Tapering
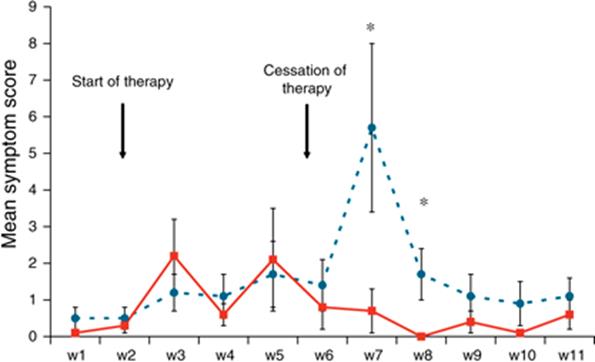
For patients who have made positive lifestyle changes and are less likely to need continued chronic acid suppression, it can still be difficult to come off PPIs. They often cause rebound hyperacidity, even if the underlying condition has resolved.[1] This occurs due to the lower stomach acidity increasing gastrin secretion, which causes the enterochromaffin cells to hypertrophy. When the PPI is suddenly discontinued, these larger cells have an increased capacity for acid secretion.[2] Figure 1 shows symptoms scores for dyspepsia in asymptomatic people given 40 milligrams of pantoprazole for 6 weeks versus controls. Despite being initially asymptomatic, they experienced rebound dyspepsia that lasted 10-14 days.[1]
When counseling about discontinuing a PPI, let patients know that they will likely have symptoms of reflux for about 2 weeks after they stop the medication. Fortunately, there are strategies to help calm reflux symptoms until rebound hyperacidity resolves.
Bridge Therapy
The following therapies will not only increase success for discontinuing a PPI but also are therapeutic for gastroesophageal reflux disease (GERD).
- Focus on nutrition. Common foods that should be avoided in those with GERD include alcohol, caffeine (coffee), chocolate, cow’s milk, animal fat, and orange juice.
- Slowly taper off the PPI over 2-4 weeks (the higher the dose, the longer the taper).
- While the taper is being completed, use the following for bridge therapy to reduce the symptoms of rebound hyperacidity.
- Encourage regular aerobic exercise.
- Encourage a relaxation technique such as deep breathing. This enhances vagal stimulation, encouraging digestion, and aids adequate peristalsis. or more information, refer to “Power of the Mind” and “Mindful Awareness” Whole Health overviews.
- Consider acupuncture 1-2 times per week.[3]
- Add one or more of the following dietary supplements:
- Deglycyrrhizinated licorice (DGL), 2-4 380 mg tablets before meals or sucralfate (Carafate) 1 gm before meals
- Slippery elm, 1-2 tbsp of powdered root in water or 400-500 mg capsules or 5 mL of a tincture three to four times daily.
- A combination botanical product, Iberogast 1 ml three times daily.[4]
- If the patient is successful with stopping the PPI, slowly taper off the above (except for positive nutritional changes, exercise, and stress management). If symptoms return, start again with one of the above or an H2 blocker (e.g., Ranitidine, 150 mg twice daily or as needed). If symptoms are still difficult to control, consider adding the PPI back at the lowest effective dose. Note: PPIs shut off all three acid pumps and H2 blockers are partial inhibitors of acid secretion. If long-term treatment is needed, H2 blockers allow better absorption of nutrients than PPIs and so potentially have fewer long-term adverse effects.
- For those with reflux hypersensitivity (those with normal endoscopies, normal pH monitoring/physiologic reflux, no esophageal motor disorder), consider an SSRI as first-line and an SNRI or tricylic anti-depressant as second-line. Patients with this condition are also more likely to have co-morbid behavioral disorders.[2]
- It would be most beneficial to avoid long-term acid suppression if possible since this is associated with malabsorption of vitamin B12[5] and iron,[6] increased risk of community-acquired pneumonia,[7] hip[8][9] and spine[10][11] fractures, diff diarrhea[6][12], and gastric cancer if a long-term PPI is used post H.pylori eradication therapy. [13] Early research has also suggested an association between chronic PPI use and dementia, which may be due to increases in amyloid plaque deposition.[14][15] Finally, PPIs have been associated with higher rates of acute interstitial nephritis and end-stage renal disease, so it may be prudent to wean off of them in patients at risk for chronic kidney disease progression.[15][16][17] For more details, refer to “Gastroesophageal Reflux Disease (GERD).”
Author(s)
“Coming Off a Proton Pump Inhibitor” was written by David Rakel, MD and updated by David Lessens, MD, MPH and Sagar Shah, MD. (2014, updated 2020). Sections were adapted from “Gastroesophageal Reflux Disease” by David Kiefer, MD, David Rakel, MD, and Rian Podein, MD.



















