Self-Hypnosis Technique for IBS and Abdominal Pain. https://wholehealth.wisc.edu/tools/balloon-self-hypnosis-technique-ibs-abdominal-pain
- Coping with Grief. Overview. https://wholehealth.wisc.edu/overviews/coping-with-grief
- Personal Health Plan Template. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/08/Brief-Personal-Health-Plan-Template.pdf
- Whole Health for Skill Building: Power of the Mind.
- https://wholehealth.wisc.edu/courses/whole-health-skill-building/
- Faculty Guide
- Veteran Handout <>PowerPoints
- Mindful Awareness Script: “Dropping In”
Other Websites
- Academy for Guided Imagery. www.acadgi.com
- American Society of Clinical Hypnosis. www.asch.net
- Association for Applied Psychophysiology and Biofeedback. Check out the “Clinician’s Resource Library.” https://www.aapb.org/i4a/pages/index.cfm?pageid=1
- Biofeedback Certification International Alliance. https://www.bcia.org/i4a/pages/index.cfm?pageid=1
- Dartmouth College Student Wellness Center. Offers a variety of short guided meditation exercises, as well as others for relaxation and guided imagery. https://www.dartmouth.edu/~healthed/relax/downloads.html
- Gratefulness. Compilation of gratitude resources. www.gratefulness.org
- Health Journeys. Numerous resources involving guided imagery for various health conditions and scenarios. http://www.healthjourneys.com/
- Health Journeys Guided Imagery Audio Library. Available as a free podcast. https://www.healthjourneys.com/partneraccess/index/display/token/0O_nsrcONaPPPo2qdk8IpDpyc6s86k9FnriuQkwdqFl6FIKIfhAfUAGxEVuEehkUS1t4MypCQzTX9Qi6JE8rNpUsGM67wnig3lc8yeSkTsBdTbW52A0I2hQDMMGXmDYN3lqQRMbP5786IQcfM7y8Gg==
- University of Massachusetts Memorial Health Care Center for Mindfulness. https://www.umassmemorialhealthcare.org/umass-memorial-center-mindfulness
Books
- A Whole New Mind: Why Right-Brainers Will Rule the Future, Daniel Pink (2006)
- Art as Medicine: Creating a Therapy of the Imagination, Shaun McNif (1992)
- Conscious Breathing: Breathwork for Health, Stress Release, and Personal Mastery, Gay Hendricks (1995)
- Evidence-Based Practice in Biofeedback and Neurofeedback (3rd ed), Gabriel Tan (2017)
- Guided Imagery for Groups, Andrew Schwartz, (1997)
- Guided Imagery for Self-Healing, Martin Rossman (2000)
- How to Meditate: A Guide to Self-Discovery, Lawrence Le Shan (1998)
- In an Unspoken Voice: How the Body Releases Trauma and Restores Goodness, Peter Levine (2010)
- Open Up by Writing It Down, James Pennebaker (2016)
- Practicing Mindfulness: 75 Essential Meditations to Reduce Stress, Improve Mental Health, and Find Peace in the Everyday, Matthew Sockolov (2018)
- Teaching Meditation to Children, David Fontana (2007)
- The Body Keeps the Score: Brain Mind, and Body in the Healing of Trauma, Bessel van der Kolk (2015)
- The Cure Within: A History of Mind-Body Medicine, Anne Harrington (2009)
- The Emotional Freedom Technique Manual, Gary Craig (2008)
- The Highly Sensitive Person, Elaine Aron (1997)
- The Meditator’s Atlas: A Roadmap of the Inner World, Matthew Flickstein (2007)
- The Relaxation Response, Herbert Benson (2000)
- When Things Fall Apart: Heart Advice for Difficult Times, Pema Chodron (2000)
- Why Zebras Don’t Get Ulcers, Robert Sapolsky (2004)
- Writing to Heal, James Pennebaker (2004)
- Books by Cheri Huber (focus on various aspects of Meditation)
- Perils and Pitfalls of Practice: Responses to Questions about Meditation
- The Fear Book
- The Depression Book
- When You’re Falling, Dive
Apps and Monitoring Software
- The popular phone apps listed below are free, although most have in-app purchases or memberships available. Find them by searching online or in your device’s app store. Note that these are not scientifically tested—you may want to have people try a variety (or search for others) to see what is most helpful.
- 10% Happier. Meditation for Fidgety Skeptics. Focused on those who are not sure they want to meditate. Premium version has videos.
- Anxiety Free. Self-hypnosis for anxiety and stress management.
- Aura. Has daily meditations, nature sounds, stories, music, and coaching.
- BioZen. Created by U.S. Department ofDefense.
- Breathe2Relax. Guides you in diaphragmatic breathing.
- Breethe. Variety of meditations, inspirational talks, and lectures.
- Buddhify. 200+ meditations for different indications. One-time purchase fee; in-app purchases also available.
- Calm. Had multiple meditations and progress trackers.
- Deep Sleep and Relax Hypnosis. Self-hypnosis for people with poor sleep.
- Digipill. Uses neurolinguistic programming and psychoacoustics. Hypnotic suggestions focused on an array of topics.
- Elite HRV.
- Ensō. For those with more experience. Has timers that can be set at different intervals to keep you alert.
- Happify. Helps users with resources to combat negativity, anxiety and stress.
- Headspace. Hundreds of guided meditations. Monthly fee after trial.
- Inscape. Meditations, music, and breathing exercises suggested based on your goals.
- Meditation and Relaxation Pro. Simple and effective guides that allow you to choose a focus or goal.
- Personal Zen. Games to reduce anxiety levels.
- Sattva. Build around meditation traditions form India.
- Smiling Mind. Created by a psychologist, tailors meditations to age; includes programs for group use.
- The Breathing App. Allows you to customize your own breathing exercises.
- The Mindfulness App. Offers a 5-day guided practice and introduction to mindfulness, personalized options, and daily reminder settings.
Special thanks to Shilagh Mirgain, PhD, and Janice Singles, PsyD, who wrote the original Whole Health Library materials on Power of the Mind that inspired content for much of this chapter.



















