Implementing Whole Health in Your Practice, Part I: What a Whole Health Visit Looks Like
The Whole Health approach is patient-driven and personalized. It incorporates elements of self-reflection, assessment, shared goal setting, and various types of support to achieve those goals. Using a patient vignette, this overview illustrates how to implement these strategies in clinical practice. It also demonstrates how a Whole Health visit can empower the patients and be more fulfilling for clinicians.
Key Points:
- Every Whole Health visit will be unique, but there are certain elements, the “Key Principles of Personal Health Planning,” that are likely to be part of most of them.These include Self Reflection, Whole Health Assessment, Goal Setting, and assistance to help achieve the goals that are set, such as Education, Skill Building, Resources, and Support.
- By focusing on a person’s values and building the visit upon what really matters to them, you take the conversation in new directions. Veterans are more likely to adhere to the plan if you co-create it with them, focusing on their values.
- It is helpful to have your own introduction to Whole Health (an “Elevator Speech”) that you can share with a Veteran or colleague who is new to Whole Health.
- Make use of Personal Health Inventories (PHIs) a Whole Health Assessment tool.There are tips you can follow as you review them, to make the most out of the information they contain.
- All the elements of a conversation—who, what, when, where, and how—can be shaped to support Whole Health,
- Tailor the Whole Health Approach to your own practice style, and take time to decide how best to document and bill for Whole Health visits.
- Remember, providing Whole Health takes a team-based approach.Veterans may learn about Whole Health, complete a PHI, and choose areas to focus on before they ever see a clinician. Many different options are available for helping them follow through their Personal Health Plans (PHPs) as well.
Introduction
“To write prescriptions is easy, but to come to an understanding of people is hard.”
—Franz Kafka
Whole Health sounds good in theory, but how to you actually bring it into the real world? You may have already explored how Whole Health can influence your own self-care practices, but what about the care of your Veterans? How is a Whole Health visit different from a standard medical visit?
Chapters 2 and 3 of the Passport to Whole Health introduce the “Key Principles of Personal Health Planning” (Figure 1). While those chapters cover the theoretical benefits of Whole Health (and it is probably best to read them first), this overview focuses more on actual practice. Here, we will answer practical questions, such as “How does a busy clinician apply key principles of personal health planning with such limited time during clinic visits. As you work through this narrative, pause every so often to ask how you can tailor what you are learning to your practice style.
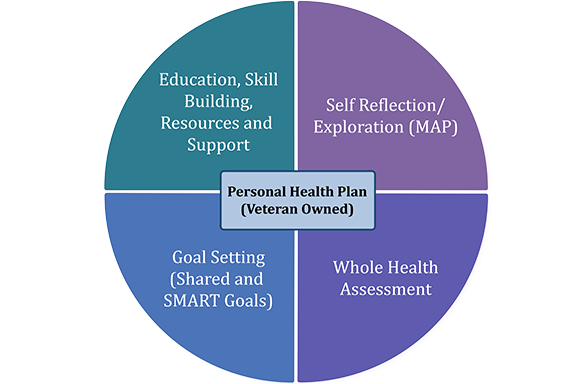
Figure 1. The Key Principles of Personal Health Planning
While this overview offers the example of an encounter between one clinician and one patient, and assumes the patient has never heard of Whole Health before, Whole Health truly requires a team effort. As they say, “It takes a village to practice Whole Health.” Therefore, throughout the overview, we have provided suggestions about how a patient’s entire team can work together to make the process more successful. In a well-functioning Whole Health System, a Whole Health Coach or Peer Partner may have already started the planning process with a Veteran before they meet the clinician. The Veteran may be independently involved in various well-being programs (e.g., meditation courses, Whole Health group visits, or Whole Health Coaching). Several members of a patient’s care team, from across disciplines, contribute to the patient’s Personal Health Plan (PHP); it is not the responsibility of any one clinician to complete the entire process. Since the PHP is continuously evolving, the ideal is for the plan to follow Veterans wherever they go in the VA system, as part of the Electronic Medical Record (EMR).
Meet the Veteran
This overview is built around the experiences of a 68-year old Vietnam Veteran named Bob, who has received care from the VA for years. Note: His experience (including a dialog between Bob and his clinician during a Whole Health visit) is highlighted with a yellow background, in case you want to focus on the Veteran vignette.
Most of us have treated patients similar to Bob. He typically comes alone to his appointments and is very familiar with his long-term primary care provider. Bob shows up to most of his scheduled appointments and is both quiet and polite. He often answers questions with very brief responses. He is aware of his many medical diagnoses (which are listed below) but has still found it difficult to keep up with his medical needs.
His many diagnoses include:
- Dyslipidemia: Bob’s LDL is 160, triglycerides are 260, and HDL is 30.
- Hypertension: His average blood pressure is 170s/90s.
- Elevated BMI: His weight is 250 lb; body mass index is 33.
- Insulin resistance. His hemoglobin A1c is climbing, and he is developing metabolic syndrome.
- PTSD: Bob has a few flashbacks per week, and it affects his sleep.
- Depression and anxiety. Bob does not regularly take his prescribed antidepressant, citalopram. In the past, his psychologist has been concerned about his risk for suicide.
- Chronic pain. Bob has severe arthritis in his knees. He is taking 2400 mg of ibuprofen a day.
- Chronic abdominal bloating. Ten years ago, he was diagnosed with irritable bowel syndrome (IBS) by a gastroenterologist after an extensive workup.
- Insomnia:Bob sleeps 5-6 hours each night and is tired all the time. Some nights, he uses an over-the-counter sleep aid. Every night, he drinks a shot of whiskey before bed.
- Alcohol use. Bob’s daughter reports he has been drinking heavily, even beyond the whiskey before bed that he initially admitted to. This pattern started after he lost his wife a few years ago.
- COPD, Tobacco use. Bob smokes 1½ packs daily and has done so for over 40 years. He has been diagnosed with Chronic Obstructive Pulmonary Disease (COPD).
Bob’s providers feels as though they have reached the limits of what medications, referrals to specialists, and procedures they can offer him. In the past, he has not followed through with many of their suggestions anyway. In fact, he often does research on the Internet or reads mail from dietary supplement companies and tries complementary therapies that his health care team members do not know much about. Bob’s primary care provider has used motivational interviewing and discussed behavior change with him dozens of times, but each year his weight and blood pressure continue to creep up.
Mindful Awareness Moment
Take a moment for mindful awareness.
- When you think about the prospect of seeing someone like Bob for a visit, how do you feel?
- If you were the one seeing Bob, what could you do, both for Bob and for yourself, to make this visit as worthwhile as possible?
- How might the Whole Health Approach help change how this visit goes?
Is it possible that this encounter could not only be more fulfilling for Bob, but also for you, as the clinician?
Before the Visit: Personal Health Inventory
Bob has never been introduced to Whole Health before. To date, he has not worked with a Whole Health Partner (a Veteran peer trained to support fellow Veterans as they engage in personal health planning). Until today, he has never completed a Personal Health Inventory (PHI), a questionnaire designed to get him thinking in more depth about his self-care and the professional care he receives. Bob received a blank copy of the Brief Personal Health Inventory when he arrived for his visit and filled it out in the waiting room. The two page PHI is being used nationwide as sites incorporate the Whole Health System model. (Several VA sites have found that people seldom complete the PHI when it is mailed in advance of their appointment, so now it is more commonly given to them when they arrive for their visit.)
As Bob filled out the PHI, he noticed the Circle of Health posted on a bulletin board. Many VA sites find it helpful to post information about Whole Health in prominent locations, such as in a waiting room, in the hall of a hospital, or in the cafeteria. One facility even posted the Circle of Health inside its bathroom stall doors! Advertising whole health can increase awareness and engagement among Veterans.
As you may already know, the Brief PHI (and the longer MyStory Personal Health Inventory) are organized around the elements of the Circle of Health (Figure 2). The PHI allows Veterans to share information not typically covered on intake forms issued by clinics or inpatient services. It casts a broad net, focusing on everything from what matters most to patients, to self-care practices, to insights a patient has about what their next steps should be. The PHIis not used instead of a standard patient history and physical, but rather, in conjunction with it and any other assessments a patient completes. For more information, refer to “The Whole Health Note: Beyond the Standard History and Physical.”


Take a moment to look over Bob’s completed Brief PHI.
Mindful Awareness Moment
Now that you have reviewed Bob’s PHI, consider the following:
- How well does the Brief PHI give you a sense of Bob and his health care needs now, compared to when you read his health history earlier?
- How long do you think it took Bob to fill out the Brief PHI? Is the added information useful?
- How much time did it take you to review the PHI? Most clinicians say that it saves them time to have all that information before they start talking to a Veteran. Do you agree?
- How often should Bob complete a PHI? Yearly? Every 2 years? Every 6 months?
- How can you get the PHI into Bob’s medical record?
ANATOMY OF BOB’S BRIEF PHI
The 4 parts of Bob’s Brief PHI offer his clinicians a sense of the different ways they could frame a conversation with him.
1. Vitality Signs
These 3 rating-scale questions provide a quick snapshot of where Bob is in terms of his physical and mental/emotional well-being (which he rated 1/5 and 3/5 respectively). Bob also rated himself 2/5 in terms of how it is to live his day-to-day life. This merits further discussion, particularly since there has been a concern about his suicide risk in the past.
2. The Big Questions
“What do you live for?” “What matters to you?” “Why do you want to be healthy?” Bob’s answers to these give insights into his Mission, Aspiration, Purpose (MAP). Bob’s answers on the Brief PHI make it clear his family matters. He is focused on his role in the upcoming wedding. He also values his independence, helping others, and his faith. A clinician can bring up some of these topics when asking Bob to set goals that honor what he truly values.
3. Where You Are and Where You Would Like to Be
These 9 questions had Bob rate where he is versus where he wants to be for the 8 areas of self-care and his overall professional care. Some questions to consider when reviewing this section of Bob’s Brief PHI include the following:
- First, what is Bob doing well? The 5/5 he gave himself on Surroundings is striking, as are his ratings of 4/4 for Personal Development and 4/5 for Spirit and Soul. 4/5 on Professional Care suggests this is another area he feels pretty good about. It can be helpful to discuss strengths during Whole Health visits, not just areas where there are deficits.
- Where does Bob score low, relative to where he would like to be?Certainly the 1/4 on both Moving the Body and Food and Drink stand out. So does the 2/4 for Recharge. The 3/5 for Family, Friends and Co-Workers might seem a bit surprising, given his strong ties to his daughter and her family. It may be helpful to ask what led to that rating.
- It is also interesting that he gave Power of the Mind a 3/3. This may indicate that he is not sure what it entails, or that he is not interested in exploring that aspect of self-care at this time. This is worth asking about, as time allows.
Remember, it isn’t just about the numbers. They give clinicians a sense of where to start, but then Bob needs to guide the process in terms what are his highest priorities. Of course, his clinician can suggest what might be a good area of focus as well. This is the essence of shared goal setting; both Bob and the clinician share their perspectives.
4. Reflections
The final two open-ended questions on the Brief PHI can lay the groundwork for creating a PHP. Bob visualizes his best possible self, then he is asked how he can move in that direction. The question of “Where might you start?” is extremely helpful in guiding first steps around creating a PHP. For Bob, his answers suggest it might help to start by asking him about Moving the Body and Food and Drink. Power of Mind may also be important, when it comes to his PTSD. Or, a different area of the Circle of Health may come up.
Some clinicians, particularly mental health clinicians, prefer to go into even more detail with the Whole Health Assessment. The PHI Booklet helps with this. It goes into more depth than the Brief PHI, with additional sections where people can explain each of their ratings for the nine “Where You Are and Where You Would Like to Be” sections. Refer to “Bob’s Personal Health Inventory Booklet” and “Reviewing Bob’s Personal Health Inventory Booklet” to get a better sense of this. Of course, a clinician may not be able to start a visit with a completed PHI, but it is still possible to do a visit. One approach is simply to show a Veteran the Circle of Health and ask them where they would like to set a goal. A simple tool to help a person spend additional time with the various self-care circles and consider where they might want to focus is the tool, “Circle of Health: A Brief Self-Assessment.”
During the Visit, Part 1: The Parts of a Whole Health Conversation
“It is our attitude at the beginning of a difficult task which, more than anything else, will affect its successful outcome.”
—William James
After Bob’s Brief PHI has been reviewed, the next step is to have a conversation with him. A Whole Health conversation requires clinicians to move beyond the “find it, fix it” model we are trained to use as students. As is reflected in the PHI, the focus shifts from “What’s the matter with you?” to “What matters most to you?” Of course, his clinician will still address health concerns and administer treatments as appropriate, but it happens in a different context; the conversation is changed.
There are 5 key elements to any conversation. You can move a patient visit in the direction of Whole Health by focusing on any one of them.
1. WHO: THE PARTICIPANTS IN THE CONVERSATION
In this case, the participants are the clinician and Bob, the patient. Both have (agendas) for the visit. It is important to keep returning to the question of what Bob wants to get out of his visit.
Having patients share their goals during a health care visit has important health benefits. A 2003 review concluded the following:
Greater expression of patient perspectives through active participation in the medical encounter favorably impacts a variety of outcomes, presumably through a better adherence to recommended treatment regimens. Such outcomes include faster symptom resolution and better biomedical parameters, such as lower blood pressure and glycohemoglobin levels (A1c’s). Physician solicitation of patient perspectives also has a positive impact on patient trust, satisfaction, and adherence. In addition, the ability of patients to share their perspective through narrative satisfies a basic human need for expression that may in itself have therapeutic value.[1]
Personalizing care—and really getting to know Bob—can dramatically increase how involved Bob is in creating his PHP. Patient-driven care is a hallmark of the Whole Health Approach.
2. WHAT: THE MESSAGE OF THE CONVERSATION
There are many different ways to give and receive information during a patient visit. Body language plays an important role. So does a review of the patient's medical records. Literacy matters as well. Can Bob read and write well enough to complete a PHI on his own? Can he understand health concepts well enough to “get” what is going on with his health? Does he understand numerical concepts well enough to take his medications properly?
The questions a clinician asks are an indication of what is important to that clinician about Bob’s care. Depending on where conversation goes, Bob can be inspired to practice more self-care, or made to feel guilty about his lack of adherence to taking his medications. He can leave feeling genuinely heard and cared about, or he can leave feeling like his clinician was judging him or too rushed to engage with him. As noted in “Implementing Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence,” a clinician’s communication skills, level of empathy, and other elements they bring into the visit can have a huge impact on patient outcomes.
3. WHEN AND WHERE: THE SETTING FOR THE CONVERSATION
The setting of the conversation also matters. Whole Health conversations are best held in a welcoming setting, with good lighting and few distractions. Many factors influence the conversation’s setting, including but not limited to: wall colors, smells, noise level, room temperature, the art on the walls. Does the professional environment foster healing? You can read more about the importance of a healing environment in “Surroundings” and related Whole Health tools on this website.
Time is also a factor. If a clinician is rushed or tends to interrupt to speed up the appointment, the visit will be less satisfying to Bob. For more information on this important topic, refer to “Implementing Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence.”
4. WHY: THE PURPOSE OF THE CONVERSATION
Each of us has ways of deciding that we believe something is true. Different people trust different sources of information, and they have different views on where a conversation should be focused. The clinician’s agenda for a visit may be very different from Bob’s. Bob may want to talk about his pain, while the clinician wants to focus on meeting blood sugar goals. Bob may smoke because it is the only thing that relaxes him enough to function despite his PTSD and anxiety, but if his clinician does not know that, the focus of the conversation may turn to all the reasons why smoking is bad and why Bob should quit, which may not be helpful.
Bob may have different standards for deciding what is true for him medically. His team has discovered over time that he prefers complementary approaches. Bob draws a lot of his ideas about what to do for his health problems from the Internet and from friends dealing with similar issues. Why is that? Which websites does he use? It may be valuable to explore these preferences and interests with him.
A clinician may be more inclined to focus on the medical literature and clinical experiences to guide personal health planning. Bob’s approach is likely different. How can Bob’s team members meet him where he is, yet still offer their perspectives? The more both parties can communicate where they are coming from, the better the conversation will go. You can learn more about how to work with differences in belief systems in the Whole Health tool “How Do You Know That? Epistemology and Health.”
5. HOW: THE TONE OF THE CONVERSATION
Body language, empathy, communication styles, and other such factors also have an important effect on a conversation’s outcome. If Bob is merely viewed as a list of problems, or if his sense is that his clinician prefers just to tell him what to do without his input, the conversation will fall flat. If the visit lacks empathy and personalization, it will be less useful to him and he may be reluctant to see the same clinician again.
Mindful awareness on a clinician’s part changes the flavor of a conversation. (Refer to “Mindful Awareness.”) If Bob knows he is the most important thing on his clinician’s mind during a visit and that he is truly being heard, the visit will be more useful to him and more fulfilling to the clinician as well.
During the Visit, Part 2: Applying Principles of Personal Health Planning
Everything discussed thus far, including PHIs and the elements of a Whole Health conversation, inform the personal health planning process, depicted in Figure 1. The PHI supports self-reflection; it is the backbone of the Whole Health Assessment. No matter what sort of clinician you are (dietitian, social worker, psychologist, nurse, physician, etc.) you may notice that it brings new perspective into a Whole Health visit. It is important to note that you may not touch on every element of the PHI in a single visit and that's okay! Tailor the visit to your needs and the needs of your patient.
In the following section of this module, each of the elements of personal health planning elements is described below. Then, the section after that illustrates how they can be used in a visit with Bob.
1. THE ELEVATOR SPEECH: INTRODUCING WHOLE HEALTH
The Whole Health Elevator Speech is an introduction to what Whole Health is and why it is important. The Elevator Speech is brief; a good ballpark is that it is less than 100 written words which takes less than 1 minute to present. Guidance for writing an Elevator Speech is featured in chapter 2 of the Passport to Whole Health.
2. SELF REFLECTION AND EXPLORATION (MISSION, ASPIRATION, PURPOSE)
Questions related to these elements are featured in the PHI. Always return to the “why” of the visit. How does the conversation reflect what is most important to the Veteran?
3. WHOLE HEALTH ASSESSMENT
The PHI has already been discussed as one tool of a Whole Health Assessment. Clinicians can also use other forms and assessments, as they wish.
Regardless of whether or not a person has completed a PHI, clinicians can still show them the Circle of Health and ask them what they think about its different parts. If they do complete a PHI, the “Where You are and Where You Would Like to Be” section can offer a brief glimpse into their strengths and challenges.
It is good to focus first on what a person is doing well. After looking at and discussing strengths, a clinician can shift focus to areas they would like to work on. Do not assume the numbers will always indicate which area they will choose to discuss first. Also, do not let this become overwhelming; it is often best to focus on one goal in just one area of the circle. Some people initially assume that they need to talk about all of them right away. Additional circles can be discussed at future visits.
Once a person has chosen a general area of focus, their team members can help them zone in on specifics. There are entire chapters in the Passport to Whole Health, as well as overviews and Whole Health tools on this website, dedicated to each of the areas within the Circle of Health. To take your Whole Health Assessment deeper, refer to “Questions You Can Ask During a Whole Health Visit” for a list of potential (though, of course, not in any way required) questions you can ask about each of the different components of the Circle of Health. There are eight skill-building courses for Veterans, one for each area of self-care in the Circle of Health.
4. GOAL SETTING: CREATING THE PERSONAL HEALTH PLAN
One indicator of a successful Whole Health visit is if a Veteran comes out of it with at least one specific goal. Ideally, clinicians and patients create goals together (shared goals). Motivational Interviewing training is helpful here. Goals that are Specific, Measurable, Action-Oriented, Realistic, and Timed (SMART) are especially useful. (For more information, if you need to refresh your knowledge, refer to “How to Set a Smart Goal.”) Consider asking how important (scale of 1 to 10) the goal is, as well as how confident they are (scale of 1 to 10) they can reach the goal.
5. NEXT STEPS: SKILL BUILDING, REFERRALS, FOLLOW UP, AND ONGOING SUPPORT
At the end of every visit, a Veteran should have a clear understanding of what will happen next. Next steps may include the following:
- Skill building. This could mean taking a class, like one of the Whole Health skill-building courses offered at some VA sites, or other self-care related classes, such as a class on yoga, tai chi, or meditation. It might also mean reading handouts or online materials for Veterans like the ones featured on the VA Office of Patient Centered Care and Cultural Transformation SharePoint.
- Referrals. This might mean going to see a specialist, such as a surgeon, pain expert, cardiologist, or oncologist. It might involve seeing someone in mental health, social work, chaplaincy, pharmacy, nutrition, or some other area. In addition, it may mean seeing a complementary and integrative health (CIH) practitioner.
- Follow up and ongoing support. Follow up and support may be offered by the clinician doing the visit, a Veteran peer, a Whole Health Coach, or any number of other team members. In some programs, nurses call patients to check in. The key is to ensure there is some accountability.
6. YOUR THERAPEUTIC PRESENCE
As you know, there are many ways clinicians influence a visit that extend beyond the words they say. Communication skills, empathy, listening, role modeling, and many other factors can influence how effective a patient encounter proves to be. For more information, refer to “Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence.”
During the Visit, Part 3: What Do Bob and His Clinician Actually Say?
This section provides a sample dialog between Bob and his clinician, to give you a sense of how a Whole Health visit can unfold. What follows is an idealized example of what might be said. As you read it, consider how you would have a similar conversation. How would your own area of expertise and style of practice change things, if you were having the conversation with Bob?
There are a few Whole Health tools that can support you with Whole Health conversations. For example, “Questions You Can Ask During a Whole Health Visit” features key questions for each component of the Circle of Health. You can also review and print the “Long Personal Health Plan Template” or the “Brief Personal Health Plan Template,” both of which have space where you can write in your recommendations for Veterans as you co-create their plans with them. Reminder: You may not fill out the entire template yourself, and some of the information may be gathered by other people on the care team.
1. SETTING THE STAGE: THE ELEVATOR SPEECH
Bob’s provider reviews Bob’s PHI using the tips listed above, and then enters the exam room.
Clinician: Hi, Bob. It is good to see you again.
Bob (arms folded, making limited eye contact): Thanks. You too.
Clinician: Thanks for filling out the Personal Health Inventory (PHI) form. Have you heard much about this Whole Health Approach the VA has been adopting?
Bob (makes brief eye contact): No, not really.
Clinician: Well, it’s based on the idea that we want to do a better job focusing on what matters most to you. We will, of course, keep talking about your medical concerns, but I would like to frame our conversation today around the things that are really important to you in your life, why you want to have your health for in the first place. Going forward we will work with you to create a plan that will honor your values and priorities. What do you think?
Bob (furrowed eyebrows, looking a little surprised, shifting in his seat): Hmm. Okay, I guess so.
Clinician: I appreciate it. So far, I have found that this process helps me to get to know people better—even ones I have taken care of for a long time. It also acknowledges how so much of our health is about how we take care of ourselves. And it taps into all sorts of approaches, including complementary and integrative health (CIH) ones, which I know are important to you. After we look over the PHI together, I will work with you to you to create what we call a Personal Health Plan (PHP).
Bob (eyebrows raised, looks both curious and skeptical): I’m game.
2. SELF REFLECTION AND EXPLORATION (MISSION, ASPIRATION, PURPOSE)
Clinician: Great. For starters, can I just say, I was really struck by a lot of your answers on the PHI. It sounds like you have a lot going on in your life. Can you tell me, to start out with, what matters most to you in your life? In other words, why do you want to be healthy? What do you want your health for?
Bob (pausing, making more eye contact): Yeah, my family comes first. I do a lot to take care of my grandkids and help my daughter, because she lost her husband in Iraq a while back. She has 5 kids. The oldest is 22, and the youngest is 10. I like to stay on the move, and I need to be in good enough shape to keep up with my grandkids. My oldest granddaughter is getting married next year, and I want to be able to walk her down the aisle, since she doesn’t have her dad to do it.
Clinician (realizing this is the most Bob has ever said at one time during a visit): Thanks for sharing that. I think your family is really lucky to have you. I really want to support you as you work on being ready for the wedding. And I know that could be tough with your arthritis and everything.
Bob (nodding): Yeah. I gotta be able to get rid of some of this pain in my knee, and I want to make sure my heart stays strong. I can’t die on my daughter. She already lost her mom and her husband. Plus, if my knee hurts all the time, I can’t get any exercise, and I can’t get out to do photography.
3. WHOLE HEALTH ASSESSMENT
Clinician (pointing to a printout of the Circle of Health): On the form you filled out, you saw this Circle of Health. When you look at the circle, what areas do you think you are doing well in?
NOTE: Remember, it is important to focus on what a person is doing right, not just to jump to the areas on the PHI where they rated themselves with a lower number.
Bob (takes the diagram and studies it for a few moments): Well, I gave myself a 5 for Surroundings, because I have a great place to live. I haven’t been able to keep my wife’s flowerbeds going as strong as I would like, but I mow the lawn plenty, especially with all the rain we’ve been having. I also feel good about my photography projects and fishing with my grandsons. I am pretty spiritual too.
Clinician (nodding): I noticed that, and I am really glad you have all those interests. You know, we health care people always seem to be talking about areas where you can do better, but I want to make sure you give yourself a pat on the back for all the great things you are already doing for your health. And these sorts of things—especially your spirituality and family, it sounds like—can really support you through life’s challenges.
Bob (nodding, eyes a little glassy): Yeah. They do.
Clinician: And when you look at the Circle of Health, is there a circle that jumps out at you as a place to focus on right now? We have a lot to go over today, so maybe we can talk about one now and then get to others at future visits.`
Bob (focused on the Circle): Well, on that last question on the form they gave me, I wrote down Moving the Body and Food and Drink. But I am really thinking about working on Recharge too.
NOTE: At this point, the conversation is shifting from Whole Health Assessment into setting goals and creating a plan.
4. GOAL SETTING: CREATING THE PERSONAL HEALTH PLAN
Clinician: What I am hearing is that we should start by focusing on Recharge, for starters. Why is this important to you?
Bob: My sleep has been terrible. My psychiatrist has been talking with me about medications, but anything else that can help would be great. I don’t want to just go back on something like Valium. And if my sleep is good, everything else gets better, like my mood and my energy to exercise.
Clinician (nodding thoughtfully): Sure. I understand. I have a few ideas about things that can help with sleep, but what are your thoughts?
Bob: Well, one of my buddies told me there is a sleep app I could put on my phone, CBT-something.
Clinician: CBT-I? That stands for Cognitive Behavioral Therapy for Insomnia, and it has good research supporting it. A lot of the Veterans in my practice have really found it helpful. I can get you some more information on the app. And, we also have psychologists who specialize in this therapy. Would you be interested in seeing one of them?
NOTE: At this point, the clinician could refer to a psychologist who offers CBT-I, provide Bob with a relevant patient handout, discuss mind-body skills, or teach Bob more about the CBT-I app. Refer to “Recharge” and related Whole Health tools for more information on ways to sleep. There is a Recharge chapter in the Passport to Whole Health as well.
Clinician (remembering Motivational Interviewing skills training from a few years back): By the way, I see you gave yourself a 2 on Recharge and you would like to be at a 4. Why didn’t you give yourself a 1?
Bob: Well, I do usually sleep a few hours a night, and I think of a 1 as being even worse than that. 5 would be 8 hours every night, but I don’t know if that would ever be possible for me. That’s why I said a 4 is where I want to be. I definitely think working with someone on my sleep might help.
NOTE: When asking about the selected numbers for any part of the circle, it’s best to ask questions such as “Why not a lower number?” or “What would a higher number look like?” Do not ask patients why they didn’t give themselves a higher number. That focuses on the negative and is less effective.
Clinician: In relation to your sleep (along with your depression and your PTSD), I also wonder if it would help to talk about how you manage stress. In the Circle of Health, this is represented by the Power of Mind circle. It is this circle here (points to it on the diagram). We know that our mind plays a huge role in affecting our health, and I wonder if meditation might help you out. We have classes here at the hospital, if you are interested.
NOTE: The circles overlap, and that is fine. Working with one topic might draw in techniques from other areas. Again, Bob’s responses should direct the conversation. Discussing the Power of Mind can guide the conversation towards mind-body tools, which might help Bob, if he is open to them. Note the clinician is asking Bob what he wants to do, rather than telling him what to do.
Bob: For now, how about we stick with the CBT-I for sleep? I would need to read up more on Power of the Mind, because I really don’t know a lot about it. And by the way, one of my friends said acupuncture is good for PTSD.
Clinician: I appreciate that you are coming up with a lot of great options. How about I give you some more information on insomnia and sleep hygiene for now? Then, maybe at a future visit, depending how you are doing, we can go into more detail with other mind-body approaches or talk more about acupuncture.
NOTE how the clinician is weaving in his/her thoughts and preferences, but also is respecting Bob’s opinions.
Clinician: Based on what we’ve been talking about I think it would be helpful for us to fill out some of the parts on this form together (shows Bob a Personal Health Plan Template) to create a personal health plan for you. At this point, we decided we are going to have you see a psychologist for the sleep work, and maybe get that phone app for CBT-I at the same time. Let’s take a second to write out some goals for you….
NOTE: The clinician and Bob could now proceed in a few different directions. The Brief and Long Personal Health Plan Templates can help guide this part of the visit. One option is to write a SMART goal together. These are discussed in Chapter 3 of the Passport to Whole Health, and in the tool “How to Set a SMART Goal.”
Another way this could go would be for Bob’s PHP to end up being a list of suggested handouts, courses, and referrals that Bob can look over before he gets in for a future visit. What the plan looks like will depend on how much time is available. The more time, the more areas a clinician can focus on. Many clinicians worry initially about the Whole Health Approach taking too much extra time. If this is a concern for you, check out “Implementing Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence.” Also, keep asking yourself how other members of the team can support different parts of the personal health planning process.
An example of a PHP for Bob is provided below; it offers an example of what a very detailed plan might look like. Again, for a short visit, the PHP may simply be one SMART goal, or an agreement that the Veteran will read through a particular handout and then check back in.
5. ARRANGING NEXT STEPS: SKILL BUILDING, REFERRALS, FOLLOW UP, AND ONGOING SUPPORT
NOTE: As the visit proceeds and goals are set, the conversation will likely shift in different directions, to cover other necessary parts of the visit. Bob and his provider may shift to a focus on the Professional Care part of the Circle of Health. They may talk about medication refills, test results, physical therapy for his hip, a referral to the diabetes clinic, etc. Ideally, Bob will leave the visit feeling empowered to help himself, and he will have good support from his care team.
Here is one way that this discussion might conclude for Bob:
Clinician: OK, so you are good with reviewing the handouts on good sleep that I will print off for you, and we’ll set you up to see a psychologist for CBT-I. I know you have explored a lot of options related to sleep in your past, and depending how things go, we can talk more later about meditation or acupuncture. Both of these are covered VA services for some conditions, and we can see if you would qualify for them.
I think it would be great if you could follow up with your SMART goal. You decided it would be, “Starting tonight, I will stop reading in bed and always try to go to bed and get up at the same time.” That is a great place to start.
Our team will call you to see how it is going. I will see you back in about 2 months to check in. In the meantime, I want you to follow up with your psychiatrist and your dietitian as scheduled. Those visits are already on the books.
Here is a summary about everything we have been talking about (hands Bob the completed PHP, with some notes jotted down on it). We’ve covered a lot! What do you think? Does this seem doable? I don’t want to give you too much to do, but the more you can have the power to support your own health with good support from your care team, the more likely you are to be ready for the wedding!
Bob (more engaged than his provider has ever seen him before): I am good with looking at all this. It is good to have some new directions I can think about. Thanks. I appreciate it. I’ve never had anyone in health care talk to me about things like this before.
Clinician: It is my pleasure. I really appreciate you taking the time to share. I really want to hear about how things go at the wedding, when the time comes.
And so the visit concludes.
This is just one example of what a Whole Health encounter could look like. Visits will vary based on who the clinician is, how long the visit is, and the setting where it happens (e.g., inpatient, outpatient, etc.).
In addition, each patient will respond differently to the process. Some people struggle because they are in the habit of having their clinicians tell them what to do, and they are used to passively listening to instructions. Some are cautious, because they do not want to negatively affect what the VA will cover for them; they worry that doing better can mean less reimbursement for services. If that seems to be the case, talk with them about their concerns.
6. THERAPEUTIC PRESENCE
This is not so much a specific step in the personal health planning process as something that is a part of the whole encounter. This is the focus of “Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence.”
Signs that Bob’s clinician successfully made good use of therapeutic presence during the Whole Health visit include the following:
- Bob feels like his provider really listened to him and paid attention to what he wants to focus on. Because of this, he is more likely to follow through with his health plan.
- The clinician has a better sense of who Bob is and what motivates him.
- The process happened in a reasonable amount of time. It will be even easier next time, because he and his clinician can pick up where you left off.
- Bob has more options, and he is more empowered. He also feels that his efforts have been acknowledged.
- The clinician feels energized by the visit, rather than depleted.
Bob’s Personal Health Plan: What He Takes with Him
Documentation is a necessary part of any visit. As mentioned before, PHPs vary in length, depending on the length of the visit, Veteran preference, and clinician style. Here is an example of a PHP for Bob that was created using the Brief Personal Health Plan Template. For teaching purposes, this is very detailed, with some additional information that was not mentioned so far. What you put in your Veteran’s templates and how you document the visit will vary. You do not need to fill out every section. The following is designed to give you some ideas.
Personal Health Plan
Name: Robert (Bob) Smith
Date: Today
Mission, Aspiration, Purpose (MAP):
My mission, aspiration, or purpose in life is…
To be active with events that really matter to me. To be there for my daughter and grandkids. To live a full and meaningful life where I stay healthy for as long as possible.
My Goal(s)
In 12 months, I want to be able to walk my granddaughter down the aisle to give her away, and I want to stand in for the father-daughter dance with her at her wedding reception. I also want to be able to do better taking care of my wife’s flower beds and to spend as much time as I can outside doing nature photography.
NOTE: The goals for this section are more general. SMART goals can be featured here too, or in the “Areas of Self Care” section.
Strengths (what’s going right already)/Challenges
Strengths include my faith, my connection with my family, and having some good friends who are also Veterans. I rated my Surroundings highly, because I really like where I live. I have regular Professional Care at the VA with a team that does a good job. I am also happy with where I am with Personal Development, because photography keeps me busy.
Challenges include my sleep pattern, my PTSD flashbacks, and my heart disease risk. Depression makes me less engaged with other people. I want to keep the sugars from going up any higher. Arthritis pain limits activity. Want to cut back on drinking, and will focus on that more at future visits.
Mindful Awareness
We can keep talking about this more, but it is important to take some time for you, so that you can notice what you need, even as you do such a good job taking care of others. Practice paying more attention to what your body tells you through symptoms. This could include watching to see if you are truly hungry before you eat. In terms of sleep, which was a big goal for you today, pay attention to your sleep patterns. What seems to help you sleep, and what doesn’t?
NOTE: If you type out a PHP like this, it is fine to add a few other suggestions, even if you didn’t go into detail with them all during the conversation.
Proactive Self-Care
NOTE: Recharge is put first, since it is the main area for Bob to focus on right now. Some additional examples of SMART goals have been added for other areas as well.
- Recharge
- “Starting tonight, I will stop reading in bed and always try to go to bed and get up at the same time.”
- See the expert on CBT-I.
- Download the CBT-I app on your smartphone.
- Review the information on healthy sleep in the Whole Health Veteran materials. Make sure you follow the sleep hygiene steps.
- We can talk more in the future about melatonin, which is on the VA formulary and might help you.
- Moving the Body
- “Starting on the first of the month, I will walk outside or use my stationary bike for 20 minutes, 5 days a week. I will check in with my Whole Health Coach a week after I start to update her.”
- Over time, we can talk about how to ramp up your exercise with the goal of getting 150 minutes (2.5 hours) each week. Go out hiking once or twice a week.
- Surroundings
- If needed, you can ask at your local senior citizen’s center for help with your wife’s flowerbeds, or offer to pay your grandson to help.
- Set aside time at least once a week to tidy up your house.
- Personal Development
- Take those photography classes you have been wanting to take.
- Get out to church or to the senior center at least once a week.
- Food and Drink
- “Starting next Monday, I will focus on Food and Drink by eating a salad or a vegetable dish every day. I will know I am successful if I can lose a pound every 1 to 2 weeks. I will continue to modify this goal by checking in weekly with the nurse case manager.”
- Follow up with your dietitian as scheduled. Ask her about the MOVE! program.
- Family, Friends, and Co-Workers
- Keep fishing with your grandsons. If you are up for it, try to give your brother a call and reestablish connection.
- Spirit and Soul
- You lit up talking about your photography. Be sure to keep it up. Display some of your work at that gallery that was interested.
- Continue to pray. A Bible study group might be a great way to get more social contact and help you feel more spiritually connected.
- Power of the Mind
- Keep following through with your counselor and psychiatrist for the work with your PTSD.
- As we agreed, we can talk about this more in the future. Talk with your counselor too.
NOTE: The SMART goals for Moving the Body and Food and Drink were added to give you some additional examples. You would not necessarily suggest all these SMART goals at the same visit.
Professional Care: Conventional and Complementary
- Health Concerns
- Blood pressure is up today—150/90.Start that new blood pressure medication. Return for a recheck in 2 weeks.
- We can talk next time about other options for Gastroesophageal Reflux Disease (GERD).
- Prevention/Screening
- Follow up with the cholesterol tests and A1c as scheduled.
- Vaccinations are up to date
- Treatment (e.g., conventional and complementary approaches, medications, and supplements)
- Continue medications as prescribed. Refills are ordered.
- Chiropractic is fine to continue, but I would be cautious with intensive approaches where a lot of force is applied to your lower back.
- Always feel free to ask questions about complementary therapies you read about.
Referrals/Consults
- Already scheduled with your dietitian and psychiatrist
- See a physical therapist—referral done
- Set up a Whole Health Coaching visit
- Referral for sleep study as discussed
Community:
- Get active with your local senior citizen’s center.
- Consider teaching a photography course at the local VA.
- Consider joining the gym at the YMCA.
Resources:
- Review the Veteran handouts on Healthy Sleep.
- Consider trying abdominal breathing, to relax. You have the handout.
My Support Team
- Principal Professionals
Primary Care Clinician
Whole Health Coach
Personal Trainer
Dietitian
- Personal Support Team
Your daughter, JoAnne
Your buddy, Roger
Next Steps
- Read the handouts we printed out for you.
- See the CBT-I psychologist. Download the app.
- Set up a visit with a Whole Health Coach within 1 week.
- See your dietitian and discuss the MOVE! program.
- Follow up with sleep study.
- See me again in 2 months. Return for nurse blood pressure check in 2 weeks after you start the new medication.
- Complete your living will and power of attorney, as discussed.
NOTE: Some of these sections are redundant. Again, use the PHP templates as a tool. Only complete the sections that are relevant to the specific visit.
After the Whole Health Visit: Documentation, Billing, and Future Visits
Bob has a PHP and follow up plan. There are a few other important aspects of practicing Whole Health that must occur after Bob’s visit is over. Clinicians need to be able to document the visit in the EHR and bill appropriately. It may also be important to make mental note of other areas to discuss with Bob in the future.
DOCUMENTATION
Generally, it is helpful to follow a template when you create a note about your visit. The Brief Personal Health Plan Template is increasingly used through the VA to provide a summary of the visit for the Veteran, but unfortunately, there is not yet a single template that is widely available for documentation. So far, different facilities have different ways to document Whole Health visits. Numerous sites are experimenting with different options. For example, some sites have created a specific tab in the EHR where all Whole Health documents are housed. Others have a specific way to enter the data from the Brief PHI. Check with your site to learn what protocols, if any, are in place.
Bob’s Whole Health note could look similar to the PHP shared previously. However, it may also follow a much more standard note with enhanced versions of different sections. Refer to the tool, “The Whole Health Note: Beyond the Standard History and Physical” for additional insights.
IDEAS FOR FUTURE VISITS
As Bob’s clinician documents the visit, it helps to take note about other areas he or she (or other colleagues) could discuss with Bob in the future. For example,
- Bob’s photography is important to him. You could explore this in more detail. Hobbies and skills are an important aspect of the Personal Development circle.
- At some point Bob was an avid walker. A SMART goal addressing walking might be something to discuss in the future, as part of the Moving the Body self-care circle. Using a pedometer might be helpful.
- Bob might eventually be interested in joining the MOVE! program.
- Bob’s PTSD may need to be addressed in greater depth, and it will be important to watch for his consult note with his psychiatrist. Bob had mentioned hearing that acupuncture might be useful for PTSD and would like to try it in the future. You can pursue this later on, after he has tried other items on his PHP, like the CBT-I for an agreed-upon period of time.
- You might mention the local mindful awareness class again, provided that his psychologist concurs. This may help with his PTSD, and it will certainly support him in other ways as well.
Conclusion
This overview and its supporting materials are intended to help you implement Whole Health into your practice. Keep asking yourself how you can incorporate elements like an Elevator Speech, MAP, the PHI, questions related to various aspects of the circle, the Key Principles of Personal Health Planning, and various steps for follow up. Experiment, and figure out what works best for yourself and the rest of your team. Clinicians who have been doing Whole Health visits for the past few years report that they have better insight into their patients, find their work more fulfilling, and have received a lot of positive feedback from their Veterans.
Finally, don’t forget that one of the most important aspects of implementing Whole Health is to apply it in your life. Be sure to complete a PHI and PHP for yourself, if you have not already done so, and take a look at “Implementing Whole Health in Your Own Life: Clinician Self-Care.”
Whole Health Tools
Author(s)
“Implementing Whole Health in Your Practice” was written by J. Adam Rindfleisch, MPhil, MD, (2014, updated 2021).



















