Passport to Whole Health: Chapter 1
Chapter 1. Whole Health: An Overview

Never doubt that a small group of thoughtful, committed, citizens can change the world. Indeed, it is the only thing that ever has.
―Margaret Mead
Health care systems are dynamic. New scientific discoveries, new illnesses, patient demands, and social change keep them constantly evolving. There is a national—and international—movement underway to evolve health care into something that is more personalized, proactive, and patient-driven, offered by clinicians who are energized and fulfilled by their work.
Thousands of health care professionals worldwide have set out on a journey of discovery, exploring new models and approaches that are inclusive, respectful of patients as individuals, and informed by the evidence. In the VA, the Whole Health approach is an answer to the call for ongoing improvement of the care offered to our nation’s Veterans.[4] It has rapidly gained momentum; leaders and teams from facilities nationwide are exploring the possibilities Whole Health offers. How can each clinician, staff member, leader, volunteer—all of us—contribute to a system that offers the best care possible?
A passport symbolizes the beginning of a journey. It enables a person to explore new territory. Like any passport, this Passport to Whole Health reference manual is designed to help you embark on new experiences, offering an opportunity for you to explore new ways of doing your work, caring for others, and even taking care of yourself. Ask yourself three key questions:
- Where do you want your work in health care to take you?
- How do you help your patients get to where they want to be with their health, based on what matters most to them?
- How can you align how you practice with the reasons why you went into health care in the first place?
This reference manual offers potential answers.
What Is Whole Health?
"Whole Health, also known as ‘Personalized, Proactive, Patient-driven Care’ is an approach to health care that empowers and equips people to take charge of their health and well-being and to live their lives to the fullest."[5]
Whole Health is built on the principles of Patient Centered Care, which includes "qualities of compassion, empathy, and responsiveness to the needs, values and expressed preferences of the individual patient."[6] Positive interpersonal interactions, healing relationships, and technically-skilled care are also key elements. Whole Health recognizes the importance of these elements and elaborates on them. At its core, Whole Health:
- Centers around what matters most to each Veteran. Whole Health is values-driven, and everything is built upon a person’s mission, aspiration, or purpose (MAP) in life.
- Personalizes care. Care is put into the context of each person’s life, and his or her specific aspirations and goals are given central importance. Care accounts for factors such as a person’s medical conditions, genome, lifestyle, needs, and social circumstances.
- Is proactive, focusing not only on what is wrong, but also on prevention and self-care. The goal is a future of well-being, joy, and vitality that involves much more than the management of problems once they arise.
- Is patient driven. The patient is the leader of his or her care team. They are an active participant in personal health planning, guiding the care they receive. The best possible outcome is alignment of an individual’s health care with their immediate and longer-term life goals. The patient is the source of control, and care is based on his or her needs and values.
- Is built upon relationships between patients and their care teams. Health care professionals, family members, peers, and other members of the patient’s community and social network offer support at many levels.
- Focuses on unlocking the body’s innate ability to heal. This holds true no matter what a person’s condition might be, and it goes beyond simply making diagnoses and managing diseases.
- Is holistic. Whole Health is about the whole person; it is inclusive of every aspect of who a person is—body, mind, spirit, and relationships with others. Physical well-being is important, but it is just the tip of the iceberg.
- Applies to clinicians as well. Clinicians are encouraged to apply the Whole Health approach to their own lives. Their well-being matters in and of itself, and healthier clinicians who role model healthy behaviors have healthier and more satisfied patients. For more information, go to "Implementing Whole Health in Your Own Life: Clinician Self-Care" in the Whole Health Library.
- Is evidence-based. Medical literature is respected and given full consideration, as are other sources of understanding patients value.
- Is inclusive of an array of skills, tools, people, and programs. Whatever is safe, effective, and consistent with patient preferences can support Whole Health.
The shift toward Whole Health is a movement supported by national VA leadership. It is also a grassroots movement, advancing with one VA employee at a time, as individuals explore how the Whole Health approach fits into their work environment and their personal lives. Whole Health has evolved through the efforts of clinicians from a variety of backgrounds—dieticians, doctors, nurses, pharmacists, psychologists, MSAs, social workers, Whole Health Partners, chaplains, Whole Health Coaches, occupational therapists, physical therapists, recreational therapists, complementary health practitioners, and many others. Thanks to Whole Health, many of these dedicated individuals are connecting more with why they chose to go into a health care profession in the first place. How might Whole Health help you find even greater fulfillment in your work with Veterans?
What Whole Health Is Not
Over the years, as Whole Health has gained more footing within VA, some confusion has arisen about how Whole Health fits into larger framework of the VA health system. As you explore how Whole Health might inform your work and self-care, keep the following in mind:
- Whole Health is not a separate program. Whole Health is an overarching approach to care. While sites may be hiring Whole Health team members or adding space for Whole Health-related offerings, Whole Health is not limited to just those people or just that space. The goal is to weave Whole Health into every aspect of Veteran care, building bridges and removing siloes that limit optimal team function.
- Whole Health includes, but is not limited to, offering complementary and integrative health (CIH) approaches to Veterans. This is especially now that multiple CIH approaches are covered in the VA as part of the benefits package, and the VA Integrative Health Coordinating Center (IHCC) has been a vital component of the VA Office of Patient Centered Care and Cultural Transformation (OPCC&CT) for several years. Whole Health is often equated to offering services like acupuncture or tai chi, but that is only part of what Whole Health encompasses.
- Whole Health builds on the great work done as part of other VA efforts. Programs like those conducted through Health Promotion Disease Prevention, Nutrition and Food Services, VA Chaplaincy, and Office of Mental Health Services synergize beautifully with Whole Health. Whole Health and Employee Health are closely connected too.
- Whole Health is not a "trend" or the "flavor of the day." Whole Health programming has been ongoing in VA since 2011, and it has rapidly expanded. From 2013 to 2021, over 63,000 VA employees took a Whole Health course in person or virtually, and another 53,000 took asychronous online courses.
- Whole Health is featured prominently in the VHA FY2022-2028 Strategic Plan; strategy 2.2 focuses on "VA and partners tailor the delivery of benefits and customize whole health care and services for the receipient at each phase of their life journey."[7] VHA’s long-range goals are aligned with overall VA goals for improvement and modernization of Veteran health services and strengthening VHA as a high-reliability organization, which includes delivering comprehensive and integrated Whole Health care. Coding data indicates that Whole Health encounters increased from 342,000 in FY16 to 616,000 in FY18 and 957,000 in FY19.
- Whole Health is for everyone. At its best, Whole Health is for all people on this planet, broad enough to embrace all expressions of being human. To this end, Whole Health includes the diversity and richness of cultural, financial, and social experience. Diversity is fundamental and vital, like the air we breathe and the water we drink, and it is encompassed by a Veteran’s MAP. Not only does it reflect a Veteran’s aspirations for his or her own physical health, but it can also take the form of an immediate or practical mission (e.g., "finding safe and stable housing" or "paying my bills") and include exploring broader life dreams. The key is to honor who each person is and how they f eel the Whole Health approach can best serve their specific needs. That is the essence of personalized care.
Why a Whole Health System?
We hear about it more and more all the time: Modern health care is faced with a number of challenges. Some of the most serious ones include the following:
- Mortality rates. Despite all that we spend on health care in the U.S., we do not do well compared to other countries when it comes to mortality rates and other health measures.[8] When it comes to average life expectancy, the United States ranks 28th out of the 36 countries that are members of the Organisation for Economic Co-operation and Development.
- Chronic disease. Chronic diseases are on the rise. Over 60% of American adults have a chronic disease, and 40% have two or more.[9] 7 out of every 10 deaths in our country are due to chronic disease.[10] However, the "find it-fix it" model of medicine does not work well with these disorders. If you are treating strep throat, you can diagnose it with a lab test and prescribe an antibiotic, and typically the problem is solved. In contrast, if you are working with someone with a complex combination of diabetes, obesity, high blood pressure, depression, and irritable bowel syndrome (IBS), it may not be in the patient’s best interest to treat each condition in isolation, especially not with medications that interact with one another.[11] Treating chronic conditions requires more time, effort, and collaboration among health care team members.
- Lack of Prevention. Many of the chronic problems we see are preventable. The U.S. Centers for Disease Control estimate that 20-40% of the 900,000 deaths each year that were related to the top five causes of death were preventable.[12] 50% of adults are not meeting physical activity requirements, 90% of people over age two eat too much sodium, 15% of Americans smoke, and 1 in 3 Americans have cardiovascular disease, which is closely linked to unhealthy behaviors.7 However, it is not easy to get people to change their behaviors. For example, it is estimated in some studies that as many as half of patients (or more) do not take their medications as prescribed.[13] For many chronic diseases, adherence to prescriptions drops even more, to the 20-30% range.[14]
- Clinician burnout. Burnout among health care professionals is occurring at an alarming rate. Over 40% of nurses,[15] 39% of social workers,[16] 60% of psychologists,12 and over 42% of physicians (may be as high as 54%, depending on specialty)[17] meet criteria for burnout. Burnout rates in the VA may be a bit lower than the national average, but in a 2018 survey of over 86,000 VA employees, fewer than half met the criteria for being fully "engaged."[18] The highest burnout rates were in administrative staff. Burnout is linked to depression, substance use disorder, and lower-quality patient care. Some surveys indicate that physician burnout has dropped slightly in the past 5 years.14
- Patients are voting with their feet. Well over a third of American adults use CIH approaches, but over 40% of people who use them do not disclose this to their health care clinicians.[19] A study of 401 Veterans with chronic, non-cancer pain found that 82% were using CIH.[20] Mounting evidence supports some approaches as safe and effective ways to work with challenging health conditions. (Chapters 14-18 feature more information on CIH.) More broadly, a 2019 survey of 1395 Veterans from the 18 Whole Health Flagships found that 97% of respondents were "Very Interested" or "Somewhat Interested" in Whole Health or already using it.
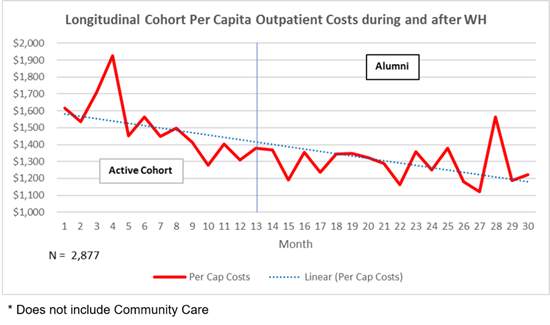
- Costs of health care. Data from 2019, shows the fiscal benefits for using Whole Health, as noted in Figure 1-2.
But, imagine…
What would your practice be like if you could overcome some of these challenges? Answer the following questions:
- What if it were possible to offer better care, perhaps with fewer resources being spent on diagnostic testing, procedures, and medications? This is not to say those elements of modern medicine do not have a role, but what if it were possible to be more strategic about their use?
- What if your patients were more empowered, acting as co-creators of their own health plans?
- What if you could work more effectively with a larger, transdisciplinary team to support each patient’s needs, and what if your patients took the lead in co-creating that team?
- What if you could, as you felt comfortable, help your patients use CIH effectively, or at least provide informed guidance to your patients about their use? And what if those services were actually offered to Veterans at your facility? What if you could add an approach to your toolbelt by taking a VA-supported training?
- What if you could feel more invigorated by your work, with greater resilience and a lower risk for burnout?
The Whole Health approach is not a cure-all for our health care system’s many ills, but it represents a shift in perspective that has been well-received by thousands of clinicians nationwide, in VA facilities and beyond. It leaves room for innovative ideas and new perspectives on how to engage with patients. Whole Health is a way to work with chronic disease, and to develop a more comprehensive approach. When all is said and done, it can help us to surmount the challenges we currently face in health care.
As you explore Whole Health in your practice, the number of available tools and recommendations you can offer grows. More importantly, you are likely to find it enriches your practice and makes your work more enjoyable. It may also help you to make positive changes when it comes to your own health. No one pretends to have all the answers, but the Whole Health approach serves as a jumping-off place for searching for them.
The Circle of Health
The Circle of Health, featured below in Figure 1-3 and full size on the first page of this manual after the front cover, offers an overall perspective on the many important aspects of health and well-being. It draws in all the personal, professional, and community resources that can support each individual. Known more formally as the "Components of Proactive Health and Well-Being," the circle is a visual representation that can be used by clinicians and patients alike to conceptualize all that Whole Health encompasses. The Circle diagram enables a person to see, at a glance, what might inform a Veteran’s PHP. It is something you can show a patient during a visit as a way to help them choose where they want to focus on in order to reach their goals.
As the "equation" across the bottom of Figure 1-3 shows, there are five key parts of the Circle of Health. These include:
- "Me" at the Center. Whole Health accounts for each individual’s story and uniqueness. Patients are invited to explore what really, really matters to them—their life aspirations, not just their symptoms. That exploration guides goal setting for their care. To make a change, people have to be aware of what they need. An important aspect of putting "Me" at the center of the Circle of Health is the development of a PHP for each patient. The PHP is co-created by the patient and the care team. Even people with the same list of health problems will have very different goals and ultimately, very different PHPs to help them reach their goals. Chapters 2 and 3 describe what the Whole Health Clinical Care Journey is and suggest ways to bring it more fully into practice.
- Mindful Awareness. Note how the "Me" circle is surrounded by "Mindful Awareness." Central to mindful awareness is the ability to be fully aware and present in a non-judgmental way. This means noticing symptoms, as well as noticing our behavior and thought patterns, and how they affect our health. Mindful Awareness is discussed in Chapter 4.
- Self-Care. Whole Health emphasizes the power of each individual to shape his/her health. Each of us has the innate capacity to heal, if only we are empowered to do so. Even people who cannot be cured, who cannot make their diseases go away, can experience a deeper sense of meaning, peace, joy, or comfort. Take a few minutes to look at the eight small circles within the larger one that immediately surrounds "Mindful Awareness." Every one of those eight aspects of self-care can be explored, individually or in tandem with others. The elements of self-care are featured in Chapters 5-12.
 Figure 1-3. The Circle of Health
Figure 1-3. The Circle of Health - Professional Care. While self-care is fundamental, all of us also rely on the support of others, including our team of health care professionals. "Professional Care" is the focus of the next circle out from the "Self-Care" circle. Prevention and treatment are central to professional care and include both conventional medicine and CIH approaches. Chapter 13 discusses prevention while Chapters 14-18 focus on various aspects of professional care, with an emphasis on CIH, since that is typically what is least familiar to VA clinicians.
-
Community. Finally, encompassing all the other parts of the Circle of Health is the outer ring, "Community." Community refers to the spaces in which we live, the resources we have available to us day-today, and our relationships with others in our broader environment. It includes where a person lives, works, and worships, and more. It includes all the people and groups a person connects with; it is everyone a Veteran relies on, as well as those who rely on him or her in return. Community also connects with social and structural determinants of health, such as education, socioeconomic status, and access to care. From public health to health policy to quality improvement initiatives, many different factors shape health beyond the personal level. Leaders in a facility create the space and opportunity for Whole Health to happen. Just as there is a "Whole Me" at the center of the circle, there is a "Whole We" that enfolds it. This "We" can extend beyond individuals to social services, support groups, neighborhoods, culture, religious groups, Veteran organizations, and local and national health care systems. Chapter 19 explores this fundamental aspect of health care.
All of these different components of the circle are aspects of Whole Health. Focusing on any one of them can enhance Whole Health for both clinicians and the Veterans they serve. The parts of the circle are interconnected; working on one area will often lead to growth in other areas of the circle as well.
Typically, when people review this information, they realize that they already bring some aspects of the Whole Health approach into their work. The question becomes, how can they incorporate the Whole Health approach even more fully? Which of the following are you and your colleagues doing?
- Using Personal Health Inventories (PHIs)
- Mapping to the MAP (Mission, Aspiration, Purpose)
- Empowering Veteran self-care
- Honoring your own self-care needs
- Bringing forward your best therapeutic presence
- xpanding your toolbox to include additional resources, tools, and well-being approaches
What else might you do to bring Whole Health into the picture? (Chapters 2 and 3 will describe these elements of Whole Health care in more detail.)
What Does Whole Health Look Like in Practice?
After hearing about Whole Health, clinicians inevitably want to know what a visit looks like in practical terms. How can it be implemented? There is no single way to practice Whole Health, but there are key elements that arise in all Whole Health practices. Consider some of the following examples of models being explored by various VA facilities:
- In some facilities, new enrollees into the VA health care system are invited right away to start on the Whole Health Pathway. They experience personal health planning, assemble their Whole Health team, and make detailed plans for follow up even as they are given support with their medical problems. Their experience may be supported by a Whole Health Coach or a Whole Health Partner, who can guide them through the process of exploring what really matters, setting goals, and beginning to create a PHP. This begins even before they seek clinical care.
- At some sites, people with difficult-to-treat chronic pain syndromes are referred to a Whole Health pain group, where they participate in shared medical appointments focused on various Whole Health topics. In addition, they have access to a variety of different CIH services, and their PHPs incorporate self-management and other elements tailored to each individual’s needs. The primary care team works with other team members to optimize Veteran self-care.
- In multiple VA sites, every member of a Patient Aligned Care Team (PACT) becomes involved in Whole Health care, most commonly when Veterans come in for physical examinations (wellness visits). PHIs might be collected, shared goals and/or SMART goals are often outlined, and a PHP may be developed. The entire team participates, from the person who introduces the Veteran to the Whole Health model for the first time, to the LVN or LPN who rooms patients and asks what matters most to them, to the RN who calls to check in on their progress a few weeks after they are seen. Whole Health Coaches and Whole Health Partners—specially trained Veteran colleagues—are also team members in many facilities. (These roles are described in more detail later in this chapter.)
- Inpatient services, domiciliaries, and palliative care groups are helping Veterans in their care to create and implement PHPs as well.
A New Normal
Consider what would happen if a health care system offered the following, not as unique experiences, but rather as the standard of care. As a patient, you would experience the following:
- You are seen as more than your list of health problems. Your team knows your story and what matters most to you, and that information is well documented in the chart.
- You are the captain of your own Whole Health care team, which you helped to co-create. Your clinicians are like your first mates; they offer guidance, updates, and support as you steer the ship.
- You are highly ‘adherent’ to treatment recommendations because you trust your team, and you helped to outline what the treatment will be.
- The clinicians and staff who serve you are role models for Whole Health themselves and are at low risk for burnout. There is less staff turnover and a higher likelihood you will have continuity with your team over the long term.
- Your clinician is rewarded for offering Whole Health, because care metrics have shifted to place higher value on aspects of care such as empathy, collaboration, and self-care. Funding mechanisms are in place to support all of this as well.
- You can take for granted that your clinician can openly discuss a wider range of self-care topics such as your spirituality, relationships, surroundings, and CIH experiences.
- Your clinicians document all aspects of your Whole Health care, including your PHI, in your medical record using the Personal Health Plan template. Other members of your team do the same. This information informs your entire team, and guides all your conversations about your care, ranging from a meeting with a pharmacist, to a follow-up call with a nurse, to a formal consultation with a specialist or a visit with a CIH practitioner. You can now use a national CPRS Personal Health Plan Template Educational Overview to help with this.
- Your care takes place in an optimal healing environment, where even the artwork on the walls, the music in the background, and the magazines in the waiting rooms are health-promoting.
- Communication is consistently impeccable, with all the members of your team offering you empathy and genuine compassion.
For more information, check out the following overviews, featured on the Whole Health Library website: "Whole Health in Your Practice, Part I," "Whole Health in Your Practice, Part II," and "Whole Health in Your Practice, Part III." Part I focuses on personal health planning, Part II on clinician therapeutic presence, and Part III on weaving CIH into your practice.
The aspects of Whole Health care described in this chapter are becoming a reality at sites across the country.[21] Fiscal year 2018 marked the launch of the full model in conjunction with the Comprehensive Addiction and Recovery Act (CARA) legislation, through the selection of 18 Flagship Facilities, one within each of VHA’s Veterans Integrated Service Networks (VISNs). These Flagship Facilities participated in the first Whole Health Learning Collaborative, a successful 18-month process through which sites received a comprehensive Implementation Guide, education and training, resources and tools, and onsite support. A 2020 report on the outcomes for the 18 VA Whole Health flagship sites, which have now been incorporating Whole Health for the past 3 years, found that[22]:
- There was a 193% increase in use of Whole Health services by Veterans with chronic pain, 211% for those with mental health diagnoses, and 272% among those with chronic conditions in general.
- Those who used opioids for chronic pain reduced them three times as much if they used Whole Health services. Use decreased by 38% (versus 11%) in those who were comprehensive Whole Health users (people who had at least 8 visits including both core services and CIH).
- Preliminary findings (based on early findings over 6 months) indicate that self-reported health and well-being outcomes improve for those using Whole Health services.
- People are much more likely to see their care as more patient centered, to be more engaged in their care, and to be more engaged in their lives as a whole.
- Pharmacy costs seem to decrease, at least to a small degree.
- Employees who are involved with Whole Health report greater motivation, lower voluntary turnover, and lower burnout.
- Higher employee involvement with Whole Health is linked to higher ratings of hospital performance (e.g., SAIL measures).
During fiscal years 2016-2018, the OPCC&CT provided funding to 31 Whole Health Design Sites to develop various aspects of the Whole Health System model of care. A second Whole Health Collaborative commenced in June 2019 as part of the next wave of Whole Health expansion across the enterprise. Each VISN selected two additional sites to participate in this next phase of the rollout, for a total of 36 new sites. Thirty-seven new Whole Health Learning Collaborative sites have also been selected. The intent is that, eventually, all VA facilities will adopt a Whole Health System model. The link below maps out the locations of the Design and Flagship sites. Note that some Flagships were previously Design Sites.
What Does a Whole Health System Look Like?
The journey towards Whole Health transformation is more than changing workflows or completing activities. It is about changing behaviors to impact our system’s values and outcomes. The entire system of care must shift; we need nothing less than an entire Whole Health System of care. The Whole Health System Designation Framework describes the transformational journey sites can take in this direction, and outlines milestone accomplishments sites can achieve towards Whole Health transformation as they progress through four phases of implementation: Preparation, Foundational, Developmental, and Full. The framework describes key accomplishments across each phase and is organized around seven domains of focus: Governance, Operations, Pathway, Well-Being, Clinical Care, Employee Whole Health, and Community Partnerships.
The Designation Framework recognizes that how these accomplishments are achieved may vary from site to site, and that sites will work through Whole Health implementation at different paces. Key accomplishments are provided as outcome-type milestones with the intent to provide sites with the latitude and flexibility in how they choose to operationalize processes and practices along the Whole Health journey. The Whole Health Designation Framework was released in March 2019 along with VISN and site-level Self-Assessment Tools and posted on the OPCC&CT SharePoint Site.
There are three key aspects of the Whole Health System, as shown in Figure 1-4, below.
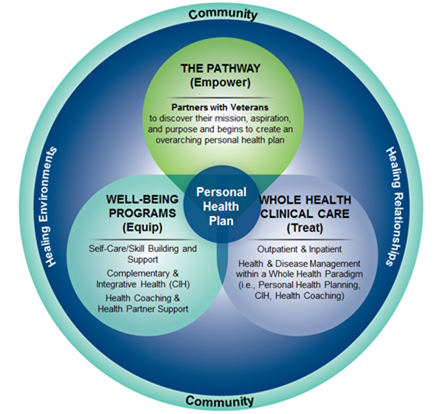
1. The Pathway: Empowering Veterans. Whole Health Partners, a new position in VA for non-clinical Veteran staff, can form a vital connection with fellow Veterans when they enroll and throughout their experience in VA. They facilitate other Veterans’ exploration of their mission, aspiration, and purpose and help them create an overarching PHP, as appropriate. Pathway programming can be offered in the VA or the community and can be inclusive of family and caregivers. To support this element of the Whole Health System, VA has created other staff roles as well. Non-clinical Veteran staff can also be trained to facilitate Whole Health courses for Veterans, including the Taking Charge of My Life and Health course. Whole Health Coaches also have specific position descriptions in VA, and many sites are now incorporating them into Whole Health care teams. Note that Coaches and Partners also play a key role within Whole Health Well-Being programs. Table 1-1 summarizes these roles, as well as their required training and the tasks they perform.
2. Well-Being Programs: Equipping Veterans. Through this aspect of the Whole Health System, Veterans are equipped with the skills training and tools they need. This includes self-care practices, skill building, and CIH approaches. Thanks to collaborations between the VA’s IHCC and a number of other VA program offices, Veterans have increased access to a variety of services. These include CIH approaches, such as acupuncture, meditation training, and therapeutic massage. Yoga and tai chi classes are also increasingly available. Veterans can be seen individually in support of their PHPs, but most services will be focused on cultivating self-care skills through ongoing classes and support. Sites may offer a series of classes that focus on a different aspect of self-care each time; the OPCC&CT has created skill-building courses for each of the eight areas to support such efforts. (These are featured in the Resources section at the end of this chapter.) Well-Being programs will be closely connected to Whole Health Clinical Care and Whole Health Pathway programming.
|
Role |
Provided By |
Training Required |
Primary Tasks |
|
Whole Health Partner (WHP) |
VA employees (ideally Veterans) who meet qualifications of WHP position description |
|
|
|
Whole Health Coach (WHC) |
VA employees who meet qualifications of WHC position description |
VA WHC Training (currently two 3-day trainings with practice in between) |
|
|
Facilitator, Intro to Whole Health |
|
2-hour virtual train-the-trainer session for OPCC&CT |
|
|
Facilitator, TCMLH |
|
3-day in-person train-the-trainer session from OPCC&CT |
|
|
Whole Health Mentor |
|
OPCC&CT Whole Health Mentor Course, a 2.5-day in-person training |
|
WH = Whole Health; OPCC&CT = Office of Patient Centered Care & Cultural Transformation;
TCMLH= Taking Charge of My Life and Health, VSO= Veterans Service Organizations. For all Whole Health Courses, visit VA Whole Health Hub SharePoint.
Veterans may choose to work with Whole Health Coaches individually or as part of a group, if Coaches are available at their site. The intent of coaching is to empower Veterans to identify and achieve their health and wellness goals. Veterans are encouraged to use their insight, mobilize internal strengths, optimally use external resources, and develop self-management strategies that support healthy lifestyle changes.[23] Qualitative data indicates that Whole Health Coaching training leads to positive changes at an individual and organizational level.[24] Health coaching has been found to improve chronic disease management,[25],[26],[27],[28],[29] and it is linked to improvements in quality of life, mood, and perceived stress.[30],[31] Research is promising, and more is still needed.[32]
3. Whole Health Clinical Care: Treating Veterans. In a Whole Health System, the Whole Health approach to care is offered in both outpatient and inpatient settings. Clinicians are familiar with the Whole Health model and how to draw from all elements of the Circle of Health as they support Veterans with developing and following through with their PHPs. In a Whole Health System, VA clinicians support Veterans as they strategize about their self-care. They provide them with the knowledge and skills they need to attain their health goals. Clinicians make use of whatever resources are most likely to be effective for an individual Veteran, whether it is counseling about self-care, coordinating CIH approaches, making referrals, doing procedures, or prescribing medications. The transdisciplinary nature of Whole Health requires that clinicians be in close contact with Whole Health Partners, Whole Health Coaches, integrative clinicians and, essentially, any and all of the members of a Veteran’s care team. Documentation in the Electronic Medical Record (EMR) supports this transdisciplinary approach.
In a Whole Health System, VA clinicians are able to offer Whole Health to Veterans with full support from the entire VA chain of command. They are supported in their own self-care efforts as well, with the recognition that caregiver well-being is also highly valued in and of itself, with the added benefit that healthy clinicians are able to provide better care as well. To learn more, and gain a sense of what a Whole Health System might be like for a patient, go to "Implementing a Whole Health System: Patient and Team Perspectives" on the Whole Health Library website. Chapter 2 goes into more detail about the respective roles of Whole Health Partners, Coaches, and Facilitators.
 Whole Health Tool: Elements of Patient Centered Whole Health Care
Whole Health Tool: Elements of Patient Centered Whole Health Care
How are you doing with the key elements of Whole Health in your work? The following list of 22 questions was designed to help Whole Health team members evaluate what they are doing well in terms of offering Whole Health and ways they might make improvements. Many of the people who complete this questionnaire find they are already promoting Whole Health in a number of ways. As you continue to explore new ways to bring Whole Health into a practice, you can repeat this assessment and see how your answers change.
Every VA employee can be involved in this process to some degree. If you are not a health care provider/clinician, you could answer these questions from the perspective of one of the health care clinicians who takes care of you. How are they doing?
The elements featured below are by no means a comprehensive list, but they can get you started with reflecting about your work with Veterans.
Place a number from 1 to 5 in the space in front of each question, according to the following scale:
- Never Happens
- Occasionally happens—a few times a month
- Often happens—a few times a week
- Frequently happens—a few times a day
- Always happens—part of every patient encounter
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
|
________ |
|
Take a moment to review your answers. Which areas are your strong suits? Where would you like to make improvements? If you were to answer from the perspective of your own primary care provider, how would they do? You can choose any one of these areas and changes you would like to make. What support do you need from colleagues? From leadership? An important contributor to clinician burnout is not having control over one’s practice environment. How much control do you have over the different aspects of your practice listed above? What can be improved?
Time to Start Your Journey!
This chapter of the Passport to Whole Health manual has given you a sense of what Whole Health is and how it might look in practice. You have had a chance to think about where you are in terms of your own practice and where you would like to be. Consider your passport stamped. Where do you go from here? That’s entirely up to you! Read on for more ideas.
General Whole Health Resources
Websites
VA Whole Health and Related Sites
The VA Whole Health website offers a number of resources for a foundational understanding of Whole Health and various "Get Started" options. The dropdown menu in the upper left corner provides links to more in-depth materials for both clinicians and Veterans. https://www.va.gov/WHOLEHEALTH/
- Circle of Health. "Walk around" the Circle of Health accessing videos, handouts, online tools, and other materials on the eight components of self-care. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
- Whole Health: A Shift Towards Health. A nice introductory video, and a good one to show colleagues to introduce the concept to them. http://link.brightcove.com/services/player/bcpid4521574267001?bckey=AQ~~,AAACmABW4_k~,u3UC4vmaozkRbnTOHzovpplgn0QYiIND&bctid=5166690410001
- Evidence-Based Research. Includes all of the evidence maps mentioned in this reference manual.
- https://www.va.gov/WHOLEHEALTH/professional-resources/clinician-tools/Evidence-Based-Research.asp
- Veterans Whole Health Education Handouts. Reviewed by a national group of Veterans, as well as by VA clinicians. https://www.va.gov/WHOLEHEALTH/veteran-handouts/index.asp
- Whole Health Hub SharePoint. https://dvagov.sharepoint.com/sites/VHAOPCC/SitePages/Index.aspx
- Whole Health Education Homepage. Multiple additional links and printable resources. https://dvagov.sharepoint.com/sites/VHAOPCC/Education/SitePages/Home.aspx
- Whole Health Community of Practice Calls. People can join after taking the Whole Health courses. https://dvagov.sharepoint.com/sites/VHAOPCC/Education/SitePages/COPs.aspx
- Integrative Health Coordinating Center (IHCC). https://www.va.gov/WHOLEHEALTH/professional-resources/IHCC.asp
- Whole Health Implementation Guide.https://www.va.gov/WHOLEHEALTHLIBRARY/docs/WH-ImplementationGuide.pdf
- Health Promotion Disease Prevention. https://www.prevention.va.gov/
- Nutrition and Food Services. https://www.nutrition.va.gov/index.asp
- VA Chaplaincy. https://www.patientcare.va.gov/chaplain/index.asp
- Office of Mental Health Services. https://www.mentalhealth.va.gov
- VHA FY2022-2028 Strategic Plan. https://www.va.gov/oei/docs/va-strategic-plan-2022-2028.pdf
Whole Health Library Website
The Whole Health Library features an array of Whole Health materials written for clinicians and Veterans, all of which have been peer-reviewed. https://wholehealth.wisc.edu
You can use the search bar on the right or choose one of the tabs. Tabs include:
- The "Home" tab provides a general definition of Whole Health and features introductory videos.
- The "About" tab provides a more in-depth definition of Whole Health, how it began, and who is involved.
- Under the "Get Started" tab, you will find documents like the PHI, PHP, and the Passport to Whole Health.
- The "Implementation" tab has five overviews that present evidence-based approaches to implementing Whole Health in your personal and professional lives. Related Whole Health tools and additional resources are also available.
- The "Self-Care" tab has overviews that incorporate the latest research findings related to the eight areas of self-care and mindful awareness. Whole Health tools that can be used at point-of-care as well as resources are available for each overview.
- The "Professional-Care" tab has overviews that focus on applying CIH approaches and the latest research to treatment plans for specific conditions, such as men’s health, endocrine health, and cancer care. Related Whole Health tools that provide practical information for use at point-of-care and resources are available for each overview.
- The "Tools" tab has multiple resources clinicians can use at the point of care and provide greater detail about topics covered more generally in the overivews. Tools are listed in alphabetical order and may include topical resources (such as ‘asthma’) or details about specific strategies to apply Whole Health in your practice.
- Under the "Courses" tab, you will find manuals, PowerPoints, and additional materials for various Whole Health course offerings.
- "Veteran Handouts" contains peer-reviewed and Veteran-reviewed documents you can print for your Veterans. All relate to areas of the Circle of Health.
All of the materials can be read online or downloaded. In addition to materials related to the specific parts of the Circle of Health, there is an entire series devoted to pain and another focused on mental health. There are also materials that cover a range of body systems, including endocrine, cardiovascular, men’s health, women’s health, and the immune system.
Materials in the Whole Health Library website related to this specific chapter include:
- Implementing Whole Health in Your Own Life: Clinician Self-Care. Overview. https://www.va.gov/WHOLEHEALTHLIBRARY/overviews/clinician-self-care.asp
- Implementing Whole Health in Your Practice, Part I: What a Whole Health Visit Looks Like. Overview. https://www.va.gov/WHOLEHEALTHLIBRARY/overviews/part-i-what-whole-health-visit-looks-like.asp
- Implementing Whole Health in Your Practice, Part II: The Power of Your Therapeutic Presence. Overview. https://www.va.gov/WHOLEHEALTHLIBRARY/overviews/part-ii-power-therapeutic-presence.asp
- Implementing Whole Health in Your Practice, Part III: Complementary and Integrative Health for Veterans. Overview. https://www.va.gov/WHOLEHEALTHLIBRARY/overviews/part-iii-complementary-integrative-health.asp
- Implementing a Whole Health System: Patient and Team Perspectives. Overview. https://www.va.gov/WHOLEHEALTHLIBRARY/overviews/implementing-a-whole-health-system.asp
- Personal Health Plan Template. https://www.va.gov/WHOLEHEALTHLIBRARY/docs/Brief-Personal-Health-Plan-Template.pdf
- There are eight Whole Health for Skill Building courses for Veterans, one for each area of self-care in the Circle of Health. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp



















