Emergency Medical Care–Information for Providers
During a medical emergency, Veterans should immediately seek care at the nearest medical facility. A medical emergency is an injury, illness or symptom so severe that without immediate treatment, an individual believes his or her life or health is in danger. If a Veteran believes his or her life or health is in danger or is experiencing a suicidal crisis, they are encouraged to call 911 or report to the nearest emergency department right away.
Veterans do not need to check with VA before calling for an ambulance or going to an emergency department. During a medical emergency, VA encourages all Veterans to seek immediate medical attention without delay. It is, however, important for you to promptly notify VA within 72 hours of a Veteran presenting to the your emergency room.
Emergency care during and after a suicidal crisis
Starting January 17, 2023, VA will pay for, provide or reimburse emergency care for certain Veterans and individuals – including ambulance transportation costs – and follow-on inpatient or residential care related to the event for up to 30 days, and outpatient care for up to 90 days, including social work.
Notification as soon as possible is imperative because VA must verify a Veteran’s eligibility for emergent suicide care if they are not already enrolled or registered with VA. You should also contact your local VA medical center (VAMC) to coordinate follow-on care and transfer activities, if necessary.
Phone numbers and email addresses to local VAMCs
Coordinating with VA prior to admitting a Veteran is key to improved care outcomes and patient satisfaction. VA will coordinate follow-on care or transportation to a VA facility when an inpatient bed is available.
Regardless of VA enrollment status, COMPACT-eligible individuals are:
- Former members of the armed forces who were discharged or released from active duty under conditions other than dishonorable after more than 24 months of active service.
- Former members of the armed forces, including reserve service members, who served more than 100 days under a combat exclusion or in support of a contingency operation either directly or by operating an unmanned aerial vehicle from another location who were discharged or released under a condition that is other than dishonorable.
- Former members of the armed forces who were the victim of a physical assault of a sexual nature, a battery of a sexual nature, or sexual harassment while serving in the armed forces.
72-Hour Notification
Veterans, their representatives, and in-network community providers should report instances of a Veteran presenting to a community emergency room to VA within 72 hours of the start of emergent care. Out-of-network providers are encouraged to notify VA as soon as possible.
Notifying VA in a timely fashion is important because this:
- Allows VA to assist the Veteran in coordinating necessary care or transfer,
- helps ensure that the administrative and clinical requirements for VA to pay for the care are met, and
- may impact a Veteran’s eligibility for VA to cover the cost of emergency treatment.
Case-specific details are necessary for care coordination and eligibility determinations. Providers, Veterans and representatives can utilize any one of the following options to report emergency services:
Online: Emergency Care Reporting
Phone: 844-72HRVHA (844-724-7842)
In-person: Appropriate VA official at the nearest VA medical facility
The person contacting VA should be prepared to supply the information shown in the table below. If the caller is unable to supply all information, VA will engage with the appropriate parties to attempt to collect the information.
| Veteran Information | Treating Facility Information |
|---|---|
| Name | National Provider Identifier (NPI) |
| Gender | Name |
| Social Security Number | Address |
| Date of Birth | Point of Contact (POC) Name |
| Veteran Address | POC Phone # |
| Date Presenting to Facility | POC Fax # |
| Date of Discharge | POC Email |
| Admitted? (Yes/No) | NOTE: POC will receive VA authorization decision information |
| Chief Complaint/Admission DX and/or Discharge DX | |
| Originating Location (address where the emergency event occurred) |
|
| Mode of Arrival | |
| Other Health Insurance |
The primary purpose of notifying VA of a Veteran in need of emergency treatment presenting to a community provider is to ensure proper care coordination. Notifying VA also allows covered Veterans to have their emergent treatment authorized by VA under Title 38 Code of Federal Regulation (CFR) §17.4020(c). The local VAMC will engage with community providers who report notification through the centralized notification process. However, if you have an urgent or emergent need to coordinate care and/or transfer a Veteran to a VAMC, please make immediate contact the nearest VAMC.
Facility Contact Numbers for Care Coordination
IMPORTANT: Failure to notify VA of care rendered through an in-network community facility in a timely manner prevents VA from authorizing the emergency care, and prevents claims and payments from being made through one of VA’s third-party administrators.
Veteran Eligibility for Emergency Care
VA has three legal authorities under which emergency treatment in a community facility may be paid for by VA:
- Authorized Emergency Treatment–Title 38 Code of Federal Regulations (CFR) §17.4020(c)
- Unauthorized Emergency Treatment (Service-connected)–Title 38 United States Code (U.S.C.) §1728
- Unauthorized Emergency Treatment (Nonservice-connected)–Title 38 U.S.C. §1725
Each authority requires the following General Eligibility requirements be met:
- Veteran is enrolled or exempt from enrollment in the VA health care system.
- A VA health care facility or other federal facility with the capability to provide the necessary emergency services must not have been feasibly available* to provide the emergent treatment and an attempt to use them beforehand would not be reasonable.
- The medical situation is of such a nature that a prudent layperson would reasonably expect that a delay in seeking immediate medical attention would be hazardous to life or health.
- Generally, emergency treatment is only covered until such time as the Veteran can be safely transferred to a VA or other federal facility. If the Veteran refuses to be transferred to a VA or other federal facility after their emergency condition is stabilized, they may be liable for the cost of care beyond the point of stabilization. VA Form 10-8001, Refusal of Transfer to VA Health Care Facility, is used when a Veteran refuses to transfer to a VA Health Care Facility.
Refusal of Transfer to VA Health Care Facility, VA Form 10-8001
The single exception to this rule is if VA is contacted and unable to accept the transfer. If this happens, it is important for the community emergency treatment facility to document any attempt to transfer the Veteran.
Additional Requirements for Authorized Emergency Treatment (Title 38 CFR §17.4020(c)):
In addition to the General Eligibility requirements, in order to be authorized for emergent care under Title 38 CFR
§17.4020(c), all of the following criteria must also be met:
- In-Network Status: The treatment was rendered at a community emergency facility that is in VA’s community care network.
- 72-Hour Notification to VA: VA must be notified of the treatment within 72 hours. If VA is not timely notified, the treatment cannot be authorized under this section.
Additional requirements for retroactive payment approval for unauthorized emergency treatment for service-connected Veterans (Title 38 U.S.C. §1728):
In addition to the General Eligibility requirements, for payment to be retroactively approved for emergent care under Title 38 U.S.C. §1728, one of the following criteria must also be met:
- Emergency treatment of a service-connected*, or adjunct condition* in a community emergency department; OR
- A Veteran who is permanently and totally disabled (P&T) as the result of a service-connected condition is eligible for emergency treatment of ANY condition; OR
- A Veteran who is participating in a VA Vocational Rehabilitation Program and requires emergency treatment to expedite their return to the program is eligible for emergency treatment for any condition.
NOTE: Legal authorities and payment methods for VA payment for emergency care of service-connected conditions are contained in Title 38 U.S.C. §1728, Title 38 CFR §17.120 and Title 38 CFR §17.132.
Additional requirements for retroactive payment approval for unauthorized emergency treatment for nonservice-connected Veterans (Title 38 U.S.C. §1725):
In addition to the General Eligibility requirements, for payment to be retroactively approved for emergent care under Title 38 U.S.C. §1725, all of the following 5 criteria must also be met:
- Care was provided in a hospital emergency department (or similar public facility held to provide emergency treatment to the public); AND
- The Veteran has received care within a VA facility during the 24 months before the emergency care; AND
- The Veteran is financially liable to the emergency treatment provider; AND
- If the treatment was due to an injury or accident, the claimant has exhausted, without success, all liability claims and remedies reasonably available to the Veteran or provider against a third party for payment of such treatment, and the Veteran has no contractual or legal recourse for extinguishing, in whole, the Veteran’s liability to the provider; AND
- The Veteran is not eligible for reimbursement under Title 38 U.S.C. §1728 for the emergency treatment.
There are limitations on VA’s ability to provide coverage when a Veteran has other health insurance (OHI). If a Veteran has OHI but the OHI does not fully cover the costs of treatment, VA may pay certain costs for which the Veteran is personally liable, unless payment by the Veteran’s OHI was barred because the Veteran or provider failed to comply with the provisions of that health plan contract or third party payer; for example, failure to submit a bill or medical records within specified time limits, or failure to exhaust appeals of the denial of payment.
NOTE: Legal authorities and VA payment methods for emergency care of nonservice-connected conditions are contained in Title 38 U.S.C. §1725 and Title 38 CFR §17.1000.
How Network Status Impacts Eligibility, Authorization and Claims Submission
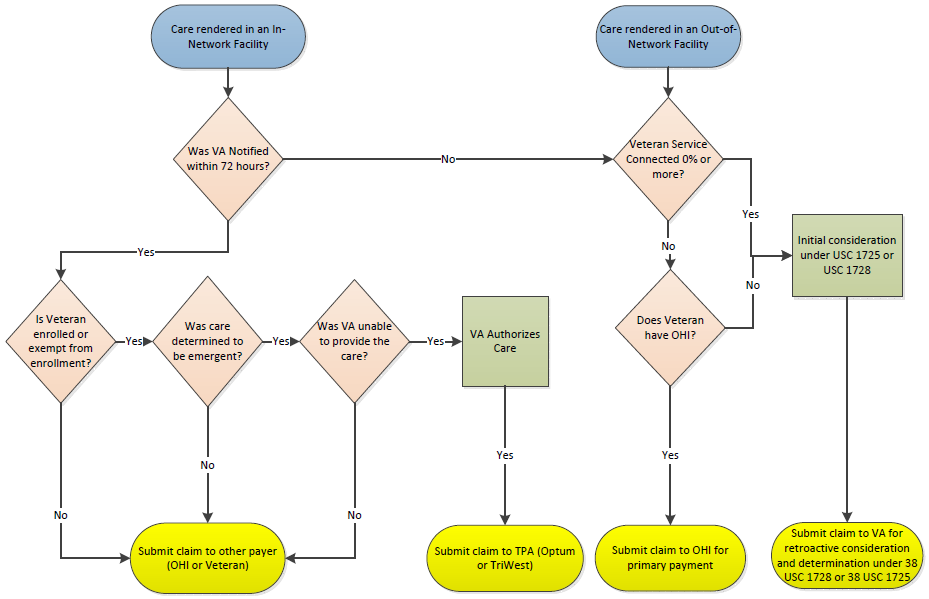
If care was rendered at an in-network facility and notification was received by VA within 72 hours, the following assessments will be made by VA:
Care At An In-Network Facility
- Is Veteran enrolled or exempt from enrollment?
- Was care determined to be emergent?
- Was VA unable to provide the care?
If the answer to all question is “Yes”, VA will authorize payment and the provider should submit claims to TPA (Optum or TriWest).
If the answer to any question is “No”, VA will not authorize payment and the provider should submit claims to another payer (OHI or Veteran).
If care was rendered in an in-network facility and notification was not received by VA within 72 hours, eligibility assessments will mirror those of an out-of-network facility (below).
Care At An Out-of-Network Facility
If care was rendered in an out-of-network facility the following assessments will be made by VA:
- Is Veteran service-connected 0% or more?
- If yes, initial consideration for payment approval will be under Title 38 U.S.C. §1725 and Title 38 U.S.C. §1728 and claims should be submitted to VA for retroactive evaluation and determination.
- If no, does the Veteran have other health insurance?
- If no, initial consideration for payment approval will be under Title 38 U.S.C. §1725 and U.S.C. §1728 and claims should be submitted to VA for retroactive evaluation and determination.
- If yes, claims should be submitted to other health insurance for primary payment.
Filing a Claim
File a Claim for Veteran Care
For information on how to file a claim and the timelines in which claims must be filed.
Supporting Documentation
It is essential that medical documentation and other supporting material for all care received by Veterans in the community is provided to the referring VA for incorporation into the Veteran’s electronic health records. Medical documentation is also an important component to assessing the patient’s condition and making determinations related to care coordination and eligibility. During the care coordination process, the local VA medical center will communicate with the community provider about information needed to support the coordination. There are multiple methods by which community providers may electronically provide the referring VA with the required medical documentation for care coordination purposes:
Veterans Health Information Exchange (VHIE)
VHIE enables bi-directional sharing of Veteran Health Information.
HealthShare Referral Manager (HSRM)
Utilize for referrals, authorizations and documentation exchange.
Azure Rights Management Services (Azure RMS)
Use for encrypted email.
E-fax: Documentation sent via email to Veterans Affairs Medical Center (VAMC) fax machine. Please contact the referring VAMC for e-fax number.
File a Claim for Veteran Care
For information on how to file documentation in support of a claim for reimbursement. Refer to the Supporting Documentation section.
Receiving Payment
VA and VA’s third-party administrators make every effort to adjudicate claims for emergency treatment quickly and accurately. When further information or clarification is needed, claims processing may be delayed.
If a Veteran is charged for emergency treatment received in the community and believes the charges should be covered by VA, they should contact the VA Office of Integrated Veteran Care (IVC) National Call Center. VA staff will assist the Veteran in understanding eligibility and determining whether the bill received is appropriate. VA will assist the Veteran and work to resolve any billing issues with the community provider.
VA IVC National Call Center: 877-881-7618, Monday-Friday, 8 a.m. to 8 p.m. Eastern Time
If you are a provider and have a question about a claim you have submitted for payment, please contact the entity to which the claim was submitted:
- TriWest: 855-722-2838
- VA: 877-881-7618
- Optum Region 1: 888-901-7407
- Optum Region 2: 844-839-6108
- Optum Region 3: 888-901-6613
Reimbursement Rates
| Type of Care | Reimbursement Rate | Emergent Care Payer |
|---|---|---|
| Authorized Emergency Treatment Title 38 CFR §17.4020(c) |
Generally, 100% Medicare (refer to the terms of your contract) |
Authorizing Third Party Administrator (Optum or TriWest) |
| Unauthorized Emergency Treatment (Service-connected) Title 38 USC §1728 |
Generally, 100% Medicare | VA |
| Unauthorized Emergency Treatment (Nonservice-connected) Title 38 USC §1725 |
Generally, 70% Medicare | VA |
Emergency Care in Foreign Countries
VA can pay for emergency medical care outside the United States if the emergency is related to a Veteran’s service-connected condition. Contact the Foreign Medical Program for more information.
Foreign Medical Program: 877-345-8179
Definitions
Adjunct condition: A condition that, while not directly service-connected, is medically considered to be aggravating a service-connected condition.
Prudent Layperson: Any medical or behavioral condition of recent onset and severity that would lead an individual who possesses an average knowledge of health and medicine to believe that his or her condition, sickness, or injury is of such a nature that failure to obtain immediate medical care could result in placing the health of the individual in serious jeopardy, serious impairment to bodily functions, or serious dysfunction of any bodily organ or part, or in the case of behavioral condition placing the health of such person or others in serious jeopardy. This prudent layperson definition of emergency medical condition focuses on the patient’s presenting symptoms rather than the final diagnosis when determining whether to authorize medical claims for payment
Service-connected Condition: A condition that has been adjudicated by the Veterans Benefits Administration (VBA) and granted a disability rating.
VA Feasibility: VA’s capability to provide the emergency services at the time a Veteran is in need of such services. Travel time to the nearest VA capable of servicing those emergent needs, the severity of symptoms and the mode of arrival will all be evaluated in assessing VA feasibility.
Resources
- Fact Sheet: Medical Documentation Submission Requirements for Care Coordination
- Fact Sheet: Centralized Community Emergency Treatment Reporting and Care Coordination
- Fact Sheet: Emergency Suicide Care and Treatment (Community Provider)
- Fact Sheet: VHA IVC Ambulance Transportation
- Optum Provider Portal
- TriWest Provider Portal
- VA Facility Locator



















