Attention A T users. To access the menus on this page please perform the following steps.
1. Please switch auto forms mode to off.
2. Hit enter to expand a main menu option (Health, Benefits, etc).
3. To enter and activate the submenu links, hit the down arrow.
You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links.
Locator
Contact
Search
Program Overview
The Minneapolis VAHCS Research Program, first established in 1946 and affiliated with the University of Minnesota Medical School, is one of the largest research programs in the VA system. The program supports the Minneapolis VAHCS clinical & education missions by:
- Helping to attract and retain outstanding clinicians
- Providing VA patients access to novel therapeutic modalities
- Regularly garnering positive media attention locally and nationally
- Discovering knowledge that improves the health and wellbeing of Veterans
- Generating VERA $ for the institution ($131.6 million from 2014-2023)
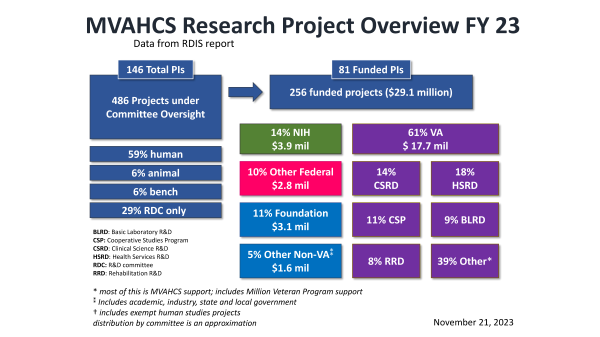
Program Metrics (FY2023)
- 140+ VA-affiliated investigators including 80+ funded VA-based faculty
- 250+ funded projects
- 445+ peer-reviewed publications
- Research expenditures ($29.1 million total) by funding source:
- NIH: $3.9 million
- VA: $17.7 million
- DoD & other federal: $2.8 million
- Other: $4.7 million
- Over 81,000 square feet of dedicated research space, including:
- Clinical research: 15,200 square feet
- Laboratory and preclinical research: 31,900 square feet
- Rehabilitaton research: 12,700 square feet
- Health Services research: 7,300 square feet
- Administrative space and storage: 13,900 square feet
Research Project Overview (FY2023)
Major Research Project Focus Areas
- Aging, Dementia, and Parkinson's Disease
- Brain Sciences and Traumatic Brain Injury
- Cancer Mechanisms, Prevention, and Treatment
- Cardiovascular Disease
- Health Care Delivery
- Pulmonary and Infectious Diseases
- PTSD and other mental health disorders
- Pain Management and Opioid Reduction
- Rehabilitation Medicine