Employee Spotlight
January 10, 2024
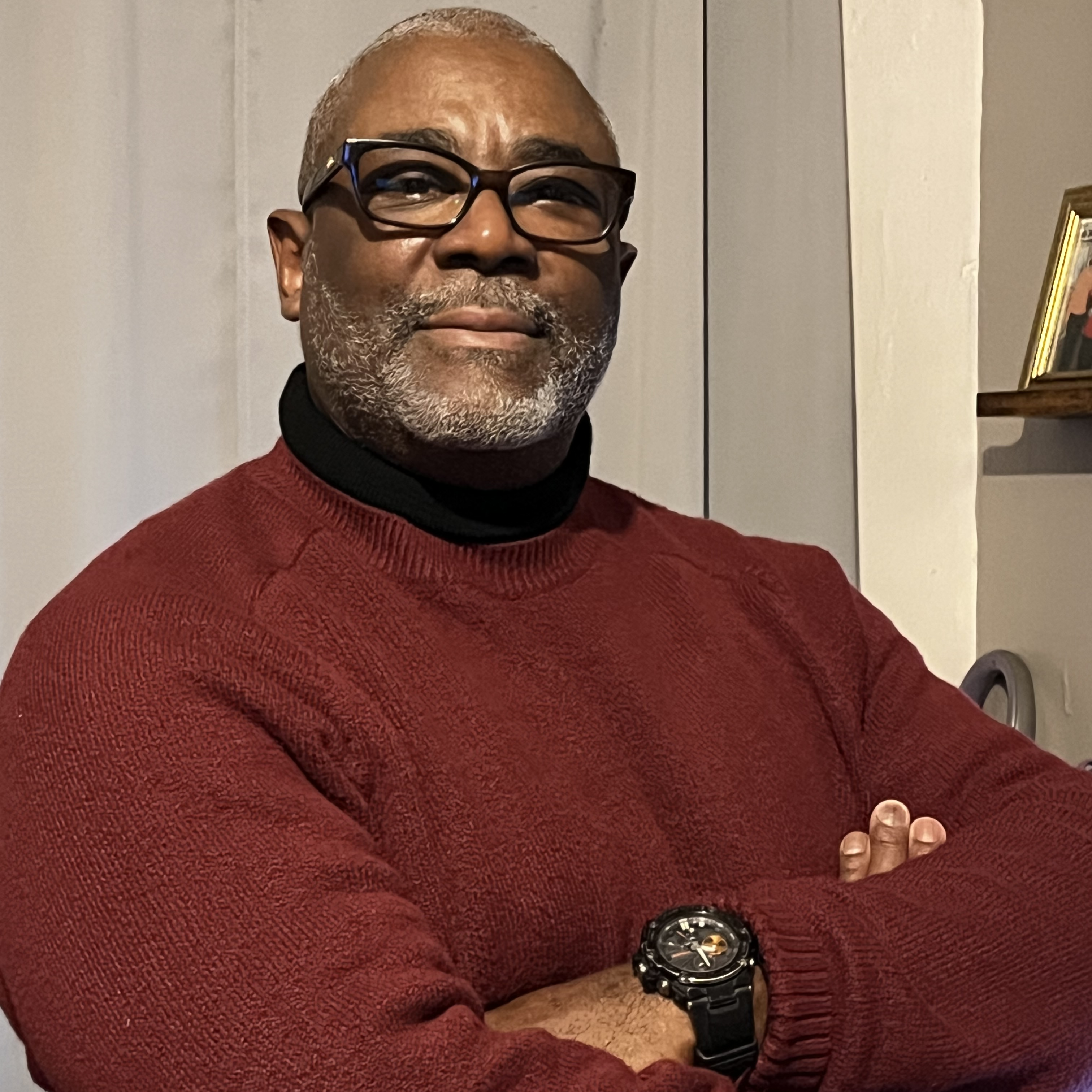
Peter Henry
Veteran Peer Support Specialist
VA New York Harbor Healthcare System
This year, we’re spotlighting VA’s Housing First approach through a series of interviews with VA employees and taking a look at how they’re working to end Veteran homelessness through this approach. Learn more about Housing First.
Q: What does Housing First mean to you, and what is your role as a peer support specialist?
A: Housing First is basically providing the services and housing that a Veteran wants, not forcing anything on them. It’s important that they have choice, because their housing can really affect other issues in their lives.
My job as a peer support specialist is to bridge the gap between the Veteran and a social worker or another practitioner, or between the Veteran and a family member. You know, letting them know that I’m a Veteran and I have some of the same circumstances. I understand their plight.
Q: Can you explain more about how you follow the Housing First approach?
A: We are the first Housing First Assertive Community Treatment (ACT) team in the Northeast. We are similar to an actual ACT team, but our primary focus is not mental health—it’s housing. I’d never heard of Housing First before this job, but now it’s what I do every day.
We really focus on giving Veterans what they want in housing. We’re bringing a lot of the services that are in the VA to the Veteran—whether it’s on the street, in the community center, or in their home. We let them know what our role is, what Housing First means to us, and what it means for them, and that’s how we proceed. We ask them, “What role do you want to play in this? Because you’re the one who’s going to be moving in.” When we speak to the Veterans with transparency, they feel better. They have more hope.
Q: Once a Veteran has moved into permanent housing, how do you assist in their recovery?
A: I believe, from my personal recovery, that you can’t treat one issue without treating others. We don’t only focus on housing. We put all the wraparound services and Whole Health in place. We try to utilize the systems that VA has in place—for example, our long-term substance use treatment programs. We reach out to those different programs and say, “Listen, we have this Veteran here who needs help. Do you have any open beds?” When we do that, we always get a great response. Unfortunately, some Veterans don’t feel as if they’re ready and, while it is frustrating, we just have to understand that’s part of their recovery process.
Q: How have you worked with Veterans who are facing challenging issues that could impact their housing stability?
A: There’s one Veteran that I have been working with for nine years. On the first of the month, he would owe his entire check because throughout the month he had borrowed more than what he gets in Social Security. It's hard, but not all Veterans we work with are able to manage everything that comes with housing, like handling their bills. Maybe they’ve never done that and need some extra support. With this Veteran, we worked with him to put a fiduciary in place to pay his rent and other bills related to his housing. Then they mail him his check. Now his biggest complaint about that is he doesn’t get his checks on the first of the month; now he gets them on the seventh or the tenth. But he can ensure that his housing is secure, which is the main thing.
I work with a Veteran in another borough who lives with paranoid schizophrenia, and because he doesn’t like the medication or the side effects, he won’t take it. It’s understandable that someone might make that choice, because the side effects can be pretty bad, but his mental health has deteriorated a lot. The property manager didn’t want us to call EMS, but as clinicians, we have to do what’s best for the Veteran. If we feel he needs to go see a doctor, that’s what we are obligated to do.
Q: How does being a Veteran impact your work?
A: As Veterans, we have a code that we understand. I meet them where they are. I don’t sugar coat it. If they’re wrong, I let them know. I think my listening to them, them listening to me, and us both being Veterans, they’re like, “OK, now we have this camaraderie.”
Q: Thank you for service. Can you tell us a bit about it?
A: I served in the Army from 1980-1986 at Fort Benning, Georgia; Fort Knox, Kentucky; and Kitzingen, Germany. I was infantry. Some of the weapons that they’re using today in Iraq and Iran, we tested those. I did some boxing in the military. It was a good time. My biggest regret was getting out.
Q: What is your reason for doing this work?
A: I’ve encountered so much working with these Veterans from their experiences in the military with substance abuse, trauma, wartime incidents, wartime injuries. I work with getting Veterans to open up about their military experiences. I’m a person that can help them—because I was in the military and I’m empathetic to their plight—open up about their experiences and start to heal. And that’s just special.
















