Passport to Whole Health: Chapter 3
Chapter 3. Whole Health Clinical Care, Part II: Equipping, Personal Health Planning, and Integration

The real voyage of discovery consists not in seeking new landscapes, but in having new eyes.
―Marcel Proust
Chapter 2 introduces the Whole Health Clinical Care Journey and then focuses in on Empowerment, Fundamentals, and Mapping to the MAP. It closes with a discussion about Shared Goals. This chapter focuses on how to Equip Veterans, incorporate Personal Health Planning, and Integrate all of these different elements in a way that flows well and supports creation of an overall Whole Health System. The role of SMART goals is also discussed.
Equip
In order to reach their goals and move forward with their Mission, Aspiration, Purpose (MAP), Veterans—and care team members, whose self-care and well-being are also fundamentally important—must be equipped with the education, resources, skill- building, and support they need. To optimize care, team members need to be able to know what is available to equip Veterans and themselves, and they need to know who is available as well. There is a matchmaking element to Whole Health care.
As you consider how best to Equip Veterans for Whole Health, keep the following in mind:
- The Office of Patient Centered Care and Cultural Transformation (OPCC&CT) has created a number of educational resources, ranging from live courses taught at sites all around the country, to virtual offerings, such as online instruction. Multiple educational offerings for clinicians and non-clinicians are featured in the Whole Health tool, “A List of Whole Health Education Offerings” in the next section. The first two course listings are for half-day courses that can be taught at any site, with continuing education units offered. They have train-the-trainer curricula as well, so you or others at your site can teach others how to teach about Whole Health.
- Many sites have developed a list of local and facility-specific Whole Health resources. If your site has one already, keep adding to it. If you do not have one, create one!
- The Integrative Health Coordinating Center (IHCC) has a list of online, vetted complementary and integrative health (CIH) resources as well as a TeleWholeHealth to aid in delivery of CIH approaches.
- The Resources sections after the chapters throughout this reference guide were created to help you fill your Whole Health toolbox with ways to equip Veterans.
- Equipping is an important focus of Well-Being Programs, which are one of the three parts of the Whole Health System (Figure 1-4). Suggestions for how to support Veterans through supporting CIH approaches are provided in Chapters 14-18.
- Equipping also includes offering them the best that current clinical services have to offer, depending on Veterans’ needs.
- Ask for support from your Field Implementation Team Consultant (FIT-C). There is one assigned to each site, and they are experts in tailoring Whole Health resources to a site’s specific needs. You can find out who is assigned to your site on the FIT SharePoint Page.
- One of the best approaches to learning about all these resources is to try them out for yourself, with your own self-care.
Whole Health Tool: A List of Whole Health Education Offerings
|
Offerings for All Employees |
|||
|
Whole Health for You and Me (WH102/102F)
|
Enables VA employees to personally experience WH in order to help foster a culture where WH is the model of care for Veterans. Employees learn about setting personal goals, mindfulness, self-care, resilience, complementary and integrative health, and the power of community through highly experiential activities. This course also introduces Employee Whole Health. It is now available as an initial 4-hour introduction to Whole Health; Whole Health 101 (8 hours) may continue being offered by sites that have already been using it. Train-the-Trainer curriculum is available for this course. |
|
|
|
Clinical Offerings (Primary focus: training clinicians to incorporate WH into their clinical practice. Whole Health Staff are developing virtual options for both existing and new courses.) |
|||
|
Applying Whole Health in Clinical Care (WH202) |
An intensive, highly practical 4-hour experience for busy VA clinicians and clinical teams that provides additional skills and tools to make clinical practice more effective, efficient, and satisfying. According to research, the vast majority of patients with chronic disease do not feel they are able to effectively support their own self-care and self-management. Whole Health 202 offers clinicians and teams a quick start guide for helping patients optimize their own health and well-being. An introductory course such as Whole Health 102 is recommended but not a prerequisite. Train-the-Trainer curriculum is available for this course. |
|
|
|
Whole Health in Your Practice |
Advances skills in the delivery of personalized, proactive, patient-driven care, extending beyond disease-based care to focus on health creation. Provides current evidence-based information and case studies and Complementary and Integrative Health approaches to treating common conditions. This course is largely experiential, with a focus on personal health planning and how to implement and sustain WH in practical and meaningful ways. Emphasis on clinician self- care and burnout prevention. |
>ul>
|
|
|
Whole Health for Pain and Suffering |
Education and skills-based practice on WH approaches to pain and suffering using complementary and integrative therapies. Provides evidence-based, safe, and effective non-pharmaceutical approaches to pain care. Shows how mind-body approaches and self-management can support coping and well-being for Veterans with pain. Emphasis on clinician self-care and burnout prevention. |
|
|
|
Eating for Whole Health |
Introduces clinicians to the WH approach as it relates to a fundamental aspect of self-care: nutrition. This advanced, stand- alone course is informed by the latest research, with areas of focus including optimizing nutrition for specific disease states, preventing chronic diseases, collaborating effectively with dietitians and other care team members, and sharing nutrition success stories. |
|
|
|
Whole Health for Mental Health |
Explores a system of care where mental health is seamlessly incorporated as a core aspect of whole-person care. This highly experiential course offers tools and skill based on positive psychology, the recovery model, psychotherapeutic approaches, and evidence-based conventional care and CIH in order to assist Veterans with mental health concerns and enhance mental wellbeing for Veterans and VA staff. |
|
|
|
Whole Health Clinical Care Symposium |
This longitudinal symposium provides training, coaching and focused groupwork time for site- based teams comprised of a leadership sponsor, a Whole Health champion, a representative clinician, and an additional key stakeholder. It focuses on supporting teams in leading, facilitating, and sustaining Whole Health cultural transformation in clinical care settings at the facility level, using the Designation Framework for Whole Health System Implementation and applying change management principles |
|
|
|
Fundamentals of Whole Health Clinical Care
|
Introduces the fundamentals of Whole Health clinical care to busy providers and healthcare teams. The class focuses on making even small changes in a busy practice to support Whole Health. The course addresses What is Whole Health, what are the key elements of Whole Health Clinical Care, and how to begin aligning care with a Veteran’s Mission, Aspiration and Purpose (Mapping to the Map). |
|
|
|
|
Introduces the fundamentals of CIH approaches to healthcare and how they differ from conventional medicine. The class provides an overview of various CIH approaches and explores how they hold the potential to improve clinical outcomes. The course discusses CIH approaches looking at their unique benefits and how they can be an important part of caring for Veterans. |
|
|
|
A Closer Look at List One Approaches |
VA has identified certain Complementary and Integrative approaches as having enough evidence of promising or potential benefit to become part of the standard benefits package for Veterans. This training helps clinical staff understand more about these specific therapies and how to incorporate these into their clinical care. |
|
|
|
Non-Clinical Offerings (Primary focus: training non-clinicians in their role as WH Coach, Facilitator, Partner, or Mentor.) |
|||
|
Whole Health Coaching |
This highly experiential and practical course provides instruction and mentoring on effective communication and coaching skills. In VA’s Whole Health Coaching model, the coach works with a Veteran individually or in a group, to proactively take action toward behavior change that aligns with the Veteran’s goals and values in a present-and future-oriented process. Graduates are eligible to become National Board-Certified Health and Wellness Coaches. |
|
|
|
Taking Charge of My Life and Health Facilitator Training |
This train-the-facilitator course teaches Veteran peer facilitators how to lead the Taking Charge of My Life and Health group that empowers Veteran participants to become more proactive in their own health. Focus is on effective group facilitation skills through practice with feedback. Facilitators learn to assist Veterans in exploring their life mission, aspirations, and purpose; learning the practice of mindfulness; and goal setting, skill-building, and self-management of their health with the support of their peers. Train-the-Trainer curriculum is in pilot stage for this course. |
|
|
|
Whole Health Partner Training |
WH Partners receive training in recruiting and engaging Veterans in the WH System. Partners learn how to guide Veterans through various offerings within the WH Pathway and to resources available in Wellness and Complementary and Integrative Health circles. Partners become well-versed in the Circle of Health, Four-Stage WH Process for navigating change, and the Personal Health Inventory. |
|
|
|
Whole Health Mentor Course |
Participants learn to support, enhance, and ensure the fidelity of services provided by the Whole Health Pathway including Whole Health Coaches, Whole Health Facilitators, and Whole Health Partners. Mentor participants will learn how to provide ongoing skill training and mentoring to staff through effective feedback techniques, continuing education, and skillful coordination with supervisors and clinical staff. |
|
|
|
Virtual Offerings |
|||
|
Whole Health Library |
This is the go-to site for all things WH. It includes essential tips on getting started with WH, overviews on all aspects of WH that synthesize the latest research, and practical tools to use at the point of care with Veterans. It also includes links to resources for both self-care and professional care. |
Available at https://wholehealth.wisc.edu/ |
|
|
Whole Health TMS/TRAIN Courses |
Accredited learning modules including Whole Health Foundation: A Personal Experience, Clinician Self-Care: You in the Center of the Circle of Health, Introduction to Complementary and Integrative Health Approaches, Mindful Awareness, Eating for Whole Health: Introduction to Functional Nutrition, Whole Health for Mental Health and Wellbeing, Whole Health Coaching Demonstration, Whole Health for Mental Health and Wellbeing Interviews, Nutrition for Pain: Whole Health Tools for Providers. Non- accredited modules include Whole Health Foundation: A Personal Experience and Facilitation Tips and Techniques. Additional courses are under development. |
|
|
|
Passport to Whole Health Reference Manual
|
Comprehensive reference manual on WH, the WH System, Personal Health Planning, mindful awareness, the areas of self-care, complementary and integrative health, and whole systems of medicine, etc. Complete with up-to-date hyperlinks of evidence and other resources. Passport to Whole Health Link |
|
|
|
Communities of Practice |
The following monthly calls are offered to continue skill-building, knowledge, and implementation strategies: WH Clinical COP, WH Coaching COP, and WH Facilitated Groups COP. Whole Health Communities of Practice |
|
|
|
Where to Start? (Your site's Field Implementation Team Consultant can help you develop an education strategy that best supports WH transformation, and can also provide additional WH education resources and support.) |
|||
|
Clinicians |
Non-Clinicians |
||
|
|
||
|
Virtual offerings are a great resource for clinicians and non-clinicians unable to attend a face-to-face course, or as a supplement to in-person offerings. Find face-to-face course sign-up and more information on the |
|||
A few additional options to consider include:
- As noted above, each VA facility has a FIT-C, who is an expert in all things Whole Health. A group of them is available to visit sites, when appropriate, and offer specific guidance related to Whole Health implementation. Check your Sharepoint site for a list of FIT-C.
- Skill-Building Courses for Veterans. These 60-80 minute courses, which focus on each of the eight areas of self-care, are available at the Whole Health for Skill Building section of the Whole Health Library website. Materials for each course include slides, participant handouts, and a faculty guide.
TeleWholeHealth
TeleWholeHealth is an important mechanism for equipping Veterans with Whole Health resources, tools, and experiences. It is built upon VA’s Telehealth offerings and allows Veterans who may not otherwise have access to Whole Health resources to experience them virtually. Offerings may be focused on disease/symptom management and/or wellness. Offering CIH approaches via TeleWholeHealth allows them to be shared at other VA medical centers, Community Based Outpatient Clinics, and non-VA locations, which markedly improves access to them.
Key TeleWholeHealth links include:
Examples of what can be offered through TeleWholeHealth include TeleYoga, TeleMeditation, TeleTaiChi (and qi gong), TeleWholeHealth Coaching, Intro to Whole Health Telehealth classes, and TeleWholeHealth Facilitated groups, such as Taking Charge of My Life and Health.
If you wish to implement TeleWholeHealth, there is a local implementation process you can follow:
- Meet with the Facility Telehealth Coordinator (FTC)
- Determine what Telehealth modality is appropriate for the service you wish to offer
- If you will be using Clinical Video Telehealth, a Telehealth Service Agreement will need to be created, detailing what services are to be provided
- Establish clinic locations and utilize appropriate Whole Health and Telehealth stop codes and CHAR 4 codes
- Implement a pathway for service, e.g., consults, scheduling, etc.
See the Resources section at the end of this chapter for a list of national TeleWholeHealth resources.
Personal Health Planning
Personal health planning is the process through which Veterans identify their MAP and outline their health and self-care goals (linked to their MAP). It also includes the activities and resources to help them pursue those goals. It begins the moment a Veteran first learns about Whole Health and continues throughout their Whole Health Clinical Care experience (Figure 2-1). The Personal Health Plan (PHP) is a summary of this information.
In the clinical setting, the personal health planning process is guided by Whole Health assessments, which may be informed by tools such as the Personal Health Inventory (PHI). The PHP evolves as Veterans choose which areas of the Circle of Health they would like to focus on and set goals (e.g., shared goals and SMART goals) related to what matters most to them. Ideally, every Veteran is able to articulate their PHP, and every member of the team is willing and able to check in about how it is going with moving toward MAP and achieving goals. The best-case scenario would be that the Veteran’s PHP is accessible to everyone on the health care team, no matter what a team member’s particular role might be. Ideally, everyone on the team is aware of what a Veteran is working on and offering encouragement, and documentation reflects this.
The personal health planning process is unique for each person, focusing on each individual’s values, health conditions, needs, and circumstances. It is built upon compassion, empathy, respect, excellent communication, cultural humility, and a genuine desire on the part of caregivers to support the health and well-being of Veterans. Ideally, these caregivers are applying Whole Health in their own lives as well.
Personal health planning is “where the rubber meets the road” in Whole Health care. In short, it involves gathering information, setting goals together with each Veteran, assembling the key elements of a plan, and then exploring how the Veteran can learn necessary skills to empower themselves to do self-care. It is also important to co-create a Whole Health team with Veterans, make appropriate referrals, and plan follow up.
Assessing Whole Health. Health assessments come in many shapes and sizes. Asking the MAP questions may be all there is time for in some visits. Forms filled out by the patient while checking in to a clinic can be helpful. Of course, gathering an updated patient history can also provide valuable information. So is a physical examination. One emphasis of the Whole Health approach is to bring additional focus to aspects of self-care, with an emphasis not only on the areas a person wants to work on, but also on what is going well. MyHealtheVet and the National Center for Health Promotion and Disease Prevention offer a number of assessment materials that shift focus in this way.
Often, a Whole Health assessment will, as time and other factors allow, involve completing a PHI. PHIs come in many forms. The PHI featured on the next page is the one most commonly being used. It starts with overall ratings of physical well-being, mental/emotional well-being, and quality of life (the “Vitality Signs”). Next, it moves through a series of questions related to MAP and the various self-care components of the Circle of Health. There is one question about Professional Care too. People rate where they are and where they would like to be when it comes to different aspects of care. The PHI concludes by asking what Whole Health (and achieving their MAP) would look like for a person and the next steps they want to take to get closer to that state. The team can review the PHI in advance and be better-equipped to have a patient-centered discussion. Answers can be entered into the medical record so that everyone on the team can access them.
Other PHIs are in use at different VA facilities. The more detailed PHI, known formally as the PHI Booklet, goes over the Whole Health process in layman’s terms and allows Veterans to share more about how they chose to rate themselves in terms of where they are and where they want to be for various elements of the Circle of Health. The Resources Section at the end of this chapter has information and links to various PHIs. Note: most sites using PHIs have reported they have better success if they do not mail PHIs out to Veterans, but rather ask them to fill them out just prior to seeing a clinician or team.
Personal Health Inventory (PHI)

Personal Health Inventory
- “Me” at the center of the circle: This represents what is important to you in your life, and may include your mission, aspirations, or purpose. Your care focuses on you as a unique person.
- Mindful awareness is about noticing what is happening when it happens.
- Your everyday actions make up the green circle. Your options and choices may be affected by many factors.
- The next ring is professional care (tests, medications, treatments, surgeries, and counseling). This section includes complementary approaches like acupuncture and yoga.
- The outer ring includes the people, places, and resources in your community. Your community has a powerful influence on your personal experience of health and well-being.

Rate where you feel you are on the scales below from 1-5, with 1 being miserable and 5 being great.
|
Physical Well-Being |
||||
|
1 Not So Good |
2 |
3 |
4 |
5 Great |
|
Mental/Emotional Well-Being |
||||
|
1 Not So Good |
2 |
3 |
4 |
5 Great |
|
Life: How is it to live your day-to-day life |
||||
|
1 Not So Good |
2 |
3 |
4 |
5 Great |
What matters most to you in your life right now? Write a few words to capture your thoughts:
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
_________________________________________________________________________________________
Where You Are and Where You Would Like to Be
For each area below, consider“Where you are”and“Where you want to be.”Write in a number between 1 (low) and 5 (high) that best represents where you are and where you want to be. You do not need to be a “5” in any of the areas now, nor even wish to be a “5” in the future.
|
Area of Self-Care |
Where I am Now (1-5) |
Where I Want to Be (1-5) |
|
Moving the Body: Our physical, mental, and emotional health are impacted by the amount and kind of movement we do. |
|
|
|
Recharge: Our bodies and minds need rest in order to optimize our health. Recharging also involves activities that replenish your mental and physical energy. |
|
|
|
Food and Drink: What we eat, and drink can have a huge effect on how we experience life, both physically and mentally. |
|
|
|
Personal Development: Our health is impacted by how we spend our time. We feel best when we can do things that really matter to us or bring us joy. |
|
|
|
Family, Friends, and Co-Workers: Our relationships, including those with pets, have as significant an effect on our physical and emotional health as any other factor associated with well-being. |
|
|
|
Spirit and Soul: Connecting with something greater than ourselves may provide a sense of meaning and purpose, peace, or comfort. Spiritual connection can take many forms. |
|
|
|
Surroundings: Surroundings include where we live, work, learn, play, and worship— both indoors and out. Safe, stable, and comfortable surroundings have a positive effect on our health. |
|
|
|
Power of the Mind: Our thoughts are powerful and can affect our physical, mental, and emotional health. Changing our mindset can aid in healing and coping. |
|
|
|
Professional Care: Partnering with your health care team to address your health concerns, understand care options, and define actions you may take to promote your health and goals. |
|
|
Reflections
Now that you have thought about what matters to you in all of these areas, what would your life look like if you had the health you want? What kind of activities would you be doing? Or how might you feel different? What area might you focus on?
_________________________________________________________________________________________
_________________________________________________________________________________________
What might get in the way? How might you start?
_________________________________________________________________________________________
_________________________________________________________________________________________
To become more familiar with the PHI, fill it out for yourself. This can serve as a helpful “mindful awareness moment” when you pause to reflect for a moment on your own Whole Health care.
Some PHI Pointers. As you review a PHI, consider the following:
- Answers for the first few questions, the Vitality Signs, can give an initial sense of whether or not a person is at risk for suicide.
- The question after the Vitality Signs covers some initial information to help you learn about their MAP.
- The next section, on the second page, allows a person to share perceptions of where they are and where they would like to be when it comes to the various aspects of Whole Health. This opens the door for Motivational Interviewing. The numbers can give you a sense of what to prioritize as you talk with them, but they may not reflect which areas they ultimately choose as a focus. People do not always choose the item they rated lowest. The numbers are simply a conversation starter.
- Remember to focus on positives too and honor strengths. Note areas where a person is already doing well, based on their self-rating. That area of their life might support them as they work on other areas where they gave themselves lower ratings.
- How will you administer the PHI? Will people fill it out in the waiting area, or while they are visiting with one of your team members, or at some other point?
- How often should you have a person complete the PHI again to keep it current? Some facilities suggest that a Veteran complete a new PHI yearly.
- PHIs save time. After looking over the information, you can rapidly move to asking more in-depth questions, because many of the questions you would have initially asked have already been answered in their written responses. This allows the conversation to become focused more rapidly.
- PHIs get you started with creating the PHP and setting goals. Patients are asked where they would like to start, and what specifically they can do to get underway. When in doubt about what to discuss, start by exploring their answers to those final PHI questions.
- It can help to develop your own style, or pattern, with reviewing PHIs. For the PHI, here is an example of three steps you can follow.
- Glance at the Vitality Signs, noting whether mental health or physical health seems to be a higher priority. How do they feel in general about the life they live? If these are rated particularly low, ask them about it right away. Assess suicide risk.
- Move on to the numbers relating to “Where you are and where you want to be.” While it is important not to become overly focused on the numbers and lose track of the rest of the information on the PHI, it can help to see where there are the biggest gaps between a person’s “Present” and “Desired” states. The areas with the biggest differences might be the best ones to ask about first. (Or perhaps it works best to mention the higher ratings first and go from there—you decide.)
- Always review the initial “What really matters to me” question on the first page and the “Reflections” section at the end. Answers to these questions provide an excellent starting point for co-creating the PHP with someone. Again, having these questions answered in advance helps Veterans focus and can save your team time.
Creating a Personal Health Plan: Tips on How to Empower and Equip
Creating a PHP is a little like matchmaking. In order to do it, you need to know patients well—including, of course, why their health is important them. You also need to know your site well. That is, what VA and community resources can you share, and who can you recommend they see for additional support? What will follow up look like? If you are going to recommend a less conventional therapy (e.g., a CIH approach), what do you know about its safety and efficacy?
Here are 12 tips to consider when you are figuring out how to create a PHP to equip a Veteran:
- Whole Health care is a team effort. During Whole Health courses, when clinicians are first learning about how to do Whole Health visits, they often become quite concerned about having the time to incorporate this model with everything else they must do when they are seeing a Veteran. Each individual can have a huge impact on a given Veteran’s Whole Health care, regardless of how many others around them are actively using a Whole Health approach. Ideally though, especially in a Whole Health System, everyone on the care team must take ownership of advancing the PHP. The PHP is not something simply discussed in a single visit with a primary care provider, or during a conversation with a hospital discharge planner. Entire Patient Aligned Care Teams (PACTs), inpatient care teams, and others must share responsibility for Whole Health care; in other words, care must be transdisciplinary. Everyone who contributes to the care of Veterans should become comfortable discussing MAP, whether they are a mental health professional, a Whole Health Coach, a dietitian, a pharmacist, a chaplain, a nurse, a Whole Health Partner, a physician, or any other team member.
- PHPs come in all shapes and sizes. Sometimes, simply listening and offering compassion is sufficient to promote Whole Health. Sometimes a plan may be just one shared and/or SMART goal. Other plans may be more detailed and cover multiple aspects of the Circle of Health. Be careful not to overwhelm Veterans with too many suggestions at once. Ask them how much they can handle and make good use of follow-ups with various team members so that the plan can keep evolving.
- Your first order of business is to synthesize all the information at your disposal. This includes what you can learn from the medical record, the physical exam (if that is in your wheelhouse), and diagnostic testing, as well as their body language and what family members or friends tell you. It also draws in the information from the PHI, if they have completed one. What do your instincts tell you about the Veteran and what will serve him or her the best?
- The Veteran, as much as possible, should be a co-author of the plan. It should NEVER feel as though you are writing the plan by yourself. Have the entire team contribute, if possible. You do not have to go it alone. The Veteran should be the lead author.
- Follow up is ALWAYS part of the plan. The patient should always leave the room with a clear sense of next steps as far as follow up visits, procedures, etc.
- Be aware of contextual errors.[58] That is, don’t forget about a patient’s social context and how it could affect their care. As clinicians, we are trained to follow guidelines and use decision aids, but you have to make sure the PHP takes into account the specifics of a person’s life. Can they afford the medications being prescribed or the dietary supplements being recommended? Do they have responsibilities to others that make it so they cannot be in a hospital or nursing home? Do they have transportation to the consultant you want them to see? Are they comfortable trying a new CIH approach? Be mindful of cultural concerns as well, remembering that just because a person belongs to a particular culture does not mean you automatically know who they are or what they believe. In the spirit of cultural humility, ask them how their culture influences their care preferences regarding their health care.[59]
- It can help to follow a PHP template. There is now a national template available in the VA electronic medical record (CPRS). Refer to the CPRS Personal Health Plan Template Educational Overview for more information.
- Have tools and educational materials on hand to help with education and skill-building. This saves time, and it helps patients understand the elements of the PHP more fully. For example, it may be helpful to have printed copies of the Veterans Whole Health Education Handouts.
- Similarly, become familiar with various resources you can recommend in a health plan. These might include classes available through your site’s Well-Being Program, mindfulness training, shared medical appointment opportunities, local CIH practitioners, mental health offerings, Whole Health Coaches and Whole Health Partners who can be helpful, recreational therapy options, building vocational skills, or any of a number of other approaches specific to your local VA facility or community.
- ALWAYS take some time, even if it is brief, to focus on the positives. Note what they are doing right. Help them identify their assets. Weave their strengths into the plan too.
- One of the best ways to learn how to equip a Veteran for Whole Health is to try this for yourself. Research indicates you will be rated as much more believable if you model healthy behaviors and, as appropriate, briefly share you own health experiences with patients.[60]
- Compare notes with your colleagues. What do your colleagues include in their Veterans’ health plans? What are some of their favorite resources related to various parts of the Circle of Health? What techniques work best for them during a visit? How do they stay on time on a busy day? Ask people from your team, your site, and beyond. Invoke the wisdom of the group.
Concerns About Time
Clinicians often raise concerns about having enough time to use the Whole Health approach. However, most people who have adopted it report at least one of the following:
- It saves time, after you have practiced it. Initially, individual clinicians who started incorporating elements of Whole Health Clinical Care report spending an extra several minutes per visit when they incorporated Whole Health into the mix. Over time, the process becomes more efficient. For each patient, it is mainly an investment up front. Once you know a person fairly well, future conversations are actually easier, because their PHI has already been reviewed and they have already outlined their MAP. You do not have to have them start the process from scratch every time you see them. Remember that not all aspects of Whole Health have to be addressed at every visit, and in general, MAP and shared goals may not change for some time.
- It is more rewarding, so it is worth the time investment.
- You can tailor how much time you spend based on the specific situation. An inpatient stay is a great opportunity to focus on Whole Health in great detail. In contrast, during a busy clinic day, you may only have a minute or two, but you can still ask about someone’s priorities, garner a piece of their story, suggest a referral or patient handout, or create one simple SMART goal they can focus on. And it is important to remember that your presence, in and of itself, can promote Whole Health. This is true because of who you are and how you relate to other people (your therapeutic presence), not just because of the plans you create.
Goal Setting Revisited: Shared Goals and SMART Goals
Chapter 2 discussed the link between Mapping to the MAP and setting shared goals. As Veterans elaborate on their MAP and what will help them to achieve it, their goals will likely become more specific. You can use the PHI to understand a Veteran’s priorities and areas of motivation. This will be helpful in setting a shared goal together.
Shared goals, as described in Chapter 2, come first. Care professionals are sought out by patients because of their expertise; patients expect them to offer guidance and insight. Shared goals arise as clinicians and Veterans share their ideas and intentions with one another. Care team members may make statements such as:
- “You want to do [insert a goal here]. I want to support you with that.”
- “So, our goal is [insert goal here]. Let’s talk about how to do that together.”
- More specific: “I know you are concerned about lowering your dose of pain medications, and I also know you want to be able to keep doing what you enjoy, like walking outside with your wife and dog. I want you to be able to do that to. Let’s talk about how we might make it happen together.”
- Also, more specific: “My goal is to see your cholesterol lab values improve, and your goal is to be able to march with your marching band in the Veteran’s Day parade. What’s great is that we have the common goal of protecting your heart and boosting your activity level. Let’s come up with a plan where you can work on one specific thing that will help both of our goals be achieved.”</;li>
When planning how to achieve shared goals, SMART goals can be important. Some clinicians find that setting one SMART goal during a visit suits their patients well, while others will set more than one if time allows (though it is important not to overwhelm people by setting too many). As noted above, you can equip people for Whole Health in multiple ways and SMART goals can be one important option to consider.
“SMART” stands for:
Specific
Measurable
Action-Oriented
Realistic
Timed
Building a clear “I will…” statement using these criteria for a SMART goal can increase the odds a goal will be successfully reached. Consider the difference between these two statements:
- Less SMART: “I will lose weight.”
- SMART: “I will eat at least two servings of vegetables each day, including a side salad with lunch and a vegetable with dinner. I will start this next Monday, and I will do it for a month before I check back in with my primary care team.”
The second goal offers specific details around how diet will change with diet changes that can be measured. It describes specific actions that realistically can be done. Timing, including both start times and when they will check back with the care team, is clear.
There are two “rulers” that can be helpful with goal setting. The first is the Importance Ruler, illustrated in Figure 3-1. Follow-through is only going to happen when people truly feel that doing something matters a lot to them. Encouraging people to talk about change, as is encouraged in Motivational Interviewing trainings, can be incredibly empowering.
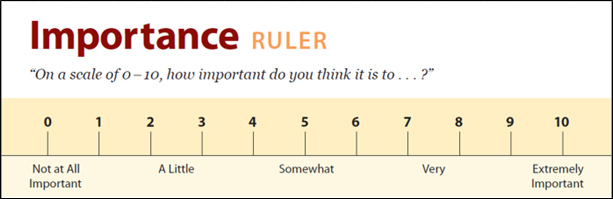
Figure 3-1. The Importance Ruler. Adapted from: Rollnick, Miller, Butler, Motivational Interviewing in Health Care, Guilford, 2008.
The second ruler to use, as appropriate, is the Confidence Ruler, illustrated in Figure 3-2. Part of being empowered as a patient is having confidence in your ability to reach your goals.
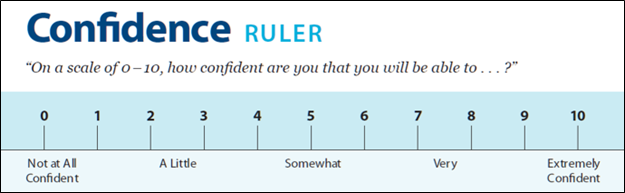
Figure 3-2. The Confidence Ruler. Adapted from: Rollnick, Miller, Butler, Motivational Interviewing in Health Care, Guilford, 2008.
Every time you set a goal with someone, pause to consider how they would assess its importance and how confidence they are they can reach it.
The following tool can be used to create a SMART goal with a Veteran. Consider writing some for yourself as practice...and follow through with them!
 Whole Health Tool: SMART Goal Setting
Whole Health Tool: SMART Goal Setting
Begin by focusing on a goal that is important to you. This goal should tie into what really matters. Once you have a goal in mind, apply the principles of SMART goals to it, as described in the table.
General Tips
- It is better to break a loftier goal down into smaller goals, in order to be sure you will succeed.
- The more detail the better. “I will exercise more” is very vague. “Starting on Monday, July 1, I will walk in the mall for 20 minutes on Monday, Wednesday, and Friday” is more detailed and incorporates all of the SMART elements.
- Make sure both the clinician and the patient agree (at least to some degree) about the goal (SMART goals should also, ideally, be shared goals).
- Be sure to double check that you covered all the parts of a SMART goal.
|
SMART Goal Element |
Questions to Consider |
Your Notes |
|
Specific |
|
|
|
Measurable |
|
|
|
Action-Oriented |
|
|
|
Realistic |
|
|
|
Timed |
|
|
Write your goal below:
This exercise was adapted from: Rollnick, Miller, Butler, Motivational Interviewing in Health Care, New York: Guilford Press, 2008.
Integrate
With so many potential aspects of Whole Health care—the Fundamentals, Mapping to the MAP, Empowering and Equipping, setting goals, and creating PHPs—it is possible to lose track of the big picture. Of all the elements of Whole Health care, Integration is imperative; Whole Health care should include a wide array of options, but it should never seem piecemeal. In fact, it is critical to incorporate this important aspect of the Whole Health Clinical Care Journey right from the beginning, to ensure Whole Health can be sustainable and successful. There are many ways integration can occur, including the following:
- Integration of the all the elements in the Whole Health Clinical Care Journey. Every member of the team, including the patient, should be aware of Whole Health fundamentals, as described in Chapter 2. They need to know what Whole Health is about and can describe it to others. Beyond that, they must understand the importance of talking about MAP. Team members should know their own MAP and be able to discuss others’ as well. As MAP is elucidated, shared goals can be set, and the process of personal health planning moves forward. People are equipped through education, resources, skill-building, and support, not to mention routine follow up. These steps are revisited regularly over the course of a person’s life.
- Integration of team members. As was noted earlier, Whole Health is a team effort. It is ultimately the responsibility of each individual Veteran to be the captain of their own team; no one health care professional can be solely responsible for providing Whole Health care. Seamless integration, with excellent communication, collegiality, and mutual respect, is essential. Increasing numbers of site leaders are now supporting Whole Health implementation. Five key elements are essential for optimal team function[61]:
- Shared goals everyone can articulate
- Clear roles; everyone knows their function and responsibilities, and everyone feels accountable
- Mutual trust, with safety to admit errors, ask questions, and try new things
- Effective communication
- Measurable processes and outcomes, with frequent feedback
- Integration of a variety of perspectives on how to approach care. This is the essence of “Integrative Medicine.” CIH, mind-body approaches, preventive strategies, medications, surgical procedures, and any number of other options can be appropriate components of Whole Health care. They should be integrated in a way that respects research findings and safety. There is also a respectful integration of previously developed VA projects and programs.
- Integration of all the elements of a Whole Health System. Chapter 1 describes the three essential elements of a Whole Health System—the Whole Health Pathway, Well-Being Programs, and Whole Health Clinical Care. Veterans ideally should move easily from one area to another. For example, a Veteran may discuss MAP with a Whole Health Coach. They may then take a Taking Charge of My Life and Health course taught by a Whole Health Partner and use what they learn to set shared (and SMART) goals. Those goals might include something like a meditation class offered at their site’s Well-Being Program, or a specific area they want to discuss with their clinical care team, such as optimizing nutrition or doing all they can to prevent heart disease. There should be good communication between the Coach, the Partner, the meditation teacher, the primary care team, and everyone else on the team, including the Veteran.
- Integration of what is needed for logistical success. The VA, like all health care institutions, is bureaucratic. To succeed, all the different parts of the system need to work together. For example, in the ideal Whole Health setting:
- Billing and coding have been updated to allow for CIH and other well-being offerings in VA.
- Community offerings and partnerships are seamlessly woven in.
- Online, etted resources are available.
- TeleWholeHealth experiences are offered with increasing frequency.
- A PHP template is available. There is now a Personal Health Plan Template in CPRS (refer to the CPRS Personal Health Plan Template Educational Overview). Templates can be a powerful tool for integrating all the different elements of Whole Health care.
- The Whole Health for Life smartphone application (app) is being offered by the OPCC&CT as a tool for to help users explore want for their health and why. It can be used independently or with a Whole Health Partner or Coach. It guides the user through the PHI, lets them select a component on the Circle, and offers videos about the component of the Circle they choose. It then helps them create a SMART goal and action step(s) to achieve it. The app creates a PHI summary where the user can monitor their progress. The Whole Health for Life app will be released in 2020 in VA and commercial app stores.
- Metrics are used, in a supportive and helpful way, to ensure that Whole Health is truly taking shape throughout facilities.
- Whole Health is successfully interwoven with Employee Whole Health (which is true nationally, now that they both fall under the OPCC&CT).
- Whole Health materials can be obtained through the purchasing department.
- Whole Health team members can be hired easily.
- The entire leadership structure of a site is supportive of Whole Health.
 Whole Health Tool: Personal Health Plan (PHP)
Whole Health Tool: Personal Health Plan (PHP)
This template was created to help Veterans and their care teams consider the full array of areas that can potentially contribute to Whole Health care. It is not necessary to cover every topic featured here; consider it a list of options.
Personal Health Plan for: _________________________________________________
Date: __________________________________________________________________________
Mission, Aspiration, Purpose (MAP):
What really matters to me…
My Long-Term Goals:
Strengths (what’s going right already)/Challenges:
MY PLAN FOR SKILL BUILDING AND SUPPORT
(Based on the Circle of Health)
Mindful Awareness:
Areas of Self-Care:
(You don’t necessarily need something for every category.)
Moving the Body
Surroundings
Personal Development
Food and Drink
Recharge
Family, Friends, and Co-Workers
Spirit and Soul
Power of the Mind
PROFESSIONAL CARE: CONVENTIONAL AND COMPLEMENTARY
Prevention/Screening
Treatment (e.g., conventional and complementary approaches, active medications, and supplements)
Referrals, Consults and Future Appointments
Shared Goals
Community & Resources:
(groups, classes and organizations that can support me)
My Support Team:
(people who can support me)
Next Steps (Follow Up):
Please Note: This plan is for my personal use and does not comprise my complete medical or pharmacological data, nor does it replace my medical record.
 Whole Health Tool: How Do You Integrate This Into Your Work?
Whole Health Tool: How Do You Integrate This Into Your Work?
Take a moment to envision how, based on all you have been learning, you want your Whole Health practice to look. Consider each of the questions below, and jot down answers as you wish. If you do not have a “practice,” list qualities of where you would like to receive your own health care.
How can you support Whole Health in your particular role on the team?

Who is on your Whole Health dream team? Complementary Health providers? Community providers? Whole Health Coaches? Whole Health Partners?

Do you have any ways of doing assessment prior to Whole Health visits, using tools like the Personal Health Inventory? When are they completed?

What Whole Health resources will you use?

How do you weave personal health planning into your typical care plans (e.g., into the visit summary)? AVS? Will you use a template? Will you create SMART goals?

What do you need to offer effective follow up? (Examples: specific resources, a directory of people you can refer to, fellow team members who will call and check in on their progress)

How will you document your Whole Health care visits?
What resources or support do you need to succeed?
Conclusion
This chapter focused on Equipping Veterans, Personal Health Planning, and how to Integrate all the different aspects of Whole Health Clinical Care. In Whole Health Clinical Care, Veterans are encouraged to take gradual steps as they move toward their MAP, and care team members can support them every step of the way. Make use of all the tools at your disposal—courses for VA staff and Veterans, TeleWholeHealth, PHIs, SMART goals, and PHP templates. Most importantly, be resourceful; tailor the plan to each individual’s needs. And be sure to integrate this into your own life too. You, as a caregiver, should also feel empowered and equipped, both to support Veterans and to take care of yourself.
One way to continue building your skills is to read on. The remainder of this reference manual focuses on the various components of the Circle of Health.
Resources for Writing Plans, Skill Building, and Support
Websites
VA Whole Health and Related Sites
- Personal Health Inventory Booklet. The most detailed version of the PHI. https://www.va.gov/WHOLEHEALTH/docs/10-773_PHI_May2020.pdf
- PHI (brief version). Online, fillable version of the PHI.
- https://www.va.gov/wholehealth/docs/10-930_PHI-Short_July2019_508.pdf
- An Intro on Mindfulness and Using the Personal Health Inventory. Podcast. https://www.va.gov/WHOLEHEALTH/phi.asp
- The Power of You. A video focused on how each clinician can bring Whole Health into a visit through his/her therapeutic presence. http://link.brightcove.com/services/player/bcpid4521574267001?bckey=AQ~~,AAACmABW4_k~,u3UC4vmaozkRbnTOHzovpplgn0QYiIND&bctid=4527187306001
- Whole Health: Personal Health Planning. Introduces the basics of creating a PHP.
- http://link.brightcove.com/services/player/bcpid4521574267001?bckey=AQ~~,AAACmABW4_k~,u3UC4vmaozkRbnTOHzovpplgn0QYiIND&bctid=4527056491001.
- Veterans Whole Health Education Handouts
- https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
- Change Management Resources
- VHA National Center for Organization Development Smart Change Toolkit. https://vaww.vashare.vha.va.gov/sites/NCOD/SitePages/SmartChange/SmartChangeHome.aspx
- Prosci Change Management. Prosci is contracted with VA to provide Change Management education/training. https://www.prosci.com
- MyHealtheVet. Has excellent resources anyone (Veterans and clinicians) can use to take stock of their health in many areas. Try calculating your “Health Age.” https://www.myhealth.va.gov/mhv-portal-web/home
- National Center for Health Promotion and Disease Prevention. Has resources that can assist with taking stock and doing Whole Health assessment. https://www.prevention.va.gov.
- My Life, My Story Program. Video of Veterans’ narratives. https://www.youtube.com/watch?v=fpzgVlExS20&feature=youtu.be
- TeleWholeHealth (TWH) Resources
- TWH Resources. You can find multiple resources to support TWH implementation, including a Telehealth Operation Manual, the TWH Supplement, and the Telehealth Training Calendar. https://telehealth.va.gov/type/clinic
- TMS TWH Training. For providers and Whole Health Staff. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/index.asp
- VA Video Connect. http://vaww.telehealth.va.gov/pgm/vvc/index.asp
- VA Video Connect for Providers. http://vaww.telehealth.va.gov/pgm/vvc/providers/index.asp
- Integrative Health Coordinating Center (IHCC). https://www.va.gov/WHOLEHEALTH/professional-resources/IHCC.asp
- Personal Health Plan (PHP) Template FAQs.
- https://vaww.va.gov/PATIENTCENTEREDCARE/FAQ_Personal-Health-Plan-Template.asp
- FIT Sharepoint Page. https://dvagov.sharepoint.com/sites/VHAOPCC/SitePages/FIT-programs.aspx
- Field Implementation Team (FIT) site visits.
- https://vaww.va.gov/patientcenteredcare/Field_Implementation_Program.asp
- CPRS Personal Health Plan Template Educational Overview. https://dvagov.sharepoint.com/:w:/r/sites/VHAOPCC/_layouts/15/Doc.aspx?sourcedoc=%7B187F7E02-62A3-44A4-9D9C-894C706DA474%7D&file=PHP%20template%20educational%20overview_5-7-2019.docx&action=default&mobileredirect=true
- TEACH. VHA National Center for Health Promotion and Disease Prevention (NCP). https://vaww.prevention.va.gov/VHEI/Teach.asp
Whole Health Library Website
- Implementing Whole Health in Your Practice, Part I: What a Whole Health Visit Looks Like. Overview. https://wholehealth.wisc.edu/overviews/part-i-what-whole-health-visit-looks-like/
- Implementing Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence. Overview. https://wholehealth.wisc.edu/overviews/part-ii-power-therapeutic-presence/
- All of the overviews contain patient narratives and have associated PHPs that may help you with ideas on what you can suggest/discuss in various situations.
- Reviewing Bob’s Personal Health Inventory Booklet, Bob’s PHI (brief version), and Bob’s PHI Booklet. Nice examples of how a completed PHI might look.
- https://wholehealth.wisc.edu/tools/reviewing-bobs-personal-health-inventory-booklet/
- https://wholehealth.wiscweb.wisc.edu/wp-content/uploads/sites/414/2019/06/M2-T-Bobs-Brief-PHI-2019.pdf
- https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2019/08/Bobs-Personal-Health-Inventory-Booklet.pdf
- Personal Health Inventory. Brief version. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/09/Personal-Health-Inventory-Brief.pdf
- Personal Health Inventory Booklet. https://www.va.gov/WHOLEHEALTH/docs/10-773_PHI_May2020.pdf
- Personal Health Plan Template. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/08/Brief-Personal-Health-Plan-Template.pdf
- Questions You Can Ask During a Whole Health Visit. https://wholehealth.wisc.edu/tools/questions-whole-health-visit/
- The Circle of Health: A Brief Self-Assessment. https://wholehealth.wisc.edu/tools/the-circle-of-health-a-brief-self-assessment/
- Whole Health and the Life of a Clinician.
- https://wholehealth.wisc.edu/tools/whole-health-and-the-life-of-a-clinician/ li>Narrative Medicine. Puts the importance of story, and of really knowing someone, into context. https://wholehealth.wisc.edu/tools/narrative-medicine
- VHA Whole Health: Personal Health Planning Staff Guide.
- https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/09/VA-Whole-Health-Personalized-Health-Planning-Staff-Guide.pdf
- ABC Guide to the Circle of Health . Introductory material to give a patient at an initial Whole Health visit. https://wholehealth.wisc.edu/wp-content/uploads/sites/414/2018/09/ABC-Guide-to-the-Circle.pdf
- Whole Health for Skill Building. One course for the eight self-care areas of the Circle of Health. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- Taking Charge of My Life and Health—Facilitator Training.
- https://wholehealth.wisc.edu/courses/whole-health-facilitated-groups/
- Whole Health Clinical Care Symposium. This course, piloted in 2020, is designed to help sites set aims and then use change management to implement Whole Health Clinical Care at their sites.
- https://wholehealth.wisc.edu/courses/whole-health-clinical-care-symposium/
Books
- Listening for What Matters: Avoiding Contextual Errors in Health Care, Saul Weiner (2016)
- Narrative Medicine: Honoring the Stories of Illness, Rita Charon (2008)
- Spontaneous Healing: How to Discover and Embrace Your Body’s Natural Ability to Heal Itself, Andrew Weil (2000)
- The 12 Stages of Healing, Donald Epstein (1994)



































