Clinical Innovations
Mentoring Partnerships
 The Mentoring Partnerships Program, sponsored by the Department of Veteran Affairs, Office of Geriatrics and Extended Care (GEC) is designed to disseminate proven clinical innovations developed by GRECC staff to new sites and provide momentum for enterprise-wide implementation.
The Mentoring Partnerships Program, sponsored by the Department of Veteran Affairs, Office of Geriatrics and Extended Care (GEC) is designed to disseminate proven clinical innovations developed by GRECC staff to new sites and provide momentum for enterprise-wide implementation.
Sites interested in adoption of the program contact the field-based coordinating centers and apply for mentoring as they stand up the new programs. As new sites begin implementation, they receive funding for 2 years, after which the medical facility is expected to have fully integrated the program into its care workflows and takes over for sustainment.
The Mentoring Partnerships Program is proud to support the following programs in FY23-24:
VA Coordinated Transitional Care Program
The Coordinated Transitional Care (CTraC) program was developed at VA Madison Geriatric Research Education and Clinical Center to provide coordinated care for high-risk, aging, and rural Veterans as they transition from the hospital to the community. The CTraC protocol is delivered by a Registered Nurse who identifies high-risk Veterans in the inpatient setting, collaborates with the interdisciplinary team to prepare for the Veteran's transition, and calls the Veteran 48 hours after discharge and at least once a week for up to 30 days to provide intensive case management and care coordination.
Across VA, CTraC has increased patient satisfaction, decreased readmissions by up to 54%, and resulted in significant cost savings of up to $1,842 per patient. Due to its success and widespread acceptability, the CTraC program was chosen for national dissemination by VA's Geriatrics and Extended Care program. Beyond the original CTraC protocol described above, additional CTraC protocols have been developed to meet the needs of Veterans in other high-risk transitions, including:
- COMPASS (developed in VA Madison) – designed to aid with the transition from hospital to a skilled nursing facility
- Supportive CTraC (developed in VA Boston) – designed to improve the quality of end-of-life care for Veterans with serious illness.
To learn more: Caroline.Madrigal@va.gov
Gerofit
 Participants in this exercise program that promotes health and wellness for Veterans have demonstrated improved health, including mental health, physical function, and well-being. Veterans Health Administration, Office of Geriatrics and Extended Care (GEC) funded this program in FY2014 to disseminate it to 4 sites: Baltimore, MD, Canandaigua, NY, Greater Los Angeles, CA, and Miami, FL.
Participants in this exercise program that promotes health and wellness for Veterans have demonstrated improved health, including mental health, physical function, and well-being. Veterans Health Administration, Office of Geriatrics and Extended Care (GEC) funded this program in FY2014 to disseminate it to 4 sites: Baltimore, MD, Canandaigua, NY, Greater Los Angeles, CA, and Miami, FL.
Given the widespread success of the program, the VHA Offices of GEC and Rural Health (ORH) have continued to support dissemination. Two more sites were added in 2015 (Pacific Islands and Salem, MA) with each site additionally developing programs for rural patient outreach. New sites implemented under these mechanisms include Little Rock, AR, Cincinnati, OH, Pittsburgh, PA, Rocky Mountain Healthcare System, Ann Arbor, MI, and Puget Sound.
Gerofit was selected and highlighted in the June 2017, VA publication Best Care Everywhere as one of the innovative and transformative programs within VA and as a Gold Status program in 2018. In FY 2017, GEC and ORH partnered together as the Gerofit program became an enterprise-wide initiative. In FY 2021, Gerofit received designation as a Whole Health program. In 2023, there are 28 programs in VA Health Care Systems across 15 VISNs with several new programs under development. To learn more about current site and further expansion visit: www.va.gov/geriatrics/pages/gerofit_Home.asp
Patient Priorities Care
 Patient Priorities Care is a Whole Health Clinical Care model appropriate for older and/or medically complex Veterans that helps determine person-centered health care goals that are rooted in what matters, but specific, realistic, and within the context of a patient’s care preferences. It is the preferred approach to address “What Matters” in VA care.
Patient Priorities Care is a Whole Health Clinical Care model appropriate for older and/or medically complex Veterans that helps determine person-centered health care goals that are rooted in what matters, but specific, realistic, and within the context of a patient’s care preferences. It is the preferred approach to address “What Matters” in VA care.
It mirrors the ask and act model of Age-Friendly Healthcare Systems (AFHS) in 2 core steps:
- Step 1. Identify Health Priorities (ask)
- Step 2. Align Care with Health Priorities (act)
Patient Priorities Care involves not only the health outcome goals that Matter Most to patients, but also their preferences for health care, what they are willing and able (or not willing and not able to do) to support those health outcome goals. This approach is meant to be a collaboration between patients/caregivers and clinicians.
These copyrighted resources are available to support patients and clinicians in the training and implementation of this approach:
- Clinicians can learn more: Patient Priorities Care VA Implementation Toolkit – Patient Priorities Care VA Implementation Toolkit
- Training in the approach for health care professionals: VA Training – Patient Priorities Care VA Implementation Toolkit
- Patients can learn more: Patient Facing Materials - Patient Priorities Care
Stride
 STRIDE is a supervised walking program for older Veterans admitted to the hospital with medical illness. STRIDE features an early assessment, supervised ambulation, and patient education about the importance of daily walking, all designed to ensure patient safety during program participation.
STRIDE is a supervised walking program for older Veterans admitted to the hospital with medical illness. STRIDE features an early assessment, supervised ambulation, and patient education about the importance of daily walking, all designed to ensure patient safety during program participation.
Developed with input from multiple disciplines, STRIDE fills an urgent need for promotion of early, safe mobility in hospitalized individuals to prevent negative consequences of inpatient bedrest and immobility.
Data from a demonstration trial at the Durham VA show that STRIDE participants were more likely to be discharged to their homes (92%) than STRIDE-eligible patients who did not enroll in the program (74%). Clinical data also show that STRIDE participants had a 1-day shorter length of hospitalization than STRIDE-eligible patients who did not enroll (4.7 days vs. 5.7 days). In addition to clinical improvements, 90% of STRIDE patients reported feeling the same or better after their walk. To learn more: Diffusion Marketplace
Other Clinical Innovations
GRECC Connect
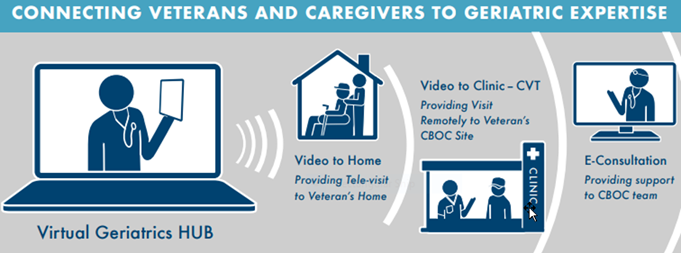
The goal of this program is to provide clinical support through consultation at a distance where geriatric consultation is difficult to obtain or not available and education in geriatrics for frontline rural teams and older Veterans. The program is a multisite project with the Bronx GRECC as the coordinating center (collaborating with multiple GRECCs across the nation) using telemedicine modalities. To learn more: www.ruralhealth.va.gov/docs/promise/2017_02_01_Promising%20Practice_GRECC_Issue%20Brief.pdf
EQUiPPED
Birmingham/Atlanta GRECC is the lead for this 12-site VA collaborative program, including 6 GRECC Sites. The goal is to reduce potentially inappropriate medications prescribed to older Veterans discharged from the Emergency Department. It involves 3 interventions: provider education, provider feedback, and Computerized Patient Record System (CPRS) order sets. To learn more: www.ncbi.nlm.nih.gov/pmc/articles/PMC5070380/
Advanced Care Planning-Group Visits (ACP-GV)
 This program has been recognized as a gold status practice by VA Central Office through the Diffusion of Excellence Initiative. It was selected for national roll-out in 2016. In addition, ORH selected ACP-GV for a Pathway to Partnership, which has subsequently led to Enterprise Wide Initiative (EWI) funding. The goal of the program is to engage Veterans and their trusted others efficiently and effectively in advance care planning. To learn more: www.va.gov/geriatrics/pages/advance_care_planning_group_visits.asp
This program has been recognized as a gold status practice by VA Central Office through the Diffusion of Excellence Initiative. It was selected for national roll-out in 2016. In addition, ORH selected ACP-GV for a Pathway to Partnership, which has subsequently led to Enterprise Wide Initiative (EWI) funding. The goal of the program is to engage Veterans and their trusted others efficiently and effectively in advance care planning. To learn more: www.va.gov/geriatrics/pages/advance_care_planning_group_visits.asp
GeriPACT
 Developed as a patient centered medical home care model for frail elderly with enhanced quality of care and patient safety. This program tracks quality measures and developed the Geri-PACT dashboard in collaboration with the Geriatrics and Extended Care Data Assessment Center. To learn more: Geriatric Patient Aligned Care Team GeriPACT - Geriatrics and Extended Care (va.gov)
Developed as a patient centered medical home care model for frail elderly with enhanced quality of care and patient safety. This program tracks quality measures and developed the Geri-PACT dashboard in collaboration with the Geriatrics and Extended Care Data Assessment Center. To learn more: Geriatric Patient Aligned Care Team GeriPACT - Geriatrics and Extended Care (va.gov)



















