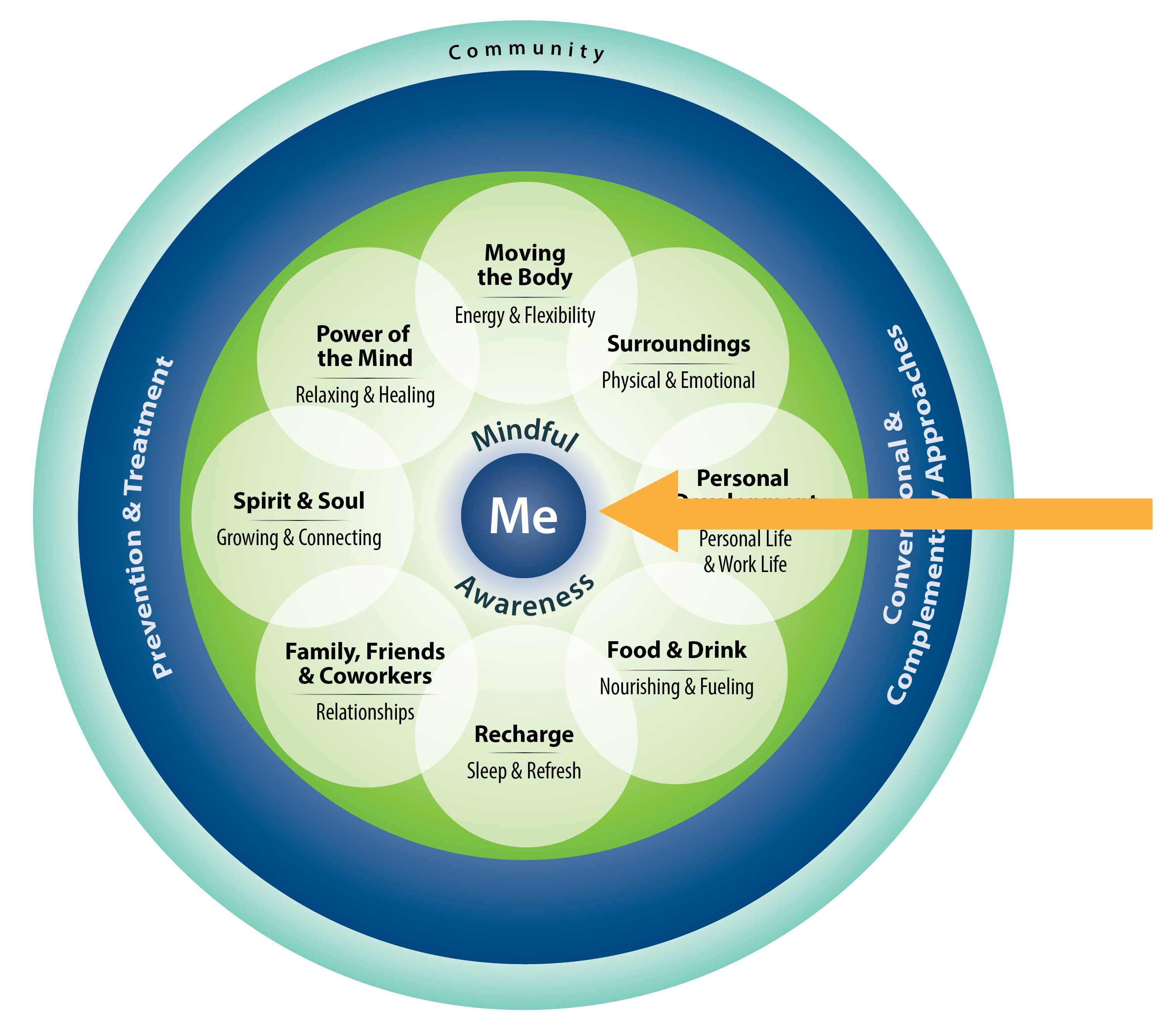
The Whole Health approach is built around the Circle of Health. “Me” is at the center, representing individualized, patient centered care. Immediately surrounding it is the “Mindful Awareness” circle, which bridges between Me and the rest of the circle, including the eight areas of self-care and the various aspects of professional care, not to mention community. To create a Personal Health Plan (PHP), people need to tune in; they need to be aware of their Mission, Aspiration, Purpose (MAP), as well as which areas of self-care they want to focus on. It is also important that they tune in to symptoms they are experiencing, as well as to what therapies or approaches they believe could be of benefit. Questions like the following (among many others) are essential to ask, in an open-minded, curious way:
- What really matters to me? Why do I want to be healthy in the first place?
- What are my symptoms telling me? What does my body need?
- How am I doing emotionally? How do I feel? What are healthy ways to help myself feel better?
- How is my thinking? Are my thought patterns healthy? Am I focusing too much on something? Are there things I need to think about that I am not paying attention to?
- How well am I able to live my life? What can help me function better from day to day?
- Who can help me be healthier? Are there treatments or tests or complementary approaches that I should look into?
- How can my community support me? How much would I like to be involved with different groups or organizations?
This overview defines mindful awareness and provides a number of examples of how people can bring it into their lives. Some practices are informal; that is you bring full attention to a typical daily activity, like doing laundry or petting your dog. Others are more formal. These practices, such as doing a seated meditation, are done for the specific purpose of building capacity for mindfulness. This overview also focuses in on the latest research on mindful awareness, including its effects on physiology, well-being, mental health problems, and various other health conditions. This overview builds on the materials in Chapter 4 of the Passport to Whole Health.
Key Points
- Mindful awareness involves focusing on the present moment, noticing what is happening without judgment.
- It takes practice to cultivate mindful awareness.
- Cultivating awareness helps people have a better sense of really matters, of their Mission, Aspiration, Purpose (MAP). It allows them to tune in to how their body is doing. It allows for more insights when it comes to creating a Personal Health Plan (PHP). It changes our brains.
- Mindful awareness can be cultivated in many ways. Meditation can have many goals, and for some types of meditation, mindfulness is a priority. Ultimately, the goal is to have mindful awareness be a state of mind that is present throughout our daily lives.
- While mindful awareness should not be viewed so much as a therapeutic tool as a way of life, it has been to have many different benefits. For example, it improves immune function, helps people with pain, reduces stress, decreases clinician burnout, and enhances a sense of well-being. It reduces depression and posttraumatic stress symptoms.
- There are many ways to bring mindful awareness more fully into your work as a clinician.
Meet the Veteran
Peace: It does not mean to be in a place where there is no trouble, no noise, or hard work. It means to be in the midst of all those things and still be calm in your heart. -Unknown

Linda is a 51-year-old nurse at the VA Medical Center. She is proud of her 27 years of service to the Veterans in her area, but it is becoming increasingly challenging to connect with her patients. She is frustrated with how often she sees the same patients in the hospital, always with the same, recurrent problems. They just do not seem interested in taking charge of their health. Additionally, the doctors are getting younger and younger, and it feels like they fail to see the value of her wisdom and experience.
Linda is not able to tolerate being on her feet for a twelve-hour shift like she once could. Low back pain often leaves her miserable by the end of her shift. She feels “scattered and irritable” a lot of the time. She is having trouble finding a sense of meaning and purpose in her work. That, combined with the pain, is taking a toll on her mood and her sleep. She does not think she can continue working given all of her frustrations and the negative effect her pain has on her ability to focus, but her allegiance to the VA leaves her feeling torn. During her visit with you today, she is tearful for most of the time. “What do you think I should do?” she asks.
As you review her chart, you note that she is regularly seeing a counselor, and she was not thought to meet criteria for depression. On Linda’s Personal Health Inventory (PHI), you are particularly struck by a few of her answers.
On her Vitality Signs, she rates herself quite low on all 3 areas.
When you ask her about this, she tells you it is the combination of the back pain and the burnout at work. She can get by, but she just does not know why she should keep putting in the effort. She does not like how negative she is becoming.
Within the self-care parts of the circle, she most wants to work with Power of the Mind, where she rated herself with a 2 out of 5.
When you ask her why this is a 2 and not a 1, she says she still enjoys her patients, at least a little. She also has hope that she can do something about this. This is reflected in her answer to the first “Reflections” question at the end of the PHI.
This overview focuses on how mindful awareness may be helpful to people like Linda. As you make your way through it, consider the following:
- Linda’s distress is multifactorial. How might mindful awareness fit into her PHP as a way of addressing multiple issues she is facing?
- What exercises or practices could you share with Linda to help get her started with cultivating mindful awareness?
- How do you feel reading/discussing Linda’s story? Do you have patients like her? Have you experienced any of the same issues?
Introduction
What is Mindful Awareness?
Mindfulness is paying attending in a particular way: on purpose, in the present moment, and nonjudgmentally.[1]
When you visit the Circle of Health for the first time (Figure 1), you might be struck by the central location of the light blue Mindful Awareness circle. It completely enfolds the “Me” (the patient) in the center circle.
Just as it is central to the Circle of Health, mindful awareness is central to the Whole Health approach to care. It is a lens that can be used to view all of the other parts of the circle.
As noted in the informational material in the Personal Health Inventory:
Mindfulness is being fully aware, or paying attention. Sometimes, we go through our daily lives on autopilot. We are not fully aware of the present. We often dwell on the past and plan events in the future. We do not spend much time really paying attention and noticing what is happening right now, without judging or trying to fix it. Your body and mind send you signals constantly. If your attention is elsewhere, you don’t notice. Then, the signals that began as whispers become loud warnings.
For example, when you miss the whispers of an early discomfort or a sad feeling, you miss the opportunity to make a change before it grows into real pain or depression. Being mindful, or aware, allows you to make conscious proactive choices about every aspect of your health. Mindfulness connects you to each component of your well-being, and to your whole self.
Mindful awareness involves attending to relevant aspects of experience in an open and accepting manner.[1] Mindful awareness practice is predicated on the following assumptions:
- Focusing on the present moment is fundamental.
Typically we do not focus our attention on our moment-to-moment experience. Instead, we operate on “auto-pilot” while our attention is focused on preoccupations with the past or future.
- Practice is needed.
With regular practice, over time, we can develop the capacity to sustain moment-to-moment non-judgmental awareness.
- Mindful awareness improves quality of life.
Moment-to-moment awareness enhances our living experience as we more fully attend and embody the discrete moments of our lives.
- Mindful awareness helps us to truly see.
Sustained, non-judgmental observation of our experience helps us see things as they really are, dispelling the fog of false perception.
- Mindful awareness allows us to be more skillful with our thoughts.
Enhanced accuracy of perception interrupts established automatic patterns of thought and behavior, allowing us to more effectively navigate the world with a greater sense of self-determination.[2]
Mindful awareness practices have conceptual roots in the Buddhist tradition, where they have been used for thousands of years to cultivate compassion and relieve suffering.
In contemporary use, mindful awareness is usually taught as a non-religious practice of self-observation and attention to the present moment. Most people find that this is compatible with their religious beliefs, since special care is taken at most hospital- and clinic-based training programs to keep them neutral in this regard.[3]
– John Kabat-Zinn
A distinction is often made between formal and informal mindful awareness practices. Formal practice involves coursework or specific time set aside to work with mindfulness techniques. (For more information about these techniques, which include various forms of meditation, refer to “Power of the Mind.”) Informal practice might be viewed more as the practice or mindful awareness that is with you every moment of the day.
A wide variety of courses that offer training in formal mindful awareness now exist, and they vary in terms of length and focus. Some people choose to learn mindful awareness practices in a class (which many people find preferable), while others spend time with audio resources, such as MP3s and CDs, to add to their experience. One common element for all the courses is that they emphasize the importance of regular practice. Many courses encourage learners to spend at least 40 minutes per day on exercises, though the optimal “dose” of such practices is still being explored through various research studies. Even 20 minutes daily can lead to dramatic improvements for people. Because practice tends to give rise to many questions, and because awareness of one’s thoughts can lead to concerns related to how to address the patterns that are observed, it is preferable to have an instructor versed with helping learners move through the training process.
Mindfulness-based interventions (MBIs) are interventions offered to facilitate practice and teaching. MBIs are now employed in a wide variety of clinical settings. Two influential examples of MBIs are:
Mindfulness-based stress reduction
Mindfulness-Based Stress Reduction (MBSR) is an eight-week program that was developed in 1979 by Jon Kabat-Zinn, PhD, at the University of Massachusetts Medical Center as an intervention for patients suffering with stress, chronic pain, and illness. This intervention uses meditation, mindful movement, group discussion, and home practice to develop mindful awareness skills.[2] These skills include, among many others:
- Living more fully in the present moment
- Cultivating mental ease and flexibility
- Practicing compassion toward self and others
- Working with challenging emotions and thought patterns
- Relating to one’s thoughts so as not to be overwhelmed by them
- Learning mindfulness techniques (including various forms of meditation) that can be practiced routinely
Mindfulness-based cognitive therapy
Mindfulness-Based Cognitive Therapy (MBCT) is a mindfulness-based mental health intervention originally designed for the treatment of recurrent depression.[3] It combines mindful awareness training with techniques used in Cognitive Behavioral Therapy (CBT). It teaches people to become aware of and disengage from mental patterns characterized by ruminative, negative thinking, with a shift toward new, more affirming and supportive, mental patterns.[4] A 2011 systematic review and meta-analysis found that it led to a 34% relative risk reduction in relapses of major depressive disorder.[5]
Both of these programs are widely employed in an array of clinical settings. Mindful awareness is the second-most commonly used complementary approach within the VA, according to the 2015 Healthcare Analysis Information Group (HAIG) Report.[6] 108 of the 131 sites (82%) surveyed for the report were offering mindfulness in some form (a variety of meditation strategies were included under the “Mindfulness” category). This is up from 57% in the 2011 HAIG Survey.[7]
Mindful Awareness Moment
When Have You Been Most Mindful?
Pause for a moment, and ask yourself the following:
- What circumstances allow you to be at a state of heightened awareness?
- When are you most present?
- When are you most peaceful, or calm?
- What makes you optimally focused?
- When are you at your most centered?
These questions are frequently posed to participants in the in-person Whole Health program. Some answers have included the following:
- When I am playing with my kids
- When I am “in the zone” playing a sport
- When I am in the operating room
- When I pray
- When I am lost in a good book or movie
- When I am gardening
- When I watch my dog
- When I play an instrument
What about the activities you listed that allows them to have such a positive effect on you? How can you bring those states of mind with you into other situations?
Why Does Mindful Awareness Matter?
It is important to emphasize that mindful awareness is an opportunity to be in the wholeness of life, including suffering, joy, peace, unrest, creativity, fullness, emptiness – all of it. It is not merely a technique for coping with a specific problem.
As will be discussed in greater detail momentarily, mindful awareness has been the subject of increasing focus in health care research. It brings about positive physiological, psychological, and clinical changes. These findings may help to guide the creation of health plans that incorporate MBIs.
An added benefit of mindful awareness is that it tends to be quite safe. Clinicians should be aware of a few provisos with this, however. First, mindful practices should be done with guidance and supervision from a skilled professional for people with severe mental health problems, and particularly if they have psychotic disorders or PTSD. Second, some people first practicing formal mindful awareness training will experience emotional distress as they come to be more aware of some of the patterns, emotions, thoughts, and behaviors that challenge them.
Incorporating Mindful Awareness into Daily Living
Mindfulness has to be experienced to be known. [8]
—Chris Germer
Usually our attention is scattered. We replay moments from the past; we savor, analyze, and edit them in our minds. We fantasize about the future, perseverating on our various hopes, fears, plans, and possible outcomes. Mindful awareness allows us to leave the world of our imaginings to fully inhabit the present moment. During mindful awareness meditation practice, our full attention is focused on the “here and now.” Mindful awareness implicitly asks the question, “What am I experiencing right now?” To cultivate mindful awareness, we continually consider this question without judgment of the answer. In this way, we maintain moment-to-moment awareness. This offers us a more complete and satisfying experience of the succession of moments that makes up our lives.
With time, mindful awareness practice evolves into a way of being
Diligent observation of the moment-to-moment mental content initially can feel effortful and even cumbersome. However, with practice, moment-to-moment nonjudgmental awareness comes more easily and naturally. Earlier, formal and informal mindful awareness practices were discussed. The goal of mindful awareness meditation practice (formal practice) is to become established in a continually mindful state (ongoing informal practice). Paradoxically, however, striving toward this goal is counterproductive. Mindful awareness is actually a process of non-striving, of being with what is.
Mindful Awareness Moment
An Introductory Breath Awareness Practice
To understand the difference between mindful awareness and our typical state of inattention and distraction, try the following experiment. Sit comfortably with the feet planted firmly on the floor. Lengthen through your back, neck, and the top of your head. Now, for the next two minutes, turn all of your awareness to your breathing. Without changing the rate or quality of your breathing, simply note the sensation of inhalation, the sensation of exhalation, and the pauses between these two dynamic states.
Now reflect:
- How easy was it to focus your attention on your breathing for two straight minutes?
- What distracting thoughts arose?
- What judgments or evaluations pulled your awareness away from your breathing?
Take two additional minutes to repeat the exercise above. This time, when your thoughts wander away from the breath, gently return your attention to your breathing. Judgments may arise – “I can’t concentrate,” or “This is boring.” When this happens, simply notice that this is a thought, and bring your attention back to your breathing. When your mind wanders, be gentle with yourself. Notice if you scold yourself for deviating from the breath, accept the passing distraction, and refocus your attention on the breath.
Now reflect again:
- How did it feel taking an additional two minutes to focus on the breath?
- How easy was it to maintain your attention on the breath?
- What distracting thoughts and judgments arose?
- How easy or difficult was it to gently bring your awareness back to your breathing?
- How do you feel at the end of the exercise?
If you found it challenging to maintain present-moment awareness of the breath during the last exercise, take heart; the body is a constant ally in remaining grounded in the here and now. Your body feeds you constant updates about your experience of the present moment. Observe your breathing. Note the feeling of your feet on the floor. What signals are arising from your body – hunger, thirst, fatigue, discomfort, elimination cues? What are you seeing, hearing, smelling, tasting, touching? In bringing the awareness to these ongoing status indicators, we are able to maintain presence in the current moment.
Unexamined entanglement in our thoughts disconnects us from our anchors in the present moment
As you experienced in the exercise above, our full attention to the present moment is almost constantly challenged by our meandering thoughts. Regrets, to-do lists, fantasies, and frustrations sweep us up on currents of emotion and distract us from our experience of the present. We find ourselves lost in thought, absorbed in reverie, caught up in a narrative of our own construction. The thoughts are not in themselves problematic, but our tendency to become engrossed in our thoughts disconnects us from the present moment. This is the web of mental entanglement that impedes our ability to perceive things as they really are.
We observe our thoughts to maintain awareness of our anchors in the present moment
Mindful awareness training incorporates the systematic observation of our thoughts. In observing our thoughts, we are able to gently redirect our attention to the present moment and avoid getting caught up in our imaginings. We do not judge our thoughts as they arise. We simply acknowledge thoughts in the form of “okay,” or “noted,” before bringing our awareness back to the question of “What am I experiencing right now?” This facilitates our full engagement in the current situation as it truly is, and allows us to employ our full cadre of internal resources.
Mindful Awareness Moment
Metacognition
Metacognition is, put simply, the mind being aware of how it works. It can be likened to a state of mind you can attain while watching a movie. If cognition – or your usual thinking patterns – are the equivalent of being lost in the movie, to the point where you feel like it is your reality, then metacognition is akin to moving out of that state, into an awareness that you are in the theater, sitting in your seat, caught up in a movie that does not necessarily represent your reality. After you experience that broader awareness, you then have the opportunity to choose whether or not to escape back into the movie. The key is that you now consciously have chosen to do so.
Take a moment to explore this more right now. What is going on around you as you read this material? What other thoughts have been intruding? How has your body been feeling? What is going on with you emotionally? What is the temperature of the room? What ambient sounds and smells surround you? How long has it been since you have taken a break, stood up from your chair, or rested your eyes?
Mindful awareness is, in part, about becoming more aware of your mind’s patterns. As you come to recognize those patterns, it can be extremely empowering, for then you can consciously choose to make changes.
Mindful Awareness Research
There is growing evidence that MBIs increase well-being in patients and clinicians.
As will be described in more detail below, studies and meta-analyses have demonstrated that MBSR and therapeutic approaches derived from it are effective in improving health status in many areas, including the following:
- Improving symptoms in those with psychiatric disorders, including those associated with major depressive disorder and various anxiety disorders
- Helping those with alcohol and substance misuse.
- Reducing pain and psychological distress in people suffering from chronic back pain, fibromyalgia, irritable bowel syndrome and other chronic conditions.
- Promoting wellbeing in healthy populations
Some highlights from the body of mindful awareness literature are presented here. This research focuses on formal mindful awareness practice, and various forms of mindfulness meditation have received the greatest attention.
Physiologic effects
Central nervous system effects
Electroencephalographic (EEG) and functional MRI data are beginning to show that mindfulness meditation changes both brain structure and function. For example, experienced meditators demonstrate greater power of alpha and theta waves on EEG, which are associated with relaxation states. Evidence suggests these relaxation states become more permanent conditions in experienced meditators.[9]
Additionally, attention and affective processes are more organized in long term practitioners of meditation, as evidenced by increased gamma oscillations on EEG. In a 2004 study, Lutz and colleagues demonstrated gamma oscillations in long term meditators with a higher level of synchronization than ever previously documented.[10]
Meditation has been linked to greater activation of the left anterior cerebral cortex, which is associated with positive mood and affect.[11] Functional MRI data demonstrate increased activation in attention centers and less cortical activity in response to distracting stimuli in experienced meditators, as compared to controls.[12]
Much attention is being given to the effects of mindful awareness on the experience of pain. Novice meditators may experience pain relief after only minimal training. This is associated with increased activation in cortical regions involved in the cognitive and emotional evaluation of pain and decreased activation of lower level sensory processing centers such as the thalamus. On the other hand, in experienced meditators, neuroimaging demonstrates increased activation in the thalamus and decreased activation of the prefrontal cortex, suggesting that experienced meditators experience sensations without superimposing an evaluative process on the sensory experience. Additionally, in response to the anticipation of a painful stimulus, more practiced meditators demonstrate smaller amplitude evoked potentials in brain centers associated with the expectation of a stimulus.[13]
Immune system effects
Interestingly, mindfulness training has been linked to enhanced immune system function.
Telomerase activity
Telomeres are protective segments of DNA at the end of chromosomes which preserve the integrity of the DNA and protect against cell death. Shortened telomeres are associated with poorer health outcomes and premature death in a variety of diseases.[14] Telomerases are enzymes that maintain the length of the telomeres, and higher telomerase activity in cells is associated with better immune system function.[15] Preliminary evidence suggests mindfulness practice is associated with increased telomerase activity.[15][16] In a 2014 meta-analysis which included 4 randomized controlled trials with a total of 190 participants, Schutte and Maulouff demonstrated a medium effect size of meditation on telomerase activity in peripheral blood mononuclear cells.
T lymphocytes
T lymphocytes are a type of immune system cell that fights infection and cancer.[16] In a 2016 systematic review, Black and colleagues found that in HIV and cancer patients, mindfulness meditation was associated with increased T lymphocyte numbers, attenuated declines in T lymphocyte numbers, or increased percentages of activated T lymphocytes as compared to controls. In a 2008 randomized controlled trial, Creswell and colleagues demonstrated stable CD4+ T lymphocyte counts in HIV infected individuals who completed an MSBR course, whereas controls showed significant declines in CD4+ T lymphocytes over the study period.[17]
Mental Health
Depression and anxiety
A 2010 meta-analysis showed large effect sizes for the treatment of affective symptoms in patients with primary depression and anxiety. In patients with depression and anxiety resulting from medical conditions, effect sizes were moderate. These results suggest mindful awareness practice is helpful for patients suffering depression and anxiety in a variety of clinical contexts.[18]
Teasdale and colleagues showed that the combination of MBCT and treatment as usual (TAU) for depression reduces by half the rate of depressive relapse as compared to TAU in people with multiple prior episodes of major depression.[2][19] A 2016 meta-analysis including data from 1258 subjects demonstrated a 0.69 hazard ratio for depression relapse in patients treated with MBCT as compared to controls over a 60 week follow-up period. The effect of MBCT for depression relapse prevention was less robust when compared to active controls (hazard ratio 0.79), though still significant.[20]
MBCT is as effective as maintenance antidepressants in preventing relapse of depression. In a well-designed trial, after completing MBCT, 75% of people with a history of major depression were able to discontinue antidepressant medications at 15-month follow-up.[21] These promising results were corroborated in a 2018 meta-analysis, where mindfulness interventions performed as well as other first-line evidence-based treatments for psychiatric disorders, including CBT and antidepressant therapies.[22] Further evidence suggests that the more severe the depression symptoms are, the greater the effect of MBCT as compared to other treatments.[20]
However, Goyal and colleagues in a comprehensive 2014 meta-analysis did not find a difference between mindfulness meditation and active controls for the treatment of psychiatric disorders.[23] They did find a moderate effect when mindfulness interventions were compared only to passive controls. Similar results were published in a 2018 meta-analysis; mindfulness interventions were superior to passive controls for the treatment of common mental disorders in the acute phase, however no difference was observed between mindfulness interventions and active controls.[24] In other words, benefits were not as great if the control group was offered something else to do, as compared to not doing anything differently and just waiting to take a mindfulness course.
PTSD
In a 2018 systematic review, Boyd and colleagues found that mindfulness based interventions were effective in reducing symptoms of PTSD, with medium to large within-group effect sizes.[25] Similarly in a 2017 meta-analysis, mindfulness based interventions were shown to be effective in reducing the symptoms of PTSD as compared to control conditions. More robust effect sizes were seen in comparison to passive controls.[26] In 2013 King and colleagues published data from a small controlled trial of MBCT for the treatment of combat-associated PTSD. In this study, combat Veterans with longstanding PTSD experienced moderate improvements in clinician-assessed and self-reported PTSD symptoms following a MBCT intervention as compared to Veterans in a TAU group.[27] In an open pilot study of MBSR taught to a heterogeneous group of Veterans at a VA facility, approximately three-fourths met symptom criteria for PTSD and two-thirds had a chronic pain diagnosis; attendance rates were high and improvements in measures of mental health and quality of life were seen over time.[28] In a small pilot randomized controlled trial (RCT), as compared to usual care, for Veterans with PTSD, MBSR participation was associated with enhanced functionality and reduced depressive symptoms, but not reductions in PTSD symptoms, for those who attended at least four MBSR classes.[29]
A telehealth mindfulness intervention has been developed for Veterans with PTSD. Telehealth mindfulness treatment involves 2 in-person sessions followed by 6 telehealth sessions (sessions that are conducted remotely). In a small pilot RCT, telehealth mindfulness treatment was associated with temporary reductions in PTSD symptoms as compared to psychoeducation. Satisfaction with the telehealth treatment approach appeared to be high.[30]
Substance Use Disorders
In a 2018 meta-analysis, Sancho and colleagues found that mindfulness-based interventions reduce dependence, cravings, and other addiction related symptoms in substance use disorders and behavioral addictions. The evidence was strongest for mindfulness-based interventions combined with treatment as usual. The most common mindfulness-based interventions studied were Mindfulness-Based Relapse Prevention (MBRP), mindfulness training for smokers (MTS), and Mindfulness-Oriented Recovery Enhancement (MORE).[31]
The authors of a 2016 systematic review concluded that MTS is as effective as the American Lung Association’s “Freedom From Smoking” program (standard of care) and can reasonably be recommended in conjunction with pharmacotherapy for smoking cessation. They further assert that mindfulness based relapse prevention is effective in improving health care related quality of life patients with substance use disorders when used in conjunction with treatment as usual. The authors caution that more studies are needed to determine the efficacy of MBRP for relapse prevention.[32]
Chronic Pain
In a 2017 meta-analysis of the effects of mindfulness meditation on chronic pain, pooled data from 30 trials (n=3536) revealed a small effect on chronic pain as compared to treatment as usual, psychoeducation and passive controls.[33] These results were corroborated in a 2018 meta-analysis wherein mindfulness meditation was superior to passive controls for chronic pain. In this analysis, mindfulness meditation was equivalent to active controls in the treatment of chronic pain conditions.[22]
Additionally, mindfulness meditation was associated with statistically significant improvement in depression, physical health-related quality of life, and mental health-related quality of life.[33] The benefits in quality of life may be attributable to increased pain acceptance and coping.[34]
In 2012, Ussher and colleagues studied the utility of a brief (10-minute) body scan for the management of chronic pain. The body scan is an exercise often employed in mindful awareness meditation. The brief body scan group had more significant findings than people in the control group, in terms of pre/post intervention measures of pain-related distress and social limitations related to pain. Interestingly, these improvements were not sustained when the intervention was repeated in the home.[35]
Chronic back pain
A 2016 RCT comparing mindfulness meditation, CBT, and usual care for the treatment of chronic low back pain in young to middle-aged adults showed that mindfulness was as effective as CBT for reducing pain and functional limitations. For both the MBSR and CBT groups, about 60% of participants experienced clinically meaningful improvement on “The Roland-Morris Low Back Pain and Disability Questionnaire” as compared to 44% of participants achieving this outcome in the treatment as usual group. This effect persisted at the one year follow-up for the MBSR group.[36] In a 2017 meta-analysis of 7 RCTs, Anheyer and colleagues demonstrated that compared with usual care, MBSR was associated with short-term improvements in pain intensity and physical functioning. There was no difference between MBSR and active controls. Additionally, it is uncertain if the improvements in pain intensity were clinically significant as they did not meet the threshold for the minimum clinically important difference.[37]
Fibromyalgia
The authors of a 2017 review article on mindfulness meditation for fibromyalgia symptoms concluded that mindfulness interventions focusing on acceptance, non-attachment, and social engagement in addition to nonjudgmental awareness appear to be most effective in improving fibromyalgia-related outcomes. They also produce improvements in depression, anxiety, anger, pain, fibromyalgia-related symptomology, stress, coping efficacy, and positive affect in comparison to wait-list and active controls.[13]
A 2017 RCT comparing mindfulness meditation to an active control found significant improvements in fibromyalgia symptomatology, pain perception, sleep quality, psychological distress, non-attachment, and civic engagement as compared to controls, and these improvements were maintained at 6 month follow-up.[38]
Irritable bowel syndrome
In a 2014 meta-analysis of 6 studies of mindfulness interventions for functional GI disorders (the most common being IBS), the mean decrease in symptom severity ranged from 23 to 42% for mindfulness based interventions with moderate pooled effects on IBS symptom severity and quality of life as compared to controls.[39] A study conducted in a Veteran population revealed significant improvements in IBS-related quality of life and gastrointestinal-specific anxiety over a 6-month period in those who participated in an MBSR program; those Veterans also showed a measurable increase in mindful awareness skills. The authors asserted the need for further studies to discern the relationship between mindful awareness education and gastrointestinal-specific anxiety and quality of life.[40]
Stress & inflammation
Mindfulness meditation reduces several physiologic markers of stress including cortisol, C – reactive protein, blood pressure, heart rate, triglycerides and tumor necrosis factor-alpha in a variety of populations.[41] Rosencranz and colleagues demonstrated both decreased stress hormones and decreased inflammatory response in a study of MBSR in healthy subjects. Subjects were randomized to either MBSR or a health enhancement program (active control). To induce stress, subjects participated in a public speaking exercise, a mental math exercise, and an inflammatory cream was applied to the forearm. These three events occurred at both the beginning and the end of the study. Subjects in the MBSR group and in the health enhancement program group showed decreased stress hormones in response to the stressful activities. Subjects completing MBSR also showed decreased skin inflammation in response to the application of the irritating cream.[42] These data suggest a potential benefit of mindful awareness training in the management of inflammatory conditions.
Decreased clinician burnout
A systematic review of 81 studies on the impact of mindfulness on the well-being of healthcare professionals demonstrated that mindfulness decreases health care provider burnout, anxiety, depression, stress, anger and distress.[43] In 2012, Goodman and Schorling published results from an eight-week MBSR adaptation specifically tailored to the needs of health care workers. A pre-post analysis of physician participants demonstrated improved indices of mental health, depersonalization, emotional exhaustion, and personal accomplishment.[44] Also encouraging are results from a 2009 study wherein primary care physicians enrolled in a twelve-month MBI showed improvements in the domains of mindful awareness, emotional exhaustion, depersonalization, perceived personal accomplishment, empathy, mood, and emotional stability. There was a correlation between improvements in mindful awareness and improvements in mood, burnout, conscientiousness, and emotional stability.[45]
In 2013, Fortney and colleagues published data from an abbreviated mindful awareness course for physicians conducted over a weekend with two follow-up evening sessions, rather than the typical eight-week MBSR course. Physicians in this study showed improvements in scores of burnout, stress, anxiety, and depression. Improvements were maintained nine months after the intervention ended.[46]
Improved care
It appears that mindful awareness in clinicians may influence both the quality of their care as well as patient satisfaction. Mindfulness interventions have been shown to enhance job performance specifically in the domains of compassion and empathy.[43] In 2013, Beach and colleagues studied physician self-perception with respect to mindful awareness.[47] Results indicate that physicians who rate themselves as more mindful are more likely to have patient centered visits (as opposed to physician-centered visits) when compared to their less mindful colleagues, as measured by the Roter Interaction Analysis System. Additionally, the patients of more mindful physicians rate physician communication and overall quality of care more highly than do patients of less mindful physicians. Mindful awareness can serve as a fundamental element of personalized, proactive, and patient-driven care.
Nonclinical populations
In the Mindful Student Study, exam-related stress scores were reduced for students who received additional mindfulness training.[49] On average, six students needed to be offered the MSS course to prevent one from experiencing clinical levels of distress. Mindful awareness has also been shown to benefit nonclinical populations, enhancing well-being, and decreasing stress and negative emotions in study participants outside of a medical treatment context.[48] In a 2018 RCT, university students who received a mindfulness intervention demonstrated significantly less distress during exams than did controls who received support as usual. Only 37% of students in the mindfulness group had distress scores above an accepted clinical threshold, as compared to 57% of the support as usual group.[49] Chiesa and Seretti in a 2009 review article examined the effects of MBSR on stress in healthy people and found that MBSR was beneficial. The included studies had mainly inactive control groups; however, MBSR also proved more effective in the mitigation of stress than an active control, suggesting a more specific effect. The authors also included a head to head trial of MBSR and relaxation training, and the two interventions performed equally well at reducing stress. Additionally, the authors reported a positive effect on spirituality in healthy study participants undergoing MBSR as compared to inactive controls. Furthermore, they included a head to head trial of MBSR versus an active intervention for spiritual development, and the two interventions performed equally well.[50] For an extensive discussion of spirituality and its relationship to health, please refer to the module entitled “Spirit and Soul.”
Mindful awareness meditation practice is a powerful tool in the maintenance and restoration of well-being. Current research demonstrates the power of mindful awareness practice to re-engineer the internal landscape for the promotion of health and happiness for patients finding living under a wide array of circumstances.
Quality of evidence
Despite the promising findings for both clinical and non-clinical populations, MBSR research—and mindful awareness research more generally—has been limited by a number of conceptual and methodological issues. Many of the quantitative studies employed small sample sizes and exhibited high drop-out rates. However, an increasing number of systematic reviews and meta-analyses are facilitating a more robust and nuanced understanding of the effects of mindfulness interventions. Many questions remain concerning the mechanisms through which mindful awareness training contributes to positive health related outcomes. Research initiatives with a combined focus upon process and outcome variables and diversified research methods (e.g. use of qualitative and physiological methods) are thus recommended. Finally, studies designed with broad cultural and conceptual sensitivity will lead to a rich understanding of the health benefits of MBSR and other MBIs.
Mindful Awareness: A Summary of Key Research Findings
General Findings
- Reduces psychological symptoms in people with chronic conditions including but not limited to low back pain, fibromyalgia, and IBS
- Prevents relapse of depression
- Assists with the treatment of alcohol and substance misuse
Physiologic Effects
- Alters brain activity. Long-term meditators have gamma wave oscillations not seen in others. Even people who have just begun meditating in the past 2 months show EEG and functional MRI changes.
- Leads to longer-lived relaxation states
- Activates the left anterior cerebral cortex, which is linked to positive mood. Increases activation in brain attention centers
Immune System Effects
- Protects cells from aging and death through enhanced telomerase activity
- Stabilizes or attenuates decline in CD4+ counts in people with HIV infection
- Enhances natural killer cell function and alters interleukin levels
Psychiatric Disorders
- Decreases depression and anxiety severity in general
- Reduces rumination in people with anxiety and depression
- Mindfulness-based cognitive therapy is as effective as medications for depression relapse prevention
- Attenuates symptoms of PTSD
Chronic Pain
- Improved pain intensity, pain acceptance, pain coping, and health care related quality of life
- Large improvement in many fibromyalgia symptoms
Other Findings
- Reduced IBS symptoms in a Veteran population
- Reduced clinician burnout
- Improves quality of care in clinician practitioners
Mnemonics For Mindful Awareness Practices
Tell me what you pay attention to, and I will tell you who you are. -Jose Ortega y Gasset
The dimensions of our moment-to-moment experience – TIES[51]
The TIES mnemonic is a useful framework for characterizing our moment-to-moment experience. It can be used to describe the internal landscape. TIES covers more or less everything that can come up for you as you practice mindful awareness:
- Talk/Thoughts: mental chatter, incessant thinking, storyline narratives
- Images: mental pictures, imagined scenes, visualized scenarios
- Emotional/Feelings: love, hate, lust, fear, joy, sadness, anxiety, jealousy, etc.
- Sensations: sound, touch, sight, taste, smell.
The process of engaging our moment-to-moment experience – SOLAR[51]
Building on the utility of the TIES mnemonic in characterizing experience, the SOLAR mnemonic is a useful framework for fully embodying our moment-to-moment experience. It can be used to observe the internal landscape.
- Stop: Take a moment to practice mindful awareness. This might be a specific time that you set aside on a routine basis, or it may be more spontaneous. Many clinicians will stop at key moments during their workday, such as prior to crossing a threshold into a clinic or hospital room, or as they are using their stethoscope.
- Observe: Pay attention, without judging, to what goes on during this time. Which elements of the TIES mnemonic (thoughts, images, emotions, sensations) come up? Just notice them.
- Let it be: Again, there is no striving, and there is no need to judge. If you catch yourself thinking about whether or not you are “good at this,” that too is just a thought that you can allow to pass by.
- And Return: Move back into what you were doing prior to stopping. Of course, you can repeat this process throughout your day.
Mindful Awareness Moment
Practicing with the SOLAR and TIES Mnemonics
This is an opportunity to practice the SOLAR steps you just learned. The TIES mnemonic is used during the “Observe” step.
Stop:
- Move to a quiet place where you won’t be disturbed.
- Set your phone or other alarm for five minutes, and then allow yourself to let go of time altogether.
- Sit comfortably in a posture of relaxed alertness.
- If in a chair, plant the feet squarely on the floor.
- If on a cushion, ideally the hips will be elevated above the level of the knees.
Ensure that both knees are amply supported by the floor, or by supportive props.
- Elongate the spine from the tailbone through the top of the head.
- Gently tuck the chin and lengthen through the back of the neck.
- Position your hands comfortably.
- Set an intention for your period of meditation. It may be as simple as “May I cultivate mindful awareness in my life,” or “May I enjoy the benefits of silence and stillness.”
Observe
- Focus your attention on the sensations in your body. Note the feeling of your hips on the chair (or cushion), your feet (or knees) grounded, and your posture erect and relaxed.
- Next, turn your attention to your breathing. Without manipulating the rate or quality of the breath, simply observe the sensations of inhaling and exhaling.
Now, on a moment-to-moment basis, observe what arises in your experience. Use the TIES mnemonic outlined above to inventory your experience. Pause, breathe, and feel what arises.
Let it be
- During your meditation, try to sit with your experience exactly as it is. Allow yourself to simply observe your experience from moment-to-moment, like scenes on a roll of film projected onto a screen. You may perceive this to be pleasant, unpleasant, or neutral – continue to sit with the experience exactly as it unfolds without trying to change it in any way.
- If at any point you become engrossed or caught up in your thoughts, gently turn your awareness back to your breathing. Let the thoughts simply roll away like scenes on a roll of film projected onto a screen.
And Return
- Continue to let your breathing anchor you in the present moment.
- At the end of your “formal” sitting remain still for a few moments, simply noting how you feel at the end of the practice.
Invite this mindful stillness into the rest of your day, taking time to momentarily Stop, Observe, Let it be, And Return as often as you are able.
Narrative Medicine: Another Way to Tune In
Reading or listening to the writings of others can be a powerful way to generate a deeper awareness. Whole not typically classed as a mindfulness intervention, narrative medicine does tend to resonate with many Veterans. Links to Narrative Medicine related tools are listed at the end of this overview.
Back to Linda
Together, you draft a Personal Health Plan (PHP) with Linda. Central to that plan is helping Linda enhance mindful awareness in her life. She has heard a little about “meditation and things like that,” and you guide her through a brief seated meditation during the last few minutes of her visit. You also provide her with information about the mnemonics (SOLAR and TIES) for mindful awareness practice (mentioned earlier in this overview) and she will start incorporating them. She will read the Whole Health Veteran handouts on Mindful Awareness as well, starting with “An Introduction to Mindful Awareness” and “Mindful Awareness Practice in Daily Living.”
You help her create a SMART (Specific, Measurable, Action-Oriented, Realistic, and Timed) goal: “Every day, starting for 5 minutes a day and increasing by 2 minutes a week until I reach 20 minutes a day, I will practice mindful awareness. I will do breathing meditations every morning. I will check in with my primary care team in 2 weeks to let them know how it is going.” For more information on SMART goals, refer to Passport to Whole Health, Chapter 3.
When Linda checks back in 2 weeks later, she is doing fairly well. She does not meditate every day but is averaging 5 or 6 days a week. As you told her, it has gotten easier for her to do over time. She has tried out a number of the digital resources listed at University of Wisconsin-Madison Mindfulness in Medicine website. She also checked out a few CDs with guided mindfulness exercises from the local library. Because it is now covered at her VA site, she has signed up to take a course in mindful awareness offered by her VA facility. During this eight-week course, she is being introduced to several different practices. She has found yoga is very helpful for her back, as well as her ability to focus, so she has added 30 minutes of yoga a day in addition to her other practices.
When Linda follows up three months later, she seems to be improving. She is much more aware of the difficult emotions she experiences, such as the frustration of seeing the same people coming into the hospital repeatedly, and the anger she feels at not being respected by her peers. By becoming more aware of her internal experience, she is able recognize patterns and work with these challenges more effectively. She still aware of the pain in her back, but it does not both her as much as it previously did. She tells you she has learned to separate the pain—the neurological signal from her back—from the suffering it causes her. She describes the suffering as how she chooses to react to the pain, noting that practicing mindful awareness has not lowered the number she would give it on a scale from 1 to 10, but it has enabled her to cope more skillfully with it. (Refer to the module “Self-Management of Chronic Pain” for more information on this and similar approaches to pain.)
Linda comments that she has gotten into the habit of taking a deep breath before she walks into a room to visit with a patient, or before she makes a patient phone call. She feels as though she is “fully present” with each person she sees, and this helps her feel better about the quality of the work she is doing. Her friends and co-workers tell her she seems “less grouchy,” and some co-workers have asked her how she manages to be so busy, and yet still get her work done. Her supervisor has asked her to talk about what she is learning at her eight-week course at a team meeting. She has even begun to teach some of her patients some basic breathing exercises to help them relax before procedures. She now gives herself a 4 on each of the vitality signs, and a 5 out of a possible 5 in terms of where she is versus where she would like to be with Power of the Mind.
Linda smiles as she leaves her visit, noting she will continue to follow up regularly with you or other members of her Whole Health team. She is planning to add some gratitude practices before her next visit.
Whole Health Tools
- Bringing Mindful Awareness into Clinical Work
- Exercises and Readings for Narrative Medicine Groups
- Going Nowhere: Keys to Present Moment Awareness
- Mindful Awareness Practice in Daily Living
- Narrative Medicine
- Practicing Mindful Awareness with Patients: 3-Minute Pauses
- Quick Guide to Using Narrative Medicine in a Busy Practice
Resources
CDs
- Kabat-Zinn, Jon, Guided Mindfulness Meditation (3 part series), Sounds True.
- Kabat-Zinn, Jon, 2010, Mindfulness Meditation for Pain Relief: Guided Practices for Reclaiming Your Body and Your Life, Sounds True.
- Nhat Hanh, Thich, 2009, Living Without Stress or Fear: Essential Teachings on the True Source of Happiness, Sounds True.
- Meditation and Guided Practices section, Sounds True website.
Online
- Center for Investigating Healthy Minds. Center at the University of Wisconsin-Madison that focuses on mindful awareness research.
- University of Massachusetts Center for Mindfulness in Medicine, Health and Society. Founded in 1995 by Jon Kabat-Zinn, PhD. First program to draw mindful awareness training into health care institutions. Offers an array of mindfulness resources.
- University of California San Diego Center for Mindfulness. Institute offering retreat-style professional trainings.
- Oasis Institute. An institute for mindfulness-based professional education and training.
- Mindfulness Based Cognitive Therapy. Designed to help people who suffer repeated bouts of depression and chronic unhappiness.
- Mindfulness Based Relapse Prevention. Developed at the Addictive Behaviors Research Center at the University of Washington, for individuals in recovery from addictive behaviors.
- University of Wisconsin Integrative Medicine. This site features a number of Power of the Mind tools, including a module entitled, “Learning to Meditate.”
- University of Wisconsin Mindfulness Digital Resources. Contains audio recordings of many mindful awareness techniques most commonly used in courses.
- Mindfulness Coach. App designed specifically for Veterans and Servicemen.
Books
For Clinicians
- Segal, Zindel, Mark Williams & John Teasdale (Eds.), 2002, 2013, Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse, The Guilford Press.
- Bowen, Chawla and Marlatt, 2011, Mindfulness-Based Relapse Prevention for Addictive Behaviors: A Clinician’s Guide, The Guilford Press.
- Germer, Christopher K., Ronald D. Siegel, & Paul R. Fulton (Eds.), 2005, Mindfulness and Psychotherapy, The Guilford Press.
- Hayes, Follette, & Linehan (Eds.), 2004, Mindfulness and Acceptance: Expanding the Cognitive Behavioral Tradition, The Guilford Press.
- Hick, Steven F. & Thomas Bien (Eds.), 2008, Mindfulness and the Therapeutic Relationship, The Guilford Press.
- McCown, Reibel, & Micozzi (Eds.), 2010, Teaching Mindfulness: A Practical Guide for Clinicians and Educators, Springer Publications.
- Roemer, Lizabeth and Orsillo, Susan, 2009, Mindfulness and Acceptance-Based Therapies in Practice, the Guilford Press.
- Shapiro & Carlson, (Eds.), 2009, The Art and Science of Mindfulness: Integrating Mindfulness and the Helping Professions, American Psychological Association.
For Veterans and Clinicians
- Baraz, James & Shoshana Alexander (Eds.), 2010, Awakening Joy, Bantam Books.
- Benett-Goleman, Tara (Ed.), 2001, Emotional Alchemy, Random House.
- Brach, Tara Brach, (Ed.), 2003, Radical Acceptance, Bantam Books.
- Brach, Tara Brach, 2013, True Refuge: Finding Peace and Freedom in Your Own Awakened Heart, Bantam books.
- Forsyth & Eifert (Eds.), 2007, The Mindfulness and Acceptance Workbook for Anxiety, New Harbinger Publications.
- Fredrickson, Barbara, (Ed.), 2009, Positivity, Three Rivers Press.
- Goleman, Daniel and Davidson, Richard J, 2017. Altered Traits: Science Reveals How Meditation Changes Your Mind, Brain, and Body, Avery, an imprint of Penguin Random House LLC
- Germer, Christopher (Ed.), 2009, The Mindful Path to Self Compassion: Freeing Yourself from Destructive Thoughts and Emotions, The Guilford Press.
- Gunaratana, Bhante, 2002, Mindfulness in Plain English, Wisdom Publications.
- Kabat-Zinn, Jon (Ed.), 1990, Full Catastrophe Living, Bantam Dell.
- Kabat-Zinn, Jon (Ed.), 1995, Wherever You Go There you Are, Hyperion.
- Kabat-Zinn, Jon, 1991, Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness, Dell Publishing.
- Kabat-Zinn, Jon, 2006, Mindfulness for Beginners, Sounds True.
- Nhat Hanh, Thich & Mai Vo-Dinh, 1991, Peace is Every Step: The Path of Mindfulness in Everyday Life, Bantam Books.
- Nhat Hanh, Thich, 1987, The Miracle of Mindfulness, Beacon Press.
- Orsillo, Susan & Lizabeth Roemer (Eds.), 2010, The Mindful Way Through Anxiety: Break Free From Chronic Worry and Reclaim Your Life, The Guilford Press.
- Remen, Rachel Naomi, 2000, My Grandfather’s Blessings: Stories of Strength, Refuge, and Belonging, Riverhead Books.
- Salzberg, Sharon, 1995, Loving-Kindness: The Revolutionary Art of Happiness, Shambhala.
- Strosahl, Kirk, 2008, The Mindfulness and Acceptance Workbook for Depression: Using Acceptance and Commitment Therapy to Move through Depression and Create a Life Worth Living, New Harbinger.
- Teasdale, Williams, Segal, 2014, The Mindful Way Workbook: an 8-week Program to Free Yourself from Depression and Emotional Distress, the Guilford Press.
- Tolle, Eckhart, 2011, Practicing the Power of Now: Essential Teachings, Meditations, and Exercises from the Power of Now, Hachette Australia.
- Williams, Teasdale, Segal & Kabat-Zinn, (Eds.), 2007, The Mindful Way Through Depression, The Guilford Press.
- Zylowska, Lidia, 2012, The Mindfulness Prescription for Adult ADHD, Trumpeter Books.
Author(s)
“Mindful Awareness” was written by Adrienne Hampton, MD (2018).



















