The ultimate goal of Whole Health is system-wide transformation. A Whole Health System fully supports patient-centered care, which is often difficult to provide in the context of traditional visits. A Whole Health System emphasizes personal health planning, Veteran empowerment, and seamless care by transdisciplinary teams. It is supported by leadership at all levels. While staff member engagement may vary from person to person, the key is to have a critical mass of people at each VA site who are committed to making positive change happen. This commitment is needed at the individual and group (team) levels, as well as at the wider organizational level. It is also vital that Veterans be equally committed to this, since they are key stakeholders as well.
Key Points:
The Whole Health System includes 3 key elements:
- The Pathway. Veterans’ Whole Health experiences typically begin with the Pathway. Veterans are oriented to Whole Health and reflect on what will support their Mission, Aspiration, Purpose (MAP). They begin learning more about, and can choose to directly experience, different ways to care for themselves and seek care from others.
- Well-Being Programs. In a Whole Health System, Veterans have support to gain new self-care skills. They can take various classes, work with Peer Partners or Whole Health Coaches, and explore various Complementary and Integrative Health (CIH) approaches.
- Whole Health Clinical Care. Clinicians of all types—providers, nurses, social workers, psychologists, chaplains, pharmacists, physical therapists, and so on—weave the Whole Health Approach into their patient encounters. All the members of a transdisciplinary team support the Veteran with personal health planning.
Introduction
The Whole Health Approach can transform care at all levels. At the individual level, it can be applied to each Veteran’s (and clinician’s) self-care. Clinicians are encouraged to prioritize therapeutic presence and support the creation and implementation of Personal Health Plans (PHPs). It does not stop there, however. As an overarching philosophy of care, Whole Health can inform the function of teams, departments, facilities, and ultimately, the entire health care system. VA facilities all over the U.S. are exploring different ways to implement the Whole Health model at a system-wide level.
In the other Implementation overviews, the focus is on “Whole Health in Your Own Life,” “Whole Health in Your Practice, Part I,” “Whole Health in Your Practice, Part II, or “Whole Health in Your Practice, Part III.” This overview scales thing up, describing what it might look like for a Veteran to receive care within a Whole Health System. What additional value is there for a Veteran to be part of a VA facility where care at every level is personalized, proactive, and patient-driven?
The Whole Health System is introduced in Chapter 1 of the Passport to Whole Health. For a well-done video of what a Whole Health System can do, see the video, “Interactive Patient Care: Bringing Whole Health Care to Life.” To learn more about the specifics of the Whole Health System implementation after reading this overview, refer to the VHA Office of Patient Centered Care and Cultural Transformation (OPCC&CT) Whole Health System Implementation Guide.
Whole Health Systems: Three Key Elements
In fiscal year 2018, 18 VA sites—one from each Veterans Integrated Service Network (VISN)—were selected by VISN leadership to implement Whole Health Systems. These flagship sites, known as the “18 in ’18,” actively explored ways to advance Whole Health. In addition to hiring new personnel, they expanded the excellent work done previously by programs like the National Center for Health Promotion and Disease Prevention.
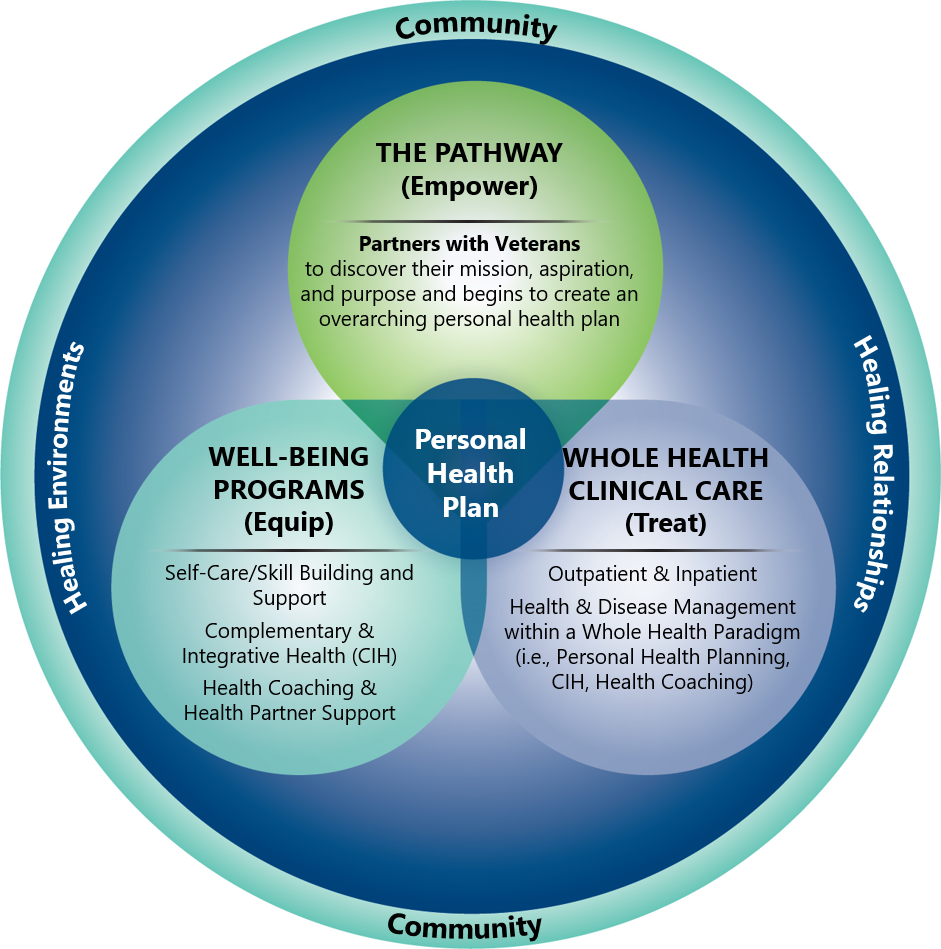
Figure 1. Key Elements of the Whole Health System
The design of each flagship site’s Whole Health System varies. However, there are 3 key elements that are part of the system, as shown in Figure 1. These elements include:
- The Pathway. Veterans, whether they are new enrollees or long-term recipients of care in the VA, can choose to learn about Whole Health and define their MAP whenever and however they would like.
- They may be encouraged to attend an orientation session focused on Whole Health, or to enroll in in-person or online course.
- As they follow the Whole Health Pathway, Veterans receive support as they begin to create a Personal Health Plan (PHP) built around what matters most to them.
- To learn more about the Pathway as part of the Whole Health System, refer to the video, “The Pathway to Whole Health.”
- Well-Being Programs. In a Whole Health System, self-care, skill building, and support are widely available.
- Veterans may receive additional support from Whole Health Partners or, Whole Health Coaches. These Whole Health team members have received additional training and/or certification related to guiding Veterans who are using the Whole Health Approach.
- Whole Health Partners are fellow Veterans who have received additional training focused introducing Whole Health to their fellow Veterans, helping them complete a Personal Health Inventory (PHI), and starting them on the process of deciding what they would like to focus on as their write their PHP.
- Whole Health Coaches use the coaching model to support Veterans with creating, and following through with, their Personal Health Plans. They can take Veterans through the various aspects of personal health planning and help them to set and achieve their goals. They can support Veterans as they follow up with clinical recommendations as well.
- In addition, various Complementary and Integrative Heath (CIH) approaches, many of which are now covered by the VA, are becoming increasingly available.
- You can learn more about Well-Being Programs by watching the video, “Skill Building to Promote Well-Being”
- Whole Health Clinical Care. A Whole Health System includes clinical care by specially trained clinicians from multiple service lines.
- This includes inpatient and outpatient providers; it relies on both primary care and specialty clinicians.
- To learn more, refer to the video, “Whole Health Approach to Clinical Care.”
- One key to successful Whole Health clinical care is a transdisciplinary team. It is necessary to shift the perspective away from thinking of clinical care as a series of isolated one-on-one encounters between a Veteran and their clinicians.
- Transdisciplinary teams encompass clinicians, patients and their loved ones, CIH practitioners, and others from throughout the community.[1]
- Teams are essential to the success of a Whole Health System, because one provider simply cannot implement the Whole Health Approach for all the Veterans in their care without support.
- Team members must communicate with each other seamlessly.As each Veteran moves through the Whole Health System, everyone on the team must be on the same page. If any member of the team sees a Veteran with a PHP, they take at least a few moments to discuss how things are going with it.
Bob: The Whole Health System From the Patient Perspective
The overview “Implementing Whole Health in Your Practice, Part I,” introduces Bob, a 68 year-old Vietnam Veteran, and provides an example of what a Whole Health clinical visit could look like for him. What would his experience look like from the broader perspective? That is, how would receiving care in a Whole Health System affect Bob as an individual?
FIRST ENCOUNTERS WITH THE WHOLE HEALTH SYSTEM: THE WHOLE HEALTH PATHWAY
Veterans can be introduced to Whole Health—and the Whole Health System—in a variety of ways. An established Veteran like Bob may first hear about it from one of his clinical team members, through taking a class, or because he asked for more information because of a poster or a website he saw. Veterans who are new to the system might be introduced to Whole Health during a new Veteran orientation program. Others may learn about Whole Health while participating in a VA Well-Being Program, like a mediation class, when the course instructor offers more information. As the VA Whole Health System Implementation Guide notes, “…any of the three Whole Health components/elements may refer a Veteran to one of the other components, and care will flow seamlessly amongst them.”
Once Veterans are familiar with what Whole Health is, they can decide how involved they would like to be with the Whole Health Pathway. The Pathway includes all the potential whttps://www.va.gov/WHOLEHEALTHLIBRARY/overviews/implementing-a-whole-health-system.aspays a Veteran can get started creating a PHP. First, they focus on exploring their MAP and completing a PHI. Then comes goal setting, along with seeking out the education, skill building, resources, and support needed to achieve their Whole Health goals. They may choose to start this process on their own, or to do it with support.
Bob’s highest priority on his PHP was improving his sleep (Recharge). Other self-care areas he wanted to focus on included Moving the Body and Food and Drink. Once Bob knew the general areas where he wanted to focus, he needed to zero in. It was time to learn more details and to experience some of the of options that could support him with implementing his PHP.
WELL-BEING PROGRAMS
Bob sought out programs that could equip him to more fully reach his goals. For example, he was drawn to mindful awareness after the clinician first mentioned it in the Whole Health Visit. He searched for more information online and selected two Veteran handouts to print out: “An Introduction to Mindful Awareness” and “Mindful Awareness Practice in Daily Living.” After reading them, he visited the Multimedia resources on the VA OPCC&CT website and downloaded several audio files featuring guided mindful awareness exercises. After he tried meditating and found it to be helpful, Bob signed up for a meditation class for Veterans, one of several well-being programs offered at his VA. He gradually ramped up to meditating 20 minutes a day.
Bob reviewed the list of other well-being services his VA covered. He signed up for a tai chi class, because he had read in the Veteran handout, “An Introduction to Tai Chi and Qi Gong for Whole Health,” that tai chi could help balance and leg strength. Since his most important goal was to be able to walk his granddaughter down the aisle and dance at her upcoming wedding, tai chi seemed like a good fit.
Bob was also pleased to learn that acupuncture was covered by the VA for treatment of chronic pain. His site offered Battlefield Acupuncture (BFA) sessions, so he signed up.
Bob was given the option of working with a Whole Health Partner (a fellow Veteran trained in guiding peers through personal health planning) or a Whole Health Coach to help him along with creating and implementing his PHP. He started to meet with a Coach every few weeks.
BOB’S EXPERIENCE: WHOLE HEALTH CLINICAL CARE AND TRANSDISCIPLINARY TEAMS
One of the remarkable things about a Whole Health System is that it helps a person implement a PHP. No one provider was expected to be totally responsible for Bob’s Whole Health; everyone on the team shared responsibility. Because Bob worked with a Whole Health Coach and clearly outlined his goals, it was easier for his clinicians to support him without having to invest a significant amount of additional time.
Over time, as he sought out the professional support he needed, Bob ended up being the captain of a large transdisciplinary team. Every member of the team was committed to Bob’s success. Bob confided to his primary care doctor that it was the first time in his life he had ever felt like his health care team truly cared about him on a personal level.
Bob’s PHP evolved with time. As Bob reached his initial goals—he was able to fully participate in his granddaughter’s wedding, for example—he set new goals to take their place. Every year or so, Bob completed a new PHI and shared it with his team.
Over the next 10 years, working within the Whole Health System, Bob started to find the right combination of self-care and professional care tools to help him with his various health needs. For example:
- Health care maintenance. Bob continued seeing his primary care team every 6 to 12 months for routine wellness visits and physical exams. He stayed up to date with his screening and diagnostic tests, as well as his vaccinations. A pharmacist on his team helped him keep track of his medications and supplements and how they interacted. Bob found that with more physical activity and some changes to his eating patterns, he was able to phase out some medications and decrease the dose of others.
- Metabolic syndrome. All of Bob’s metabolic syndrome issues markedly improved. He felt that was due to 4 things: 1) participating in the MOVE! Program, 2) being able walk more with the help of his physical therapist, 3) having a good response to acupuncture, and 4) taking a cooking skills course from a dietitian at a Healthy Teaching Kitchen. Bob was able to lower his doses of blood pressure and cholesterol pills, and his blood sugars normalized. He gradually lost 30 pounds. (For ideas on how to help someone like Bob with these challenges, refer to “Heart Health” and related Whole Health tools for more information, as well as “Type 2 Diabetes Mellitus” and “Achieving a Healthy Weight.”)
- PTSD. Bob continued meditating and followed up regularly with his mental health team. He received psychotherapy, including Prolonged Exposure Therapy, which reduced how often his PTSD symptoms were triggered. He tried several other mind-body approaches that were offered at his VA without additional charge, including guided imagery, clinical hypnosis, and biofeedback. Ultimately, for his PTSD, he found he favored breathing exercises and seated meditation over the other techniques. (Refer to “PTSD” for more information about how to apply Whole Health for this challenging chronic condition.)
- Depression and anxiety. Bob made sure he took his antidepressants without missing doses. He saw a psychiatrist who was skilled with the Whole Health Approach. Over the years, his episodes of suicidal ideation became less frequent, and he did some work with a therapist surrounding the complicated grief he experienced after he lost his wife. He continued to have “occasional ups and downs,” but found they were much easier to handle. (Refer to “Anxiety,” as well as “Depression” and “Grief” for more information on how Whole Health can help with these challenging mental health issues.)
- Chronic pain. Tai chi helped a lot with Bob’s balance and leg strength, and he continued to practice it a few times a week. His primary care provider had him start taking turmeric capsules, which eased his knee pain. For a period of about 3 months, Bob had Battlefield Acupuncture, which eased his chronic pain. With the support of his facility’s pain team, he created a pain self-management plan, and ultimately, it helped him reach a point where he felt he could manage his pain on his own without medications, acupuncture, or other interventions. (For more information, refer to “Chronic Pain” and “Self-Management of Chronic Pain.”)
- Irritable bowel syndrome (IBS). Bob’s gut symptoms steadily improved after his primary care provider had him take probiotics for a month. Doing so also seemed to help with his mood and PTSD. (Refer to “Irritable Bowel Syndrome” and “Promoting a Healthy Microbiome with Food and Probiotics” to learn more about the many ways gut function affects health.)
- Insomnia. Cognitive Behavioral Therapy for Insomnia (CBT-I), which was part of Bob’s original PHP, was helpful. Eventually, he was able to sleep 7-8 hours most nights. His sleep study was negative for obstructive sleep apnea, and with his weight loss, he stopped snoring. (Refer to “Recharge” and related Whole Health tools for more information on ways to improve sleep.)
- Tobacco use and COPD. Bob decreased his smoking to 1/3 of a pack daily, which helped his breathing. For COPD flares, he used the breathing exercises he learned from his meditation instructor. Every few years, he was given the “Tobacco Use Disorders” Whole Health tool. He never completely quit, but he kept trying.
- Alcohol use. It took several years, but Bob acknowledged that his drinking was a problem and agreed to see a substance abuse specialist in the VA. He enrolled in Alcoholics Anonymous and later became a sponsor. (Refer to “Substance Use” and related tools learn how the Whole Health Approach can help Veterans struggling with substance abuse.)
Many of the elements Bob incorporated into his PHPs over the years were not specifically intended to address one particular problem, and they had an effect on many different aspects of his health. Better sleep, more activity, improved stress management, and increased attention to Food and Drink (along with other approaches to self-care) can have benefits that extend beyond any one medical diagnosis. It was not necessarily that all of Bob’s problems were completely “cured.” Some were, but others did not completely go away. The key was that Bob’s quality of life and overall functionality improved. Whether Bob was cured or not, he experienced healing. He was empowered to take steps that would help him live his life more fully.
Bob received excellent patient-centered care through the Whole Health System. What were common threads that ran through his experience?
- His care was personalized. His PHP was specific to his needs and honored his values.
- His care was proactive. The focus was on more than simply playing the “defensive game” of responding to his health concerns after they arose.
- His care was patient-driven. Bob was the one mobilizing his team. He was in charge of his PHP; he decided where to focus and when. He also took classes, learned skills, and most importantly, understood the importance of taking care of himself. He acknowledged that he had to do his own work and could not simply be passive as others took care of him.
- He remained highly motivated. His team helped with that, by engaging him in his care.
- His care was evidence-informed. Bob was guided to follow a care plan that was supported by good research when possible. His longevity despite his multiple chronic issues was likely due to a combination of factors, including his connections with others, his spirituality and sense of purpose, his ability to stay active, his improved sleep, his decreased cardiac risk, his improved mood, and his ability to manage stress. The important thing was, his care included many different elements that could increase his longevity. No one will ever know how much each factor contributed, but the final outcome was good.
- Bob had a dedicated transdisciplinary team that communicated in-person, on the phone, and through medical records. The team communicated well with Bob and with each other.
The Whole Health Transdisciplinary Team
Whole Health Teams are vital to the successful implementation of a Whole Health System. As VA sites experiment with implementing Whole Health, clinicians must determine how they can best contribute, based on their training, skills, and scope of practice. Just as patients do when creating PHPs, clinicians must also ask what education, skill building and support they need to be effective Whole Health caregivers. How this looks will vary by person and by profession. For instance, one Whole Health Coach will do things differently compared to other Whole Health Coaches. They will also do it differently from a physician, advanced practitioner, social worker, pharmacist, chaplain, psychologist, dietitian, occupational therapist, or MSA. There is a richness in the diversity of practice styles that come into play.
The medical literature describes 3 general types of teams:[2]
- Multidisciplinary teams are groups of professionals working in parallel to support a patient. They do not necessarily communicate.
- Interdisciplinary teams are groups of professionals working together to address a common problem.Though their perspectives may remain separate, they work together more closely.
- Transdisciplinary teams work from a shared framework that links ideas from different disciplines. Each discipline’s unique expertise is honored, but team members let down professional boundaries. Transdisciplinary team members include professionals (including CIH practitioners), the patient, and the patient’s loved ones and various members of the community. Some experts hold that transdisciplinary teams are equipped to focus on real-world problems in ways other types of teams cannot.[3]
A Whole Health Team is a transdisciplinary team. Patients are active members of their team. They are the captains, essentially, and they choose the other team members. Bob’s team included his daughter, Whole Health Coach, primary care PACT members, acupuncturist, tai chi instructor, physical therapist, dietitian, psychotherapist, AA sponsor, and pharmacist. A number of his fellow Veterans were part of his team as well.
WHAT WE KNOW ABOUT SUCCESSFUL TEAMS
Over 15 years ago, the Institute of Medicine noted that high-functioning teams with representatives from multiple disciplines were one of the key elements of the 21st–century health care system.[4] While most research related to teams focuses on interdisciplinary teams, findings likely cross-apply for transdisciplinary teams as well. Some of the main research findings related to team-based care include the following:
- Functional teams are beneficial to patients and team members alike.[3]
- Patient outcomes improve.[5]
- Patient safety is enhanced—over 60% of sentinel events are linked to failures in inter-professional teamwork and communication.[3]
- Teams are more efficient when they work together, which results in increased cost savings and workforce retention, as well as reduced lengths of stay for patients.[6]
- Burnout risk is reduced for team members.[7]
- Effective teams have strong support at the organizational level.
- Team leaders create a positive atmosphere and motivate fellow team members. They focus on keeping the team high-functioning.
- Protocols encourage communication, routine meetings, and standardized (and efficient) ways to both document and find information in patient records.
- Members back each other up, to prevent any one person from being overloaded or at risk of making errors.
- The team is adaptable; members handle change well.
- Teams practice democratic decision making, so collective agreement is given higher priority than individual perspectives or biases.
- Members trust and respect each other.
- There is excellent communication. A meta-analysis of 72 studies across different industries found that information sharing was one of the best predictors of overall performance for the nearly 4,800 teams studied.[10]
- Team members have a shared understanding and a sense of camaraderie. Camaraderie increases when team members complete training together and see each other outside of the workplace at social gatherings.
- Team members break out of professional silos and hierarchies and are mindfully aware of any biases they might have. Successful teams effectively navigate their differences in perspective and use those differences to their advantage.
- Successful teams still function well even if they are spread out geographically. Having a Whole Health Partner or someone else who helps keep tabs on the overall Whole Health trajectory of a given Veteran is important; it is the equivalent of having a conductor who can bring an orchestra into harmony. Of course, the ultimate conductor is the patient, but it is important for them to have additional support keeping track of the many different aspects of their care.
Your Role in the Whole Health System
Take a moment to reflect on what you can bring to a Whole Health System. Ideally, everyone in a Whole Health System would have the skills and experiences necessary to confidently answer the following questions.
- Do you have a good general knowledge about Whole Health?
- Do you have an Elevator Speech? If not, you can learn how to create one in Chapter 2 of the Passport to Whole Health.
- Can you describe the various components of Circle of Health? Consider displaying a copy where you can see it regularly.
- Have you completed a PHI for yourself? You can complete the Brief PHI or spend more time and fill out the longer MyStory PHI.
- Can you list—and follow—the four “Key Principles of Personal Health Planning?” (These are featured in Chapters 2 and 3 of the Passport to Whole Health and in the overview, “Implementing Whole Health in Your Practice, Part I: What a Whole Health Visit Looks Like.”
- Which of the following roles can you play in a Whole Health System?(You will likely find that you are suited for more than one role.)
- Organizational leader (e.g., VISN lead or Pentad member)
- Department chair or head
- Care team leader
- Whole Health Team (e.g., Whole Health Program Manager, Whole Health Clinical Director, site Whole Health Point of Contact)
- Whole Health Flagship Education Champions or some other type of Whole Health instructor
- Group visit or shared medical appointment leader
- Provider of services related to one or more of the self-care circles (e.g., a dietitian might be a Food and Drink expert, or a social worker may help most with Surroundings or Family, Friends, and Co-Workers.Chaplains are a natural fit for Spirit and Soul).
- Provide CIH services or other Well-Being Programs
- Offer clinical visits that bring in personal health planning
- Set the stage for a Whole Health visit (may include welcoming a patient to the VA, rooming them)
- Orient new Veterans about Whole Health
- Be a Whole Health Partner or Whole Health Coach
- Contribute to Whole Health inpatient care
- Contribute to Whole Health outpatient care
- Provide Whole Health-focused domiciliary/residential care
3. Who else do you need on the team? It might be helpful to create a list of potential team members. Examples might include: Systems redesign, Clinical Applications Coordinator, Community Care, Health Promotion Disease Prevention Coordinators, and leadership, as well as any of a large number of different types of clinicians (e.g., providers, nurses, mental health, pharmacists, physical therapy, chaplains, social workers, etc.) and people from the community.
Each clinician, staff member, community provider, or other member of the transdisciplinary team will have something different to offer. Consider how your specific skills complement the skills of others on the team. There are a number of ways to build team dynamics, including CREW, TeamSTEPPS, National Center for Organizational Development, Relationship-Based Care, and others.
A Whole Health System is only as effective as the people who are part of it. As more people learn about the Whole Health Approach, “Whole Health care” will become synonymous with “VA health care.” Eventually, people will come to take it for granted that VA care always equates to “good care,” the kind of care that everyone should be receiving. In your role, whatever that may be, you can be an integral part of the transformation to a Whole Health System that offers everyone the best care anywhere.
Author(s)
“Implementing a Whole Health System” was written by J. Adam Rindfleisch, MPhil, MD, (2014, updated 2021).



















